Occupational Noise Exposure in Relation to Hypertension: A Cross-sectional Study in the Steel Factory
Received: 07-Aug-2017 / Accepted Date: 20-Sep-2017 / Published Date: 05-Oct-2017 DOI: 10.4172/2329-6879.1000266
Abstract
Background: Noise has been acknowledged as one of the most prevailing physical hazard in occupational health and safety. Noise can possess both permanent and temporary health outcomes. The hazardous exposure to occupational noise is generally identified to have aural effects. However in past few years, researches have been carried out to perceive the association between noise exposure and cardiovascular diseases. Yet, the topic has been under controversies regarding its actual relationship or association since there is an existence of other confounders, variables or lifestyle with the exposure which might affect the subsequent disease condition. The results have not been consistent in the studies. Hypertension is one of the most significant etiological factors for cardiovascular diseases. Noise can cause high blood pressure mostly by two ways: either by releasing stress hormones like steroids or by stimulating sympathetic nervous system. China being one of the most rapidly developing countries in the world is having most prominent effect of noise in the daily life since it is a point for most of the goods manufacturing. Various national and international organizations like CDC, OSHA, and NIOSH etc. has recommended various ways to control the noise hazard and its deleterious impact on human health. This research was also done to assess the relationship or association between noise exposure level and prevalence of hypertension in the workers from steel factory in Guangzhou.
Aim: The goal of the study was to find out the relationship between occupational noise exposure and prevalence of hypertension regarding its confounders.
Methods: A cross-sectional study was carried out to find out the association between noise exposure level (<85, 85-90, >90) dBs and hypertension. The data was collected in Guangzhou No.12 Peoples hospital. A sample of 274 workers was taken from the steel factories in Guangzhou. The data was collected through physical examination and questionnaires. For statistical analysis, Chi square test was used in order to compare the variables. Logistic regression analysis was used to test the association between hypertension and the selected variables.
Results: As a result, we found out that cumulative noise exposure is associated with hypertension (P=0.004). The total prevalence of 9.8% of hypertension cases were under the noise exposure group of >90 db. The independent association of hypertension was seen after the linear regression analysis as BMI group over weight (odd ratio = -0.090, CI 95%= (-0.005)–(-4.280) with P=0.039 when compared to the reference category of BMI underweight. The correlation of hypertension was also seen with age group (P=0.009), working years and sleeping hours with P=0.030 and P=0.047 respectively.
Conclusion: The study showed that the prevalence of hypertension is associated with the occupational noise exposure and highly influenced by BMI group overweight after our final regression analysis. Age group, working years and sleeping hours also showed having some association with the prevalence of hypertension.
Keywords: Occupational noise; Hypertension; Cardiovascular disease; Non-auditory effect of noise
Introduction
Noise is any unwarranted disturbance within a useful frequency band (NIOSH, 1991) [1], and it has been identified as one of the most prevailing physical hazards in occupational health and safety of the expeditiously developing countries. Globally, noise now has been listed as the third epidemic to cause physiological and psychological dysfunctions after the other chronic diseases such as cancer and circulatory diseases and has proven to have calculable association among noises-aggregated health effects [2].
Noise can act as both physical and psychological impetus. Globally, about 600 million workers are exposed to occupational noise [3]. The World Health Organization estimated that about 250 million workers around the globe are exposed to potentially hazardous noise levels [1]. Listed as one of the most prevailing physical hazard, noise has variations in occurrence and is proven to be prominent causes for occupational related health outcomes. The noise impact can either endure temporary or permanent health impairments (auditory and non-auditory effect). The aftermath of the noise exposure is slow and elusive. Annoyance can have immediate result; detrimental health effect is seen only after persistent and recurring exposure to inimical noise.
Noise acts as stress arbitrator debilitating concentration and causes sleeping disorder affecting psychosocial aspect of the person with passive presentation in day to day activities [4]. Persistent exposure to occupational or environmental noise may induce various contrary health effects as sleep disturbance, annoyance, noise-induced hearing loss (NIHL), cardiovascular disease, endocrine effects, and elevated incidence of diabetes [5,6]. According to WHO, annually 45000 lives are lost due to noise-induced cognitive impairment in children, 903000 due to noise-induced sleep disturbance, 61000 due to noise-induced cardiovascular disease, and 22000 due to tinnitus in Western Europe [4]. In the States, 4 million of workers get exposed in the harmful noisy environment every day and approximately 10 million people have noise related hearing disorders or loss where 22 million of worker population is exposed to possibly damaging noise every year. About 82% of cases were reported in 2007 related to occupational hearing loss among workers in manufacturing sector.
Noise and hearing Impairment
Hearing loss occurs with continuous noise exposure and extent of exposure, which gradually progresses over years. Hearing loss due to continuous exposure to noise upsurges swiftly in period of first 5-10 years of noise exposure. The rate of hearing loss then decelerates as the hearing threshold increases. This is also contrast to age related hearing loss, which quickens over time [7]. The hazard of noise induced hearing loss is sensed to be low at exposure below 85 dB for 8 hours’ time-weighted on average, although it surges ominously as exposure upswing above this level [8]. Occupational noise is basically measured in A-weighted decibel (dB) A and the modest amount of exposure is 8 hours per working day. It has been proven that there is a strong association between the parameter and its potential of impairing human hearing. This is one of the most prevailing epidemiological measurements of exposure. Hearing impairment is one of the preeminent results of occupational noise exposure.
The primary effect of exposure to surplus noise usually upsurge in threshold of hearing (threshold shift) [1]. The acquaintance to loud sound in occupational setting causes generally two kinds of hearing sensitivity: a temporary threshold shift (TTS) in hearing sensitivity or permanent threshold shift (PTS). The temporary threshold shift in hearing sensitivity refers to the hearing loss which last for several hours (14 hours or longer in definite cases) and permanent threshold shift refers to sensitivity which is perpetual. Noise induced permanent threshold shift (NIPTS) is a permanent threshold shift which can be accredited to noise exposure [7]. Threshold shift is predecessor of noise induced hearing loss and tallies to permanent increase in threshold of hearing which might be escorted by tinnitus. The noise induced tinnitus may be for either short term (24 hours) or permanent after persistent noise exposure. Noise-induced hearing impairment occurs predominantly at higher frequencies (3000−6000 Hz), with the largest effect at 4000 Hz. It is irreversible and increases in severity with continued exposure.
Noise and psychology
Noise has various ranges of psychological outcomes. Several studies were done and as per epidemiological research most prevailing psychological noise aftermath comprises of annoyance, psychological well-being and psychiatric hospitalization [6]. The leading psychosocial effect from noise exposure and occupational noise exposure is annoyance. Association within noise and annoyance has been interpreted on population level composed with various effectalternating factors. Annoyance from uninterrupted sound seems to differ significantly by individual. There are also numerous factors that might stimulate annoyance and succeeding stress mechanism. Annoyance intensifies sympathetic stimuli specifically in noise sensitive individual, and might be the non-sleep intervened pathway that is existing in the individual with excessive occupational noise exposure who might consequently develop heart diseases. Epidemiological studies shows that annoyance in offices is considerable at equivalent sound levels >55 dB (A). A few studies show that 35-40% of office workers are highly annoyed at noise levels from 55 to 60 dB (A). In industrial situations, similar percentages of highly annoyed workers occur at equivalent sound levels >85 dB (A).
Noise-induced cardiovascular conditions
Cardiovascular system does not stand at first place when comes to the onset of diseases and hazards in occupational setting unless the pathogenesis is associated to stress-related disorders. Noise can be hazardous in several ways. As noise surges stress hormones such as cortisol, epinephrine and non-epinephrine which later may be the causes for the onset of high blood pressure, heart stroke and heart failure. The short-term laboratory research on human being and long standing research on animal have together delivered biological mechanism and creditability for the theory that long term exposure to environmental noise affects the cardiovascular system and roots manifest disorders like hypertension, ischemic heart disease and stroke [9].
There was increased risk of acute myocardial infraction mortality in the workers in sawmill who were exposure to higher occupational noise exposure [10]. Till date, cardiovascular diseases (CVD) have been often studied and reviewed for over past 40 years with conclusions as occupational noise contributes in elevation of blood pressure (BP), hypertension and other cardiovascular related diseases [11]. Repeated exposure to high intensity of noise in various working circumstances increases the risk of CVD with two folds. Among the exposure group, young aged smokers were at greater risk for CVD as it is one of the main causative agents for it [12]. CVD, being a primary causation for mortality globally, is also predicted to have greater impact and prevalence in coming decades [13-15].
Noise and hypertension
Hypertension (HTN) or high blood pressure is a prolonged medical status where the blood pressure in the arteries is raised persistently [16]. Hypertension was defined by the World Health Organization: a systolic BP ≥ 140 mmHg or a diastolic BP ≥ 90 mmHg, or had been treated for hypertension [17]. Hypertension is one of the significant causes for CVD. There are some modifiable components as eating habits, smoking and drinking habits, occupation and some nonmodifiable components as genetic deposition, age and gender are known for causing hypertension [18].
HTN is comparatively prevailing and acknowledged as one of the common health risk among workers exposed in loud noise [19]. There are two probable biological mechanisms for relationship between noise and high blood pressure; it can either because of release of stress hormones like steroids or by stimulation of sympathetic nervous system with release of adrenaline hormones. The pathophysiology of the noise to induce hypertension is hypothesized as involvement of dysfunctional stress mechanism.
The auditory system which is also related to sympathetic nervous system and neuroendocrine system reacts to the sound stimulus through reflexes which are evidenced by cardiovascular effects such as alteration in catecholamine, epinephrine and non-epinephrine, corticosteroids levels. The continuous exposure and repetition to the noise can be pathogenic, leading to persistent ascending of vascular auto regulation resulting to hypertension [20]. A study has showed that the levels of stress hormones like catecholamine and cortisol are higher in the in the exposure group than the non-exposure group [21]. While some research concentrated on the sympathetic medullary axis and demonstrated elevated heart rate and blood pressure [22]. Chronic exposure to occupational noise has proven for extorting hypertension according to many previous studies [23-28]. Elevated risk of hypertension was shown between the subject who were exposed to high level of noise for longer duration and after adjustment for age, race, working years gradual increase in risk of hypertension was shown with the cumulative noise exposure of 85 dB and above [29].
It has been shown that the industrial workers are at higher risk of stroke or CVD by 27% than the financial workers but non-significant with noise exposure level [30]. Various studies have shown that there is a connection between noise exposure and high blood pressure [31]. It has been shown that the long-term exposure to self-reported occupational noise exposure was related with approximately 3 folds rise in the prevalence of angina pectoris and 2 folds increase in prevalence of coronary heart disease (CHD) and isolated diastolic hypertension (IDH) [28]. Though there was no proven epidemiological reason for it. The confounders like lifestyle and hereditary factor are some additional factors that may give biased interpretation regarding the relationship [32].
Other factors likely to affect the blood pressure are shift work and workplace noise [33,34]. The association between shift works and noise exposure was given by Attarchi et al. which explained that the prevalence of hypertension and mean of systolic and diastolic blood pressure were relatively higher among the shift workers exposed in the noise above 84 dB [34]. Though, WHO in 1999 concluded that the current evidence offered weak correlation between long term exposure to noise above 67-70 dB and prevalence of high blood pressure [35]. Some of the present day studies have a call that noise exposure above 50 dB at night time may mark up the risk of myocardial infraction by enhancing the production of cortisol.
Meanwhile, China today is one of the rapidly developing countries in the globe. With maximum growth in its economy and standards, there has been a drastic modification of life style among the Chinese population. These modifications are having prominent effects with the noise exposure levels in daily life of Chinese population, weather it is at their workplace, transportation or leisure time activities or entertainments. Approximately, tens of millions of immigrant workers in China are into intense laboring in constructions and manufacturing exposing themselves to extraordinary level of noise compared to another working environment. As a result, the prevalence of noise induced adverse health effects are up surging [36]. There has been a rising interest on the aftermath of occupational noise exposure over health with the rapid industrialization in China.
Few recent studies and researches has concluded that noise pollution has been placed at 4th position to conduce sub-healthy state in the Chinese population summing with further factors such as inadequacy of rest and physical workouts, additional work shifts and air pollution [37]. The prevalence of hypertension and high blood pressure are also increasing with its rapid development. A study showed that 33.6% (35.3% in men and 32% in women) or 335.8 million (178.6 million men and 157.2 million women) of the Chinese adult population had hypertension in 2010 [38]. Since China is major country for most of the production of materials and part required by all over the world, we see a lot of large scale industries and factories, few of the studies done in different cities of China are given below for a brief acknowledgement of occupational noise and prevalence of hypertension in China.
A case–control study conducted in Hangzhou showed that there was a high risk of hypertension in the exposed group than in non-exposed group of study [39]. A research done in a Taiwan in an aircraft manufacturing plant showed that among 790 workers 141 were classified as hypertensive and 56 were further more diagnosed with hypertension in 10 years of study [25]. A study done among 3150 workers in a steel factory in Zhengzhou showed the prevalence of hypertension in 29.88% of male and 12.13% of female who were exposed to the cumulative noise exposure level of 95 dB to 113 dB [40,41]. A study conducted in a coal company in Nanjing with 738 participants showed the prevalence of hypertension in 29.2% of the workers who were exposed to the occupational noise [32].
Aims of the study
• To determine the relationship between occupational exposure to noise and hypertension.
• To investigate the prevalence of cardiovascular diseases related to occupational noise exposure.
Materials and Methods
Study population
The study was done at Guangzhou No.12 People’s Hospital, China. The samples of 274 were taken from the hospital database which was pre-collected through a questionnaire survey and physical examination. The study populations were from a steel factory in Guangzhou. The worker were from different department of the factory such as galvanized workshop, acid rolling line, equipment room, rolling operation, grinding machines etc. The inclusion criteria for the study population were:
• Participant with noise exposure more than one year (including one year)
• Noise exposure intensity larger than 80 dB (A).
• No family hereditary deafness, no external ear and middle ear disease, no detonation history, no history of head trauma.
• No ototoxic drug taking history (common ototoxic drugs are: streptomycin, gentamicin, kanamycin, vancomycin, quinine, aspirin, diuretics, anticancer drugs)
• No history of infection affecting the hearing function (may affect the hearing function of infectious diseases mumps, meningitis, brain, measles and rubella and other diseases);
• No family history of hypertension and other family history of cardiovascular disease.
Noise exposure assessment and frequency analysis: The noise exposure was assessed for 8 working hours. A portable noise measuring meter was used to determine the frequency of noise which was carried by each worker within their working hours. The noise exposure level in the factory was then classified into 3 categories: 90 dB. We took this level of exposure on the basis of few studies that used these levels for their studies [42].
Blood pressure measurement and hypertension: The systolic and diastolic blood pressures were obtained using a sphygmomanometer. The determination of hypertension in the study was the systolic blood pressure higher or equals to 140 mmHg and diastolic pressure higher than or equals to 90 mmHg. The blood pressure measurement was done by professional health workers in the hospital. The prehypertensive workers were identified through the questionnaire survey.
The questionnaire was developed to retrieve some general information of participants. It included the demographic data, personal (smoking habits, drinking habits, physical exercise, sleep duration, use of headphones and access to noise post work) and professional history (length of service, contact to noise throughout the service, daily and weekly exposure to noise, work shifts, use of PPE, exposure to high temperature, vibration, radiation, electromagnetic radiation, dust, organic solvent and heavy metals), past and present medical history, use of ototoxic drugs. Smoking habit was specified as no smoking and amount or frequency to smoking per day for last 6 months. Likewise, drinking habit was classified as per intake of more than one kind of liquor per week for more than 1 year. All the subjects filled out the questionnaire after giving informed consent and before a physical examination.
Statistical analysis
All the data were analyzed by SPSS version 21.0. We started with illustrating the frequency distribution of all variables according to the level of noise exposure. The bivariate analysis was done to test the association between the variables and exposure and outcome in order to identify the further potential confounders that can be associated to exposure. The normality of the variables was tested by Shapiro-Wilk considering the p-values >0.05 as a point to keep the hypothesis that the variable is normally distributed. For all the variables with normal distribution, we chose parametric test to acquire the correlation coefficient value i.e. Pearson’s correlation (r). For the variables which were not normally distributed we took the Spearman’s correlation coefficient value (Spearman’s rho). The variables were categorized and Chi-square was used to test the association and for the p-values bivariate correlation test was done. Next, the confounders with P value< 0.05 from Chi-square and correlation results were included into the generalized linear model. All the variables were individually tested for the association of noise with hypertension and were considered to be included in the regression analysis. The model was composed of confounders which were statistically significant i.e. P< 0.05. Regression analysis with linear regression was done to test the individual independent relation between the variables and high blood pressure. The ultimate odd ratio concluded the prevalence of hypertension.
Results
Total of 274 workers were incorporated in this study. Out of these 19/274 workers were found having high blood pressure after physical examination and history collection through the questionnaire.
Effect of age on hypertension: Only the male population was taken in the study since there were no female workers in this department of the factory. The age group was divided into 3 groups: <27, 27-30 and >30 with the mean age of 28.6 ± 4.23 years. The non-parametric correlation for age showed the rho value of 0.201 and P=0.001 (Table 1) showing the association although we took the parametric correlation for further analysis. Here we saw that hypertension is positively correlated with age of the workers. With the increase of age, the prevalence of hypertension was also increasing with the Chi square value χ2=0.32 and P=0.009.
| Continuous variables | Mean | Standard deviation | Correlation coefficient (Spearman’s rho) | p-values |
|---|---|---|---|---|
| Age | 28.62 | ± 4.23 | 0.201 | 0.001 |
| Working years | 4.69 | ± 2.86 | 0.131 | 0.03 |
| Cumulative noise exposure (CNE) | 91.77 | ± 3.64 | 0.216 | 0 |
| Systolic blood pressure(SBP) | 122.02 | ± 11.68 | r=0.391 | 0 |
| Diastolic blood pressure (DBP) | 77.05 | ± 8.34 | 0.271 | 0 |
| Body mass index (BMI) | 22.8 | ± 3.1 | 0.195 | 0.001 |
| Sleeping hours | 7.68 | ± 1.15 | -0.1 | 0.047 |
*r=Pearson’s correlation coefficient
Table 1: Statistics for continuous data.
Effect of noise exposure duration on hypertension: The noise exposure duration was taken in terms of working years, daily noise exposure and weekly noise exposure. The sample group taken had 1 year of minimum and 17 years of maximum working duration in the factory with the mean working years of 4.69 ± 2.86 years (Table 1). The mean daily noise exposure hours of the workers was 1 hour at minimum and 12 hours at maximum a day with mean noise exposure hours of 10.24 ± 3.23 hours per day. Likewise, the workers were exposed to the noise for maximum of 6 days and minimum of 3 day per week with the mean weekly exposure of 4.23 ± 0.72 days a week.
The duration of noise exposure (per day and week) did not seem to have any relation with the prevalence of hypertension in our study as the correlation coefficient for daily noise exposure was 0.073 with P=0.230 and for weekly noise exposure the correlation coefficient was 0.037 with P=0.54. But the working year showed having correlation with hypertension with Spearman’s rho=0.131 and P=0.030 (Table 1).
Effect of cumulative noise exposure (CNE) on hypertension: The mean cumulative noise exposure in this study was 91.77 dB ± 3.64, with Spearman’s rho value 0.201 and P=0.001 (Tables 1 and 2), which showed that hypertension was related to the cumulative noise exposure. The cumulative noise exposure groups were divided into 3 categories: <85, 85-90 and <90 dB of noise. Ongoing into the relationship between cumulative noise exposure and hypertension, we found out that the noise exposure at <85 dB and 85-90 dB had no significance of hypertension but as the noise exposure level increases to >90 dB, we saw that 19(9.8%) workers of 274 workers were having hypertension (Table 3). Hence it was found out that cumulative noise exposure group was having association with hypertension with derived Chi square value 0.015, and P=0.005 showing the significance relationship (Table 3).
| Variables | CNE groups | P-value | ||
|---|---|---|---|---|
| <85 | 85-90 | >90 | ||
| n=6 | n=74 | n=194 | ||
| Age group | ||||
| <27 | 3 (3.2%) | 3 (3.4%) | 0 | |
| 27-30 | 30 (32.3%) | 25 (28.1%) | 19 (20.7%) | P=0.13 |
| >30 | 60(64.5%) | 61 (68.5%) | 73 (79.3%) | |
| Use of PPE | ||||
| Never wear | 0 | 4 (21.1%) | 15 (78.9%) | |
| Occasionally wear | 5 (3.6%) | 32 (23.4%) | 100 (73%) | |
| Regular wear | 1 (1.4%) | 27 (37%) | 45 (61.6%) | P=0.80 |
| Almost every time | 0 | 11 (24.4%) | 34 (75.6%) | |
| Smoker | ||||
| No smoking | 3(2.1%) | 42 (29.2%) | 99(68.8%) | |
| 1-10/day | 1 (1.3%) | 22 (29.3%) | 52 (69.3%) | |
| 11-20/day | 2(4.1%) | 8(16.3%) | 39 (79.6%) | P=0.77 |
| 21-40/day | 0 | 1 (25%) | 3 (75%) | |
| >40/day | 0 | 1 (50%) | 1(50%) | |
| Alcohol frequency | ||||
| < 1 time/week | 5 (3.2%) | 41 (26.3%) | 110 (70.5%) | |
| 1 time/week | 0 | 22 (24.7%) | 67 (75.3%) | |
| 2-3 times/week | 0 | 9 (37.5%) | 15 (62.5%) | P=0.34 |
| 4-5 times/week | 0 | 2 (50%) | 0 | |
| 5 times/week | 1 (100%) | 0 | 0 | |
| Physical exercise | ||||
| Never exercise | 0 | 25 (39.7%) | 38 (60.3%) | |
| 1-2 time/week | 5 (2.8%) | 42 (23.7%) | 130 (73.4%) | P=0.139 |
| 3-5 times/week | 1 (3.4%) | 7 (24.1%) | 21 (72.4%) | |
| 6 and above/week | 0 | 0 | 5 (100) | |
| BMI group | ||||
| Under weight | 2(9.5%) | 6(28.6%) | 13(61.9%) | |
| Normal weight | 2(1.6%) | 37(30.3%) | 83(68%) | P=0.149 |
| Over weight | 1(1.4%) | 16(22.2%) | 55(76.4%) | |
| Obese | 1(1.7%) | 15(25.4%) | 43(72.9%) | |
| Hypertension | ||||
| No | 6 (2.4%) | 74(29%) | 175 (68.6%) | P=0.01** |
| Yes | 0 | 0 | 19 (100%) | |
| Education | ||||
| Primary and below | 2(1.8%) | 30(26.8%) | 80(71.4%) | |
| Junior high school | 4(2.5%) | 44(27.2%) | 114(70.4%) | P=0.92 |
| Cardiovascular symptoms High blood pressure | ||||
| No | 6(2.2%) | 72(26.8%) | 191(71%) | P=0.77 |
| Yes | 0 | 2(40%) | 3 (60%) | |
| Palpitation | ||||
| No | 6(2.3%) | 71(27.3%) | 3(21.4%) | P=0.73 |
| Yes | 0 | 3(21.4%) | 11(78.6%) | |
| Heart rate change | ||||
| No | 6(2.3%) | 72 (27.1%) | 188(75%) | P=0.89 |
| Yes | 0 | 2(25%) | 6(75%) | |
Table 2: General characteristics of variables with cumulative noise exposure group.
| Variables | Hypertensive | Normotensive | p-value |
|---|---|---|---|
| n (%) | n (%) | ||
| n- 19 | n- 255 | ||
| CNE group | |||
| <85 | 0 | 6(100%) | χ2 =0.15 |
| 85-90 | 0 | 74(100%) | r=-o.14, P=0.005** |
| >90 | 19(9.8%) | 175(90.2%) | |
| Age group | |||
| <27 | 2 (2.2%) | 91 (97.8) | |
| 27-30 | 6 (6.7%) | 83 (83.3%) | χ2 =.032 |
| >30 | 11 (12%) | 81 (88%) | r=.159, P=0.009** |
| Use of PPE | |||
| Never | 2(10.5%) | 17(89.5%) | χ2 = 2.44 |
| Occasionally | 9(6.6%) | 128(93.4%) | Rho=.008 |
| Regular wear | 3(4.1%) | 70(95.9%) | P=0.901 |
| Almost every time | 5(11.1%) | 40(89.9%) | |
| Smoker | |||
| No smoking | 6 (4.2%) | 138 (95.8%) | |
| 1-10/day | 10 (13.3%) | 65 (86.7%) | |
| 11-20/day | 3 (6.1%) | 46 (93.9%) | χ2=0.152 |
| 21-40/day | 0 | 4 (100%) | r=0.075 P=0.218 |
| >40/day | 0 | 2 (100%) | |
| Alcohol frequency | |||
| <1 time/week | 7 (4.5%) | 149 (95.5%) | |
| 1 time/week | 8 (9%) | 81 (91%) | |
| 2-3 times/week | 4 (16.7%) | 20 (83.3%) | χ2=0.240 |
| 4-5 times/week | 0 | 4 (100%) | r=0.118, P=0.051 |
| 5 times/week | 0 | 1 (100%) | |
| Physical Exercise | |||
| Never exercise | 3 (4.8%) | 60 (95.2%) | |
| 1-2 times/week | 15 (8.5%) | 162 (91.5%) | χ2=0.474 |
| 3-5 times/week | 1 (3.4%) | 28 (96.6%) | r=0.004, P=0.948 |
| 6 and above | 0 | 5 (100%) | |
| BMI group | |||
| underweight | 0 | 21 (8.2%) | |
| Normal weight | 5 (26.3%) | 117 (45.9%) | χ2=0.024 |
| Over weight | 5 (26.3%) | 67(26.3%) | r=0.179, P=0.003** |
| Obese | 9(47.4%) | 50(19.6%) | |
| Education | |||
| Primary and below | 11 (9.8%) | 101 (90.2%) | |
| Junior high school | 8 (4.9%) | 155 (95.1%) | χ2=0.118 |
| High or secondary school | 0 | 0 | r=-0.037, P=0.540 |
| University | 0 | 0 | |
| Cardiovascular symptoms | |||
| Palpitation | |||
| Yes | 19 (7.3%) | 241 (92.7%) | χ2=0.611 |
| No | 0 | 19 (100%) | r=0.063, P=0.0296 |
| Heart rate change | |||
| Yes | 19 (7.1%) | 247 (92.9%) | χ2=0.938 |
| No | 0 | 8 (100%) | r=-.047, P=0.435 |
| High blood pressure | |||
| Yes | 19 (7.1%) | 250 (92.9%) | χ2=1 |
| No | 0 | 5 (100%) | r=-0.037, P=0.540 |
Table 3: Association between variables and hypertension.
Effect of body mass index on hypertension: The body mass index (BMI) was calculated by dividing the body mass by square of body height, mass in kilogram and height in meters. The standard interpretation of body mass index was taken as the reference such as BMI underweight (<18.5), normal weight (18.5-23), overweight (23- <25) and obese (>25). The calculated mean BMI was 22.87 ± 3.1 (Table 1). However we took BMI group to include in the further correlation analysis. The Chi square value was 0.024, Pearson’s correlation value 0.179 and P=0.003 which is <0.05. Therefore, as per the significance value, we found that the BMI has positive association with prevalence of hypertension on the workers. When included in regression analysis, it was shown that the BMI over weight was independently associated with prevalence of hypertension among the factory workers with odd ratio (-0.005)-4.280 with P=0.039 (Table 4).
| Variable | Odd Ratio | Confidence Interval (CI-95%) | Sig |
|---|---|---|---|
| Body mass Index | |||
| Underweight | -0.117 | 0.065-(-0.24) | 0.73 |
| Normal Weight | -0.101 | (-0.177)-(-0.024) | 0.1 |
| Over weight | -0.09 | (-0.005) - (-0.024) | 0.03** |
| Obese | 1 (Ref) | ||
| *controlled for BMI group, age group and CNE group | |||
Table 4: Odd ratio of hypertension among the body mass index (BMI) group.
Effect of sleeping hours on hypertension: Sleeping hour’s data was collected through the questionnaire. The minimum and maximum sleeping hour recorded were 5 hours and 12 hours respectively. The calculated mean for this was 7.68 ± 1.15. The P value of sleeping hours in relation to hypertension was 0.04 (Table 1). As this value fulfilled the significance value we saw that sleeping hours also had relation with the hypertension prevalence in the study.
Discussion
Although there is a considerable part of literature nowadays linking environmental noise exposure with hypertension and consequently with other cardiovascular disease, the results, however are inconclusive. In many cases, they considered to be supportive rather than definite due to failure to reach the level of statistical significance [43]. Furthermore, there is a certain degree of heterogeneity among studies regarding the age, gender, mean of assessment/measurement of exposure, duration of exposure, and sound level used, leading to mixed results [44,45]. Here in this study, we found out an association between Body Mass Index group overweight and hypertension. We also saw that age and cumulative noise exposures can also have influence for the prevalence of hypertension as 9.8% of the total case was under the CNE group >90 dB and with the increase in age group the prevalence of hypertension was also increasing. Our hypothesis has been not accepted that the noise exposure level is independently associated with hypertension and unlike few other we found no association between smoking alcohol drinking habits, use of personal protective equipment with hypertension. Likewise, comparing it to similar other researches, we saw similar kind of effects of noise level, age group, BMI and other confounding upon hypertension.
A study carried out in of the steel factory Henan province, China showed that cumulative noise exposure, alcohol consumption and BMI more than normal may affect the hypertension prevalence rate of the workers exposed to noise. Here the cumulative noise exposure level was taken as 95-99,100-104 and 105-113 dB with OR (95%CI) 1.84(95%CI: 1.35-2.51), 1.74(95%CI:1.24-2.45) and 1.68 (95%CI: 1.09-2.58), drinking (OR=1.60, 95%CI: 1.32-1.95) and BMI ≥ 24.0 kg/m2 (OR=1.26, 95%CI: 1.22-1.30), but in this study we found out that the cumulative noise exposure and age group are correlated with hypertension but doesn’t have independent association with hypertension. Although this study supports our result that BMI group of overweight is independently associated with prevalence of hypertension. A study done in Finland also suggested that the work load and occupational noise is responsible for the increased risk of coronary heart disease due to increased blood pressure, BMI and glucose level [46]. A multivariate analysis in a study publicized that age, body mass index, cumulative noise exposure, current antihypertensive medication and alcohol intake were the significant predictors for systolic blood pressure [47].
There are enormous health effects from the noise in the daylight, the noise exposure during night also have some significance health consequences. According to WHO, NNG (Noise Guideline for Europe) has given the association between night noise exposure and health effects in various 4 range of noise exposure level i.e. the noise exposure below 30 dB has no significant health effects. From 30-40 dB, it initially influences the sleep and has some contrary effects in the vulnerable groups. The exposure to 40-55 dB shows acute rise in adverse health consequences and also the vulnerable groups inclines to be intensely affected. The upsurge of the noise level above 55 dB has recurrent contrary health outcomes with elevated per centum of annoyance in huge population group [46,48]. A cross-sectional study carried out in one of the screw manufacturing factory in Taiwan with 188 male workers showed that the noise exposure of ≥ 80 dB for 2–4 years have a higher risk of hypertension. Exposure to the noise ≥ 70 dB at 4000 Hz for 2–4 years is associated with hypertension considering the inverse of noise frequency component on high blood pressure [49]. Various researches has found out that the occupational noise exposure was marked from <45 dB [50] >95 dB [51,52]. When we compared these studies with our study, we saw that we could not prove that noise exposure of <85 dB, 85-90 dB and >90 dB are independently associated with hypertension but they are correlated with each other. Most of the prevailing risk factors for the cardiovascular disease are age, gender, tobacco, smoking and drinking habit, inadequate physical activity, elevated blood pressure and cholesterol level and low socio-economic state. Most of these factors are related to occupational noise exposure [53].
A population of 432 exposed to the occupational noise exposure >85 dB showed that the relationship of age, body mass index and alcohol intake was significant to prevalence of high blood pressure [54]. A research talking about the related with noise vulnerability at working environment shows inadequateness of these covariate data confines the possibility to regulate the confounding factors in the researches. Hence, partial adjustment of the confounders may conclude to overestimation of the CVD effects of cardiovascular diseases only. 27% of industrial workers are at elevated risk of it than that of the financial sector workers but not indicatively by noise [30]. A research conducted in Hangzhou, China in order to determine the relationship of systolic blood pressure and diastolic blood pressure in regards with case group of 1390 workers exposed to occupational noise and 1399 workers in the control group of non-exposure group to occupational noise which concluded that there is an correlation and dose-response relationship between occupational noise exposure and elevated systolic and diastolic blood pressure and risk of prevalence of hypertension [39].
A study carried out in Japanese blue collar male workers working in the paper manufacturing factory to find the similar relationship between occupational noise and hypertension. Here in this study, two groups were taken one exposed with occupational noise in paper manufacturing plant (242 workers) and one group (173) from chemical plan without noise exposure. They showed that 16.9% of hypertension was prevalent in the noise exposed group whereas 34.7% of hypertension was found in the group without noise exposure. We saw the reverse relationship between noise and hypertension in this study since the workers were under the implication of guidelines for occupational noise management which might have prevented the workers from the contrary effect on noise on health. Unlike in our study, we saw no relationship between noise and use of PPE [55]. Another cross-sectional study done to determine the status and influence of hypertension on mechanic factory workers in Hunan provenience of China also enclosed that the hypertension prevalence was 12.1%. Logistic regression analysis showed the body weight index (BMI), age, and history of hypertension in parents and accumulative noise dose levels influenced the hypertension prevalence [56].
The developed countries have taken up different effective ways to prevent the adverse effect of occupational noise on health. Many scientific studies have been carried out to find out the adverse effects of noise and also different actions have been taken for the health promotion to subdue the contradiction made by occupational noise. Media communication has been proven to be most effective way for spreading the awareness in public. Rules and regulations have been taken up to defy all the adverse health effects of noise and is under strict evaluation under the government (for e.g.) Occupational Safety and Health Administration (OSHA) in the U.S.A created in 1971. Its mission is to prevent work related injuries, illnesses, and deaths among workers " OSHA's mission is to assure the safety and health of America's workers by setting and enforcing standards; providing training, outreach, and education; establishing partnerships; and encouraging continual improvement in workplace safety and health" (OSHA, 2004). With the foundation of OSHA, the occupational mortality rate has reduced by 62% and the injuries reports by 42%. Meanwhile, regarding the occupational health status of developing countries is prevailing behind due to lack of proper adoption of rules and regulations and awareness [57].
A study done in Amsterdam showed that there is a definite relation between noise and hearing loss but the relationship with noise and hypertension could not be evaluated after the adjustments of the confounding factors, also quoted that noise brings up various other non-auditory effects such as annoyance, irritation, impairment of communication and perception due to the stress causation due to noise [58]. A cross-sectional study carried out in the blue-collar worker demonstrated a potent relationship between noise exposure with hearing loss as well as hypertension with hearing loss greater than or equal to 65 dB loss at 3, 4, or 6 k Hz and high blood pressure greater than or equal to 90 mmHg diastolic or taking blood pressure medication in the 56+ age group [59]. The studies have shown that occupational noise not only results for hearing disorders or cardiovascular disorders but also causes the agitation in autonomic nervous system as well as endocrine system [60]. A study done in sack factory concluded that the occupational noise exposure has no significant in the rise of diastolic blood pressure but increased the systolic blood pressure, also indicating that the works should not be exposed to more than 89 dB of sound [61].
The researchers have found out that there are some genetic and environmental interaction between the angiotensin and chronic noise exposure resulting in hypertension [62]. Though there exist variation and contradiction in the findings of studies. This might be because the studies and researches consist of various study designs, alterations in exposure assessment, use and nature of personal protective equipment at occupation, diverse unit of capacity to regulate or control for confounders [63].
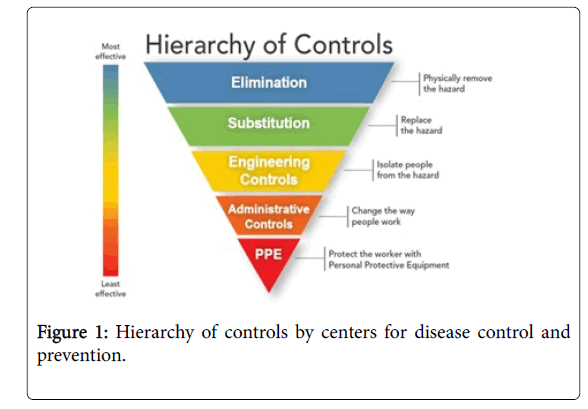
The hierarchy of control: Since occupational noise exposure has enormous health hazards, management of these hazards is mandatory. The occupational safety and health professionals from The Centers for Disease control and Prevention has then formed a Hierarchy of Control to control the hazard and reduce the risk of adverse health effects. This group strategically ramifies to degrade or withdraw the noise exposure and hazards. In the general cases, this helps to route away or eliminate the source of noise hazards. If elimination is not feasible, there is an alternative for substitution of those resounding equipment with nominal sound producing equipment. The next level of control in the hierarchy is engineering control. This control strategy is used when the substitution control fails to execute the hazardous occupational noise. Engineering controls necessitate physical alterations of workplace like reprogramming of the equipment in order to eliminate and obstruct the noise root reaching to the workers. If the hindrance of sound hazards is not viable by elimination, substitution and engineering controls, the consecutive control to be used is the administrative controls. This control group involves the alternating way of how workers would work or change their duty shifts in order to escape the long term noise exposure. At last we see the least effective level of control is the use of personal protective equipment (PPE) as they depend on the workers drive whether to use it or not. The use of PPE would give protection to the workers when it is interfused with other control group like administrative controls and when the noise is not completely removed by engineering controls (Figure 1) [31].
Source: The centers for disease control and collection prevention, 2016. Meanwhile in China, the government and the organizations has conducted substantial scale occupational hazard monitoring census, epidemiological surveys for the baseline information for further more development of occupational disease and forming new policies. China has adopted various steps in order to degrade the prevailing occupational health diseases. Yet, it needs to strengthen its policies, supervision and management to meet the demand of growing problems and population especially in the large scale industries and chemical factories. Occupational health standards system in China comprehends of extends including physical, chemical, biological, ergonomics and atmospheric condition at the working surrounding. The occupational health standards in China is mainly branched into imperative National Standards (GBZ) and recommended National standards (GBZ/T) that comprises of hygienic design of industrial enterprises, exposure limit of occupational hazards in the working environment diagnosis of occupational disease, warning signs of occupational hazards in the working place and technical specifications for occupational health and surveillance.
Limitation
Though we were able of complete this research fruitful relatively, we still had some confinements during the research listed below:
• The information we had for this research was from the physical assessment carried out for the works in the hospital in general basis hence there lacked quality regulations as this research had very limited time to carry out.
• The 19 workers out of 274 were categorized as hypertensive grounded on a blood pressure measurement taken during their assessment only. This way, the selection bias might have formed also the workers might have misclassified with diagnosis or treatment.
• As we have used the cross-sectional study design to see the correlation between hypertension and occupational noise exposure in this study, but this study design doesn’t assure that the outcome is actually an effect of exposure, to approve cause-effect relationship.
• It is uncertain that the workers primarily had hypertension was deliberately allotted to the work setting with greater noise exposure environment.
• Several studies have shown that the use of personal protective equipment would have association with hypertension but in this study we did not find any relationship of PPE with noise exposure and hypertension, so we did lack the précised evidence about use PPE.
• The sample size from this factory is relatively low in comparison with other studies, hence further addition of data and analysis needs to carry out. We also not clearly state that the BMI is highly associated with the prevalence of hypertension as the confidence interval was very high. Therefore, deeper study needs to be carried out with inclusion of some more sample size.
Conclusion
We found out that hypertension is co-related with noise exposure, age and BMI regarding the confounders. We saw that working year and sleeping hours also had relationship with hypertension. However, an independent association of hypertension was seen with BMI group over weight only. The main idea of this study was to support the hypothesis that the noise exposure is independently associated with hypertension, but we only saw there was correlation between the parameters. Even though we have many limitations in our study, we can still get some picture of associations between the noise exposure and prevalence of hypertension. Although there has been proven and well accepted relationship between noise induced hearing loss and noise exposure, the relationship between noise exposure and cardiovascular disease is still under argumentations. The research further might help for further limiting the hazard exposure and to spread the precautions as a part of public health studies. This study would contribute to the currently ongoing other similar study to fight the risk of this non communicable disease.
References
- Concha BM, Campbell LD, Steenland K (2004) Occupational noise, in assessing the burden of disease from work-related hearing impairment at national and local levels, WHO Protection of the Human Environment, Geneva.
- Yuen FK (2014) A vision of the environmental and occupational noise pollution in Malaysia. Noise Health 16: 427-436.
- Occupational Noise and Health, in Health and Safety Middle East: Published: 2012
- World Health Organization (WHO) (2011) Regional Office for Europe, Burden of disease from environmental noise, in Quantification of healthy life years lost in Europe.
- Hammer MS, Swinburn TK, Neitzel RL (2014) Environmental noise pollution in the United States:Â Developing an effective public health response. EHP 122: 115-119.
- Passchier VW, Passchier WF (2000) Noise exposure and public health. EHP 108: 123-131.
- Kirchner DB, Evenson E, Dobie RA, Rabinowitz P, Crawford J, et al. (2012) Occupational noise-induced hearing loss. JOEM 54: 106-108.
- ANSI ( 1996) Determination of Occupational Noise Exposure and Estimation of Noise-Induced Hearing Impairment (NIHL) and S3.44, Editors. ASA .
- Babisch W (2011) Cardiovascular effects of noise. Noise Health 13: 201-204.
- Davies HW, Teschke K, Kennedy SM, Murray RH , Hertzman C, et al. (2005) Occupational exposure to noise and mortality from acute myocardial infarction. Epidemiology 16: 25-32.
- Skogstad M, Johannessen HA, Tynes T, Mehlum IS, et al. (2016) Systematic review of the cardiovascular effects of occupational noise. Occupational Medicine 66:10-16.
- Reinberg S Workplace noise tied to heart disease risk. Health Day Reporter.
- Li N, Liu F, Song L, Zhang P, Qiao M, et al. (2014) The effects of early life Pb exposure on the expression of IL1-β, TNF-α and Aβ in cerebral cortex of mouse pups. J Trace Elem Med Biol 28: 100-104.
- World Health Organization (WHO). (2013)A global brief on hypertension: silent killer, global public health crisis, Geneva.
- Dzhambov AM, Dimitrova DD (2016) Heart disease attributed to occupational noise, vibration and other co-exposure: Self-reported population-based survey among Bulgarian workers. Med Pr 67: 435-445.
- Andren L, Hansson L, Bjorkman M (1981) Haemodynamic effects of noise exposure before and after beta 1-selective and non-selective beta-adrenoceptor blockade in patients with essential hypertension. Clin Sci (Lond) 61: 89-91.
- Kaplans NM (2002) Kaplan’s Clinical Hypertension. (8th Edn.), Lippincott Williams & Wilkins, Philadelphia.
- Sakata K, Suwazono Y, Harada H, Okubo Y, Kobayashi E, Nogawa K (2003) The relationship between shift work and the onset of hypertension in male Japanese workers. J Occup Environ Med 45: 1002-1006.
- Babisch W (1998) Epidemiological studies of the cardiovascular effects of occupational noise – a critical appraisal. J Occup Environ Med 1: 24-39.
- Sudo A, Nguyen AL, Jonai H, Matsuda S, Villanueva MB, et al. (1996) Effects of earplugs on catecholamine and cortisol excretion in noise-exposed textile workers. Ind Health 34: 279-286.
- Green MS, Schwartz K, Harari G, Najenson T (1991) Industrial noise exposure and ambulatory blood pressure and heart rate. J Occup Med 33: 879-83.
- Rhee MY, Kim HY, Roh SC, Kim HJ, Kwon HJ (2008) The effects of chronic exposure to aircraft noise on the prevalence of hypertension. Hypertens Res 31: 641-647.
- Weinmann T, Ehrenstein V, Von Kries R, Nowak D, Radon K ( 2012) Subjective and objective personal noise exposure and hypertension: an epidemiologic approach. Int Arch Occup Environ Health 85: 363-371.
- Chang TY, Hwang FB, Liu SC, Chen YR, Wang SV, et al. (2013) Occupational noise exposure and incident hypertension in men: a prospective cohort study. Am J Epidemiol. 177: 818-825.
- Rosenlund M, Berglind N, Pershagen G, Jarup L, Bluhm G (2001) Increased prevalence of hypertension in a population exposed to aircraft noise. Occup Environ Med 58:769-773.
- Bodin T, Maria A, Ardo J, Stroh E, Bjork J, et al. ( 2009) Road traffic noise and hypertension: results from a cross-sectional public health survey in southern Sweden. Environ Health 8: 38.
- Gan WQ, Davies HW, Demers PA (2011) Exposure to occupational noise and cardiovascular disease in the United States: the National Health and Nutrition Examination Survey 1999-2004. Occup Environ Med 68: 183-190.
- Sbihi H, Davies HW, Demers PA (2008) Hypertension in noise-exposed sawmill workers: a cohort study. Occup Environ Med 65: 643-646.
- Stokholm ZA, Bonde JP, Christensen KL, Hansen AM, et al. ( 2013) Occupational noise exposure and the risk of stroke. Stroke 44: 3214-3216.
- National Institute for Occupational Safety and Health Division of Applied Research and Technology (DART) December 2.
- Jing L, Ming X, Lu D, Hengdong Z, Liping P, et al. (2016) Prevalence of hypertension and noise-induced hearing loss in Chinese coal miners. JTD 8: 422-429.
- Rosenstock L, Mark C, Brodkin C, Redlich C (2004)Textbook of clinical occupational and environmental medicine., Elsevier Saunders: Philadelphia.
- Attarchi M, Dehghan F, Safakhah F, Nojomi M, Mohammadi S (2012) Effect of exposure to occupational noise and shift working on blood pressure in rubber manufacturing company workers. Ind Health 50: 205-213.
- Berglund B, Lindvall T, Dietrich HS (1999) World Health Organization (WHO): Guidelines for Community Noise.
- Yongbing S, Martin H, Willium (2013) Noise induced hearing loss in China: A potentially costly public health issue. J Otol 8: 51-56.
- Xie YM, Liu BY, Piao HY (2006) Exploration on the common characters of sub-healthy people based on clinical epidemiology. Zhongguo Zhong Xi Yi Jie He Za Zhi 26: 612-616.
- Bundy JD and He J (2016) Hypertension and related cardiovascular disease burden in China. Ann Glob Health 82: 227-233.
- Chen S, Ni Y, Zhang L, Kong L, Lu L (2017) Noise exposure in occupational setting associated with elevated blood pressure in China. BMC Public Health 17: 107.
- Li Y, Chen G, Yu S (2015) Prevalence and influence factors of hypertension among the workers exposed to noise in steel making and steel rolling workshop of an iron and steel plant. China J Prev Med 49: 5.
- Tanaka M, Shimal S, Nakamura K, Takahashl H, Tanaka K (1992) Investigation of noise in a factory. Ann Physiol Anthropol 11: 21-27.
- Ndrepepa A and Twardella D (2011) Relationship between noise annoyance from road traffic noise and cardiovascular diseases: a meta-analysis. Noise Health 13: 251-259.
- Munzel T, Gori T, Babisch W, Mathias B (2014) Cardio vascular effects of environmental noise exposure. Eur Heart J 35: 829-836.
- Kulbe JR, Mulcahy Levy JM, Coultrap SJ, Thorburn A, Bayer KU (2014) Excitotoxic glutamate insults block autophagic flux in hippocampal neurons. Brain Res 1542: 12-19.
- Koskinen HL, Kauppinen T, Tenkanen L (2011) Dual role of physical workload and occupational noise in the association of the metabolic syndrome with risk of coronary heart disease: Findings from the Helsinki Heart Study. Occupat Environ Medi 68: 666-673.
- Talbott EO, Gibson LB, Burks A, Engberg R, McHugh KP (1999) Evidence for a dose-response relationship between occupational noise and blood pressure. Arch Environ Health 54: 71-78.
- Hume K (2010) Sleep disturbance due to noise: Current issues and future research. Noise Health 12: 70-76.
- Chang TY, Liu CS, Young LH, Wang VS, Jian SE, et al. (2012) Noise frequency components and the prevalence of hypertension in workers. Sci Total Environ 416: 89-96.
- Belojevic GA, Jakovljevic BD, Stojanov VJ, Slepcevic VZ, Paunovic KZ (2008) Nighttime road-traffic noise and arterial hypertension in an urban population. Hypertens Res 31: 775-781.
- Davies HW, Teschke K, Kennedy SM, Hodgson MR, Hertzman C, et al. (2005) Occupational exposure to noise and mortality from acute myocardial infarction. Epidemiology 16: 25-32.
- Lyzwinski LN (2014) Public health perspectives on noise and cardiovascular disease. WJCD 04: 23-34.
- Agrawal Y, Niparko JK, Dobie RA (2010) Estimating the effect of occupational noise exposure on hearing thresholds: the importance of adjusting for confounding variables. Ear Hear 31: 234-237.
- Lang T, Fouriaud C, Jacquinet-Salord MC (1992) Length of occupational noise exposure and blood pressure. Int Arch Occup Environ Health 63: 369-372.
- Inoue M, Laskar MS, Harada N (2005) Cross-sectional study on occupational noise and hypertension in the workplace. Arch Environ Occup Health 60: 106-110.
- Pang LJ, Chen LZ, Fu BY (2005) Prevalence and influence factors of hypertension among mechanic factory workers. Zhong Nan Da Xue Xue Bao Yi Xue Ban 30: 0276-04.
- Salameh, A-NI (2005) Effects of occupational noise exposure on blood pressure, pulse rate, and hearing threshold levels of workers in selected industrial plants in Jenin City, Palestine.
- Van Dijk FJ, Souman AM, de Vries FF (1987) Non-auditory effects of noise in industry. VI. A final field study in industry. Int Arch Occup Environ Health 59: 133-145.
- Talbott E, Helmkamp J, Mathews K, Kuller L, Cottington E (1985) Occupational noise exposure, noise-induced hearing loss, and the epidemiology of high blood pressure. AJE 121: 501-514.
- Sally LL, Gillespie B, Bonnie MH, Rosemary AZ (2004) Acute effects of noise on blood pressure and heart rate. Arch Environ Health 59: 392-399.
- Ismaila SO, Odusote A (2014) Noise exposure as a factor in the increase of blood pressure of workers in a sack manufacturing industry. BJBAS 3: 116-121.
- Bing FH, Chang TY, Cheng YK, Liu CS (2012) Gene-environment interaction between angiotensinogen and chronic exposure to occupational noise contribute to hypertension. Occup Environ Med 69: 236-242.
- Zhang X, Wang Z, Li T (2010) The current status of occupational health in China. Environ Health Prev Med 15: 263-270.
Citation: Shrestha A, Shiqi M (2017) Occupational Noise Exposure in Relation to Hypertension: A Cross-sectional Study in the Steel Factory. Occup Med Health Aff 5:266. DOI: 10.4172/2329-6879.1000266
Copyright: © 2017 Shrestha A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 13509
- [From(publication date): 0-2017 - Nov 07, 2025]
- Breakdown by view type
- HTML page views: 12290
- PDF downloads: 1219