Case Report Open Access
Oral Rhabdomyosarcoma: A Case Report
Deyhimi Parviz* and Khalesi SaeidehDepartment of Oral & Maxillofacial Pathology, Dentistry School, Isfahan University of Medical Sciences, Isfahan, Iran
- *Corresponding Author:
- Parviz Deyhimi
Associate Professor
Department of Oral & Maxillofacial Pathology
Dentistry School, Isfahan University of Medical Sciences, Isfahan, Iran
Tel: 0098-311-7922879
E-mail: Deihimy@dnt.mui.ac.ir
Received Date: December 10, 2013; Accepted Date: February 19, 2014; Published Date: February 21, 2014
Citation: Parviz D, Saeideh K (2014) Oral Rhabdomyosarcoma: A Case Report. J Clin Exp Pathol 4:161. doi: 10.4172/2161-0681.1000161
Copyright: © 2014 Parviz D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
Rhabdomyosarcoma (RMS) is a malignant soft tissue neoplasm of skeletal muscle origin. The most common sites of occurrence are the head and neck, genitourinary tract, and extremities. Although Rhabdomyosarcoma has a relative predominance for head and neck region, it is less frequent in oral cavity, and accounts for only 0.04% of all head and neck malignancies. Some studies have been showed that soft palate and tongue are the most common sites for oral RMS. We present a case of oral Rhabdomyosarcoma in a 15 year old girl, and demonstrate the clinical, radiological, histological, and immunohistochemical features of this neoplasm.
Keywords
Embryonal Rhabdomyosarcoma; Muscle tumor; Oral; Sarcoma
Introduction
Rhabdomyosarcoma (RMS) is a malignant soft tissue neoplasm of skeletal muscle origin. It is the most common soft tissue sarcoma in children under 15 years of age, and rare among people older than 45 years of age. The most common sites of occurrence are the head and neck (40%), genitourinary tract (25%), and extremities (20%) [1]. Rhabdomyosarcoma are anatomically divided into 2 categories including parameningeal and nonparameningeal.
Parameningeal sites are the nasal cavity, nasopharynx, paranasal sinuses, middle ear, mastoid, infratemporal fossa, and pterygopalatine fossa. The scalp, orbit, parotid gland, oral cavity, oropharynx, and larynx are considered non parameningeal sites [2]. Oral Rhabdomyosarcoma is rare neoplasm, and accounts for only 0.04% of all head and neck malignancies [3].
Three main types histologic appearance of RMS are embryonal, alveolar and pleomorphic. The embryonal type presents the subtypes including classic, spindle cell and botryoid [4]. The embryonal type of RMS is the most common variant, and occurs in children between birth and 15 years old. The embryonal RMS contains a mixture of spindle and undifferentiated round cells and immature striated muscle like cells (rhabdomyoblasts) with abundant eosinophilic cytoplasm either tightly or loosely packed in a myxoid stroma. The botryoid tumor is a morphologic variety or subtype of the embryonal type and because of gross resemblance to cluster of grapes have been named botryoid. Histologically a multilayered band of cells just below the surface epithelium called the cambium layer is a special finding of this variant. The alveolar type presents in the older children (10 to 25 years old) and contains clusters of small round cells with hyperchromatic nuclei and eosinophilic cytoplasm separated by fibrovascular septa. Pleomorphic type occurs in older people between the age group of 50-60 years and is characterized histologically by large bizarre cells of racquet, strap, ribbon and spindle types in a haphazard arrangement [5-7].
The histogenesis of RMS is still indistinct, but the most widely believed hypothesis is that RMS arises due to proliferation of embryonic mesenchymal cells that exhibit a tendency toward myogenic differentiation and probably originate from satellite cells associated with the embryogenesis of skeletal muscle [8-10].
In this report, we present a case of oral Rhabdomyosarcoma in a 15 year old girl, and demonstrate the clinical, radiological, histological, and immunohistochemical features of this neoplasm.
Case Report
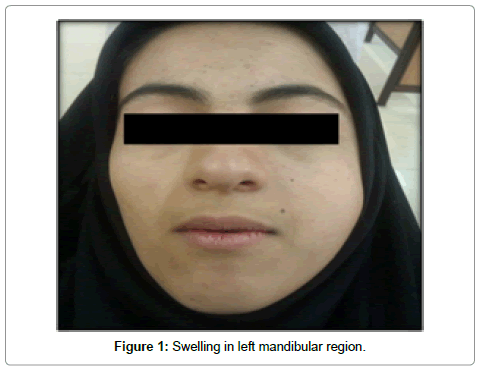
A 15 year old female was referred to the department of oral and maxillofacial surgery of dental school of Isfahan university of medical sciences in 9 mars 2013 with a chief complaint of painless swelling in the mandibular left posterior region of 40 days duration. The swelling was initially small size and quickly increased (progressive growth). She had not a past history of trauma and systemic disease. But, there was a history of weight loss before 2 month ago. According to the patient statement, there was no sign of pain, sensation disorders, pus discharge, and bleeding in the involved area. Extra oral examination showed facial asymmetry, and a diffuse, soft to firm, tender swelling in the posterior region of the mandible (Figure 1).
The left submandibular lymph nodes were palpable, firm, mobile and non-tender. Additionally, she had limitation in maximum opening.
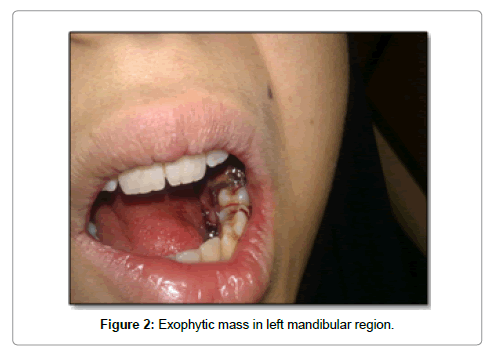
Assessment of the intraoral cavity showed a 7 × 5 cm, exophytic ulceroproliferative growth, and red to brown, soft to firm, mild tender and diffuse mass. This lesion was covering the buccal and lingual side from the first molar to the retromolar area. Furthermore, the swelling of the left cheek was obliterating the buccal vestibule. The mass was resulting in impingement with occlusion (Figure 2). According to the patient statement, after 30 days of initiation of lesion, the third molar involved in the mass exfoliated. The second molar in the affected region were displaced. The patient could speak, but could not feed comfortably, and she has orthopnea.
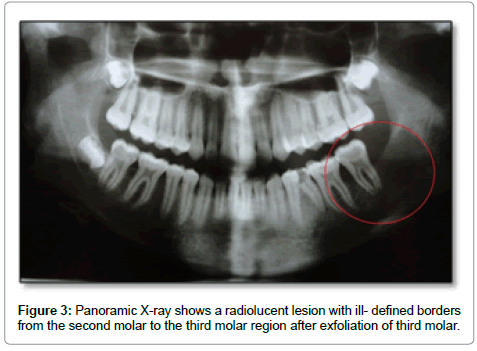
The panoramic X-ray revealed a radiolucent lesion with ill-defined borders. The lesion was extending anteroposteriorly from the second molar to the third molar region, inferiorly up to the inferior alveolar canal of the mandible and superiorly to the alveolar ridge (Figure 3).
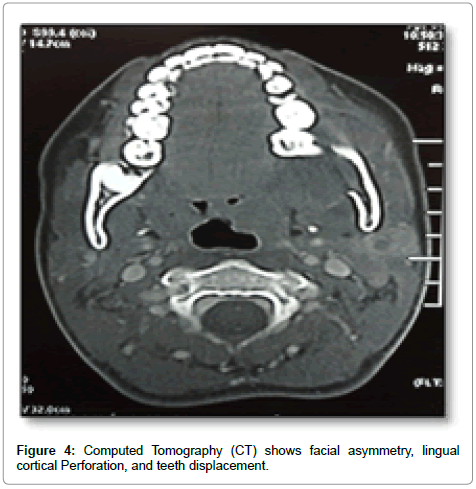
The Computed Tomography (CT) showed the infiltrative soft tissue mass. The lesion caused facial asymmetry, the marked expansion, and lingual cortical plate perforation. Displacement of the adjacent structures, and second molar was also noted (Figure 4).
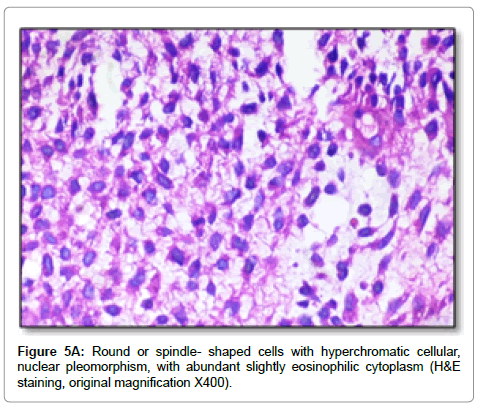
The lesion was subjected for histopathological examination via incisional biopsy under general anesthesia. Histopathological analysis of the hematoxylin/eosin-stained material showed highly cellular mesenchymal tissue containing round or spindle-shaped cells with darkly staining hyperchromatic cellular and nuclear pleomorphism, and cells with abundant slightly eosinophilic cytoplasm (Figure 5A).
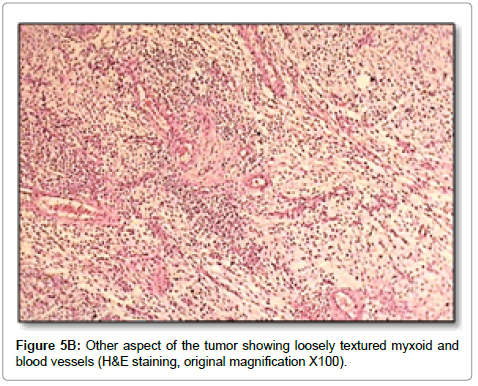
Mitotic figures, and some areas with loosely textured myxoid were noted (Figure 5B). The stroma also displayed severe bleeding, and moderate amount of mixed inflammatory cell infiltrate mainly containing, lymphocytes, plasma cells, and neutrophils. Histopathological features of this tumor indicated a differential diagnosis including Rhabdomyosarcoma, Ewing sarcoma and malignant lymphomas.
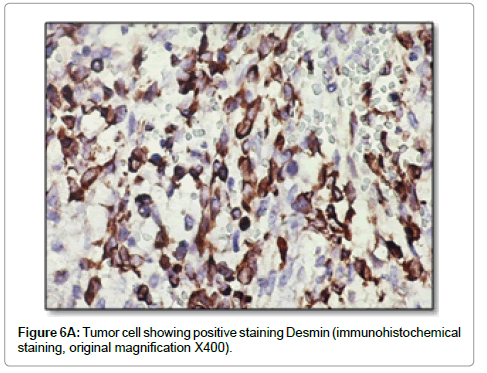
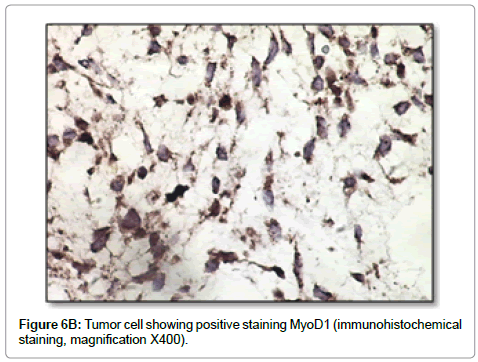
Considering the histopathological findings were not characteristic of a specific tumor, immunohistochemical staining was performed for vimentin, desmin, myogenin, MyoD1, Smooth muscle actin (SMA), S100, CD99, Leukocyte common antigen (LCA), and Ki-67. The neoplastic cells were strongly positive for vimentin, desmin, MyoD1, myogenin, and weakly positive for CD99 (Figure 6). Furthermore, the tumor cells were negative for S100, LCA, and SMA. On the basis of all the immunohistochemical staining results, the tumor was identified as embryonal Rhabdomyosarcoma. The result of immunohistochemical staining for ki-67 showed proliferative activity in 70% of tumor nuclei.
She was referred to the oncology department, and the treatment plan was a combination of chemotherapy.
Although, the tumor showed dramatic regression after the initiated 6 weeks of chemotherapy, the computed tomography showed lungs metastasis. Unfortunately the patient denied further treatment because of high cost of treatment and at present her condition is undetermined.
Discussion
Rhabdomyosarcoma is the third most common extracranial malignant tumor in children after neuroblastoma and wilms tumor [9]. The highest incidence of RMS is in the children aged 1-4 years, lower rate in children aged 10-14 aged and lowest rates between 15-19 years of age [10]. Approximately, 35% of all RMS occur in the head and neck regions. But, oral RMS is rarely encountered [7].
In oral RMS males are affected more commonly than females, and majority are occurred in first two decades of life [11]. In this report, a 15 year old female was presented. A common site of oral cavity has not been well recognized. Some studies have been showed that soft palate, tongue and buccal mucosa most common sites for oral RMS. Some other studies have been presented oral RMS in the posterior mandibular region [9,11]. Our patient involved the left mandibular posterior area.
In general, the patients with oral RMS often have an advanced lesion at the early stage, because of a rapidly enlarging painless mass, local infiltration, pain, ankyloglossia, paresthesia, and trismus. Primary oral RMS is rarely affected lymph nodes [11]. Some studies, showed involvement of the teeth in affected region [10]. In our patient, the painless mass with rapidly growing and involvement of the teeth, but no sign of pain or paresthesia was seen. She had facial asymmetry, and experienced difficulty in opening the mouth.
A careful histopathological analysis is necessary for differentiate the tumor from other small round cell tumors, which are also malignant or aggressive lesions. On the basis of some viewpoints, Rhabdomyosarcoma histologically has been divided in to four broad subtypes: botryoid and spindle cell RMS, alveolar RMS, embryonal RMS, and undifferentiated RMS [9]. The most common type of head and neck RMS are of embryonal type. In our patient, the presence of round cells with eosinophilic cytoplasm and immunohistochemical staining ruled out the diagnosis of malignant lymphomas and Ewing sarcoma. The use of immunohistochemistry for desmin, myogenin, and MyoD1, may only recommend the skeletal muscle differentiation, and is mainly beneficial for the diagnosis of RMS [12]. Positive result for vimentin showed that the tumor has a mesenchymal origin. Positive reaction for desmin indicated muscular differentiation. Although it is very sensitiveit was not very specific for skeletal muscle. Desmin could not distinguish between skeletal and smooth muscle differentiation [13]. The MyoD family include four proteins myogenin, MyoD1, myf-5, and MRF-4. Antibodies to Myogenin and MyoD1 have high sensitivity and specificity for skeletal muscle differentiation [13]. They are positive in about 90% of the RMS and the diagnosis of RMS was established only of at least one of these proteins were positive [12]. In our case, desmin, myogenin, and MyoD1 were positive. Immunohistochemical staining for CD99 mainly used for the diagnosis of Ewing sarcoma, but it is also present in other tumors, such as lymphoblastic lymphomas, and some Rhabdomyosarcoma [13]. In our case, immunohistochemical staining showed weakly positive for CD99.
Metastases develop during the progression of the disease in about 20% of cases. Major metastatic sites are the lungs, lymph nodes, and bone marrow. The lungs are involved in at least two thirds of patients’ metastasis [5]. In our patient, it was found to have metastasized to the lungs at the time of initial presentation.
References
- Wang C (2012) Childhood rhabdomyosarcoma: recent advances and prospective views. J Dent Res 91: 341-350.
- Al-Khateeb T, Bataineh AB (2002) Rhabdomyosarcoma of the oral and maxillofacial region in Jordanians: a retrospective analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93: 580-585.
- Chi AC, Barnes JD, Budnick S, Agresta SV, Neville B (2007) Rhabdomyosarcoma of the maxillary gingiva. J Periodontol 78: 1839-1845.
- Newton WA Jr, Gehan EA, Webber BL, Marsden HB, van Unnik AJ, et al. (1995) Classification of rhabdomyosarcomas and related sarcomas. Pathologic aspects and proposal for a new classification--an Intergroup Rhabdomyosarcoma Study. Cancer 76: 1073-1085.
- Enzinger FM, Weiss SW, Goldblum JR (2008) Soft tissue tumors. (5thedn), Mosby, St. Louis, USA.
- Grundy R, Anderson J, Gaze M, Gerrard M, Glaser A, et al. (2001) Congenital alveolar rhabdomyosarcoma: clinical and molecular distinction from alveolar rhabdomyosarcoma in older children. Cancer 91: 606-612.
- Chigurupati R, Alfatooni A, Myall RW, Hawkins D, Oda D (2002) Orofacial rhabdomyosarcoma in neonates and young children: a review of literature and management of four cases. Oral Oncol 38: 508-515.
- Loducca SV, Mantesso A, de Oliveira EM, de Araújo VC (2003) Intraosseous rhabdomyosarcoma of the mandible: a case report. Int J Surg Pathol 11: 57-60.
- Miloglu O, Altas SS, Buyukkurt MC, Erdemci B, Altun O (2011) Rhabdomyosarcoma of the oral cavity: a case report. Eur J Dent 5: 340-343.
- França CM, Caran EM, Alves MT, Barreto AD, Lopes NN (2006) Rhabdomyosarcoma of the oral tissues--two new cases and literature review. Med Oral Patol Oral Cir Bucal 11: E136-140.
- Arya K, Vij H, Vij R, Rao NN (2011) Rhabdomyosarcoma of mandible: A diagnostic predicament. J Oral Maxillofac Pathol 15: 320-325.
- Andrade CR, Takahama Junior A, Nishimoto IN, Kowalski LP, Lopes MA (2010) Rhabdomyosarcoma of the head and neck: a clinicopathological and immunohistochemical analysis of 29 cases. Braz Dent J 21: 68-73.
- Rosai J (2011) Rosai and Ackerman’s surgical pathology. (10thedn), Mosby, St. Louis, USA.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 17748
- [From(publication date):
March-2014 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 12916
- PDF downloads : 4832