Overview of Bone Tumours in a Tertiary Care Hospital
Received: 15-Apr-2019 / Accepted Date: 13-May-2019 / Published Date: 20-May-2019 DOI: 10.4172/2472-016X.1000130
Abstract
Background: The neoplasms of bone account for only 0.2%–0.5% of the overall human tumour biology. Most bone tumours arise de-novo from genetic mutations; but numerous risk factors such as chemotherapy, irradiation, foreign bodies, bone infarcts and pre-existing bone lesions have been implicated. Bone tumours have heterogeneous population of cells and morphology. For accurate diagnosis of tumours and tumour like lesions of bone, there is a need of tissue diagnosis & staging and radiological diagnosis to delineate the plane of tumour involvement and its appropriate management.
Objectives: To study the spectrum of clinico-radiological & histopathological features and management of tumour and tumour like lesions of bone and to establish the statistical significance by testing the agreement between clinicoradiological and histopathological diagnosis by Cohen’s kappa value.
Materials and Methods: A total of 76 cases (14 clinical entities) were taken in our study. All cases underwent thorough clinical, hematological and radiological investigations to arrive at an empirical diagnosis of the lesions. Then all patients were subjected for histopathological tissue sampling (FNAB (Fine Needle Aspiration Biopsy) or incisional biopsy) for accurate diagnosis which guide the orthopaedic surgeon to plan the appropriate line of management. All the cases were under surveillance for diagnosing the development of metastasis.
Results: The histopathological correlation of 95.37% with 97.25% sensitivity, 95.41% specificity, 97.01% positive predictive value and 95.41% negative predictive value in diagnosing musculoskeletal tumours. The strength of agreement between clinico-radiological and histopathological diagnosis by Cohen’s kappa value was very good (κ=0.817).
Conclusion: The management of tumours and tumour like lesions of bone pose a greater challenge for an orthopaedic surgeon in instituting treatment modalities. The successful diagnosis of bone tumour and its management depends on collaboration between the orthopaedic surgeon and the pathologist who determine the need for secondary biopsy in diagnosing bone and soft tissue tumourse.
Keywords: Bone Tumours; Cohen’s Kappa; Histopathology; Fine Needle Aspiration Biopsy (FNAB); Incisional Biopsy
Introduction
The neoplasms of bone account for only 0.2%–0.5% of the overall human tumour biology [1]. The uncommonness of bone tumours has contributed to the paucity of the relative frequency, incidence rates and risk factors of the various subtypes of bone tumours [1]. Most bone tumours arise de-novo from genetic mutations; but numerous risk factors such as chemotherapy, irradiation, foreign bodies, bone infarcts and pre-existing bone lesions have been implicated [2]. The aetiology of bone cancers is better established than their benign counterparts [3].
The classification of bone tumours by the World Health Organization (WHO) on 2013 has been developed with the framework and concept of the cellular origin which is widely accepted [4]. This classification is based on the line of histological differentiation by reflecting the type of intercellular matrix material produced by the particular bone tumour [4,5].
The evaluation and treatment of bone tumour is a crucial part of the core of orthopaedics. Bone tumours assume an aggressive course and prove to be more lethal, with extensive metastasis. The wide spectrum of these bone tumours, their diverse origins from the multiple cell types found in bones coupled with the tendency of these tumours to produce overlapping anatomic pattern, make osseous neoplasm a complicated but highly challenging area from the point of view of morphological diagnosis. In general, the incidence of bone and joint cancers are higher in whites than in blacks and higher in males than in females, with patients less than 20 years accounting for the majority of affected individuals [6].
The definitive clinical diagnosis of bone lesion is often difficult. So, it is essential to identify the lesion correctly before deciding the line of treatment, which may range from simple curettage and bone grafting, excision surgery, amputation, irradiation or palliative management. For accurate diagnosis of tumours and tumour like lesions of bone warrants the tissue diagnosis and staging. Along with pathological diagnosis, radiological diagnosis like radiographs, CT, MRI, PET and bone scan helps in delineating the plane of tumour involvement and its spread to soft tissues & neurovascular structures [1,2,6].
Objectives
• To prospectively study the spectrum of clinico-radiological & histopathological features and management of tumour and tumour like lesions of bone.
• To establish the statistical significance by testing the agreement between clinico-radiological and histopathological diagnosis by Cohen’s kappa value.
Materials and Methods
With a level IV evidence, a prospective cohort study was performed from 2015 to 2018 in the department of Orthopaedics, Bapuji hospital and Chigateri Government General hospital, JJM Medical College, Davangere, Karnataka, India. The cases for this study were recruited by convenient sampling technique. A total of 76 cases (14 entities) of tumour and tumour like lesions of bone were included and managed appropriately.
The patients of all age groups of both sexes, patients with clinical suspicion of primary tumours and tumour like lesions of bone, patients with clinical suspicion of metastatic bone lesions and patients who were willing to participate were included in the study. The patients with confirmed diagnosis of bone tumours, patients with confirmed bone tumours under chemotherapy and radiotherapy, patients with confirmed bone tumours with palliative treatment regimen, patients with confirmed lymphoma and leukemia and patients who refused to participate in the study were excluded in the study.
After obtaining the informed and written consent from the patients, they were subjected to thorough clinical examination, laboratory investigations like complete blood count, peripheral smear, renal function tests, liver function tests, serum calcium, phosphorus, vitamin D3 & alkaline phosphatase and serological tests like HIV, HbsAg & HCV. All patients were subjected to radiological analysis with plain radiograph of the affected part, CT scan to delineate the tumour margins and MRI to obtain information about surrounding structures and soft tissue involvement. WHO classification of bone tumour system were followed in our study.
For all 14 clinical entities, one case in each clinical entity has been explained in detail with pre-treatment, FNAC, histopathological and post treatment investigations.
Case Series
Case entity 1–Simple bone cyst
A 10 year old female patient came with chief complaints of pain over right shoulder since 2 months and inability to use the right shoulder. On examination, the patient had a deformity over right arm. The radiographic evaluation showed a lytic lesion over proximal 1/3rd shaft of right humerus with a pathological fracture over the lesion. A fine needle aspiration biopsy reported fibrous tissue, giant cells with spindle shaped cells (Figure 1).
Figure 1: (a) Radiograph of right humerus showing a lytic lesion over proximal 1/3rd shaft of humerus with a pathological fracture over the lesion. (b) MRI of right humerus in coronal section showing a well defined intramedullary altered signal intensity of lesion with a pathological fracture of lesion without periosteal reaction and soft tissue invasion suggestive of simple bone cyst with pathological fracture.
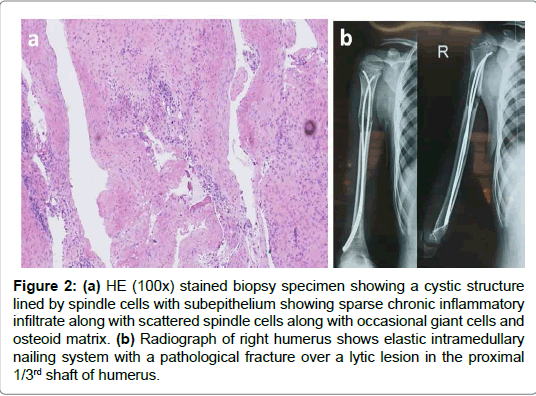
MRI right humerus showed a lytic lesion with thinning of cortex and a pathological fracture over the lesion over proximal 1/3rd shaft of humerus. The pathological fracture over the lesion was managed with thorough curettage of the lesion and intramedullary elastic nailing of humerus. The intraoperative curetted lesion confirmed the diagnosis of simple bone cyst in the histopathological examination (Figure 2).
Figure 2: (a) HE (100x) stained biopsy specimen showing a cystic structure lined by spindle cells with subepithelium showing sparse chronic inflammatory infiltrate along with scattered spindle cells along with occasional giant cells and osteoid matrix. (b) Radiograph of right humerus shows elastic intramedullary nailing system with a pathological fracture over a lytic lesion in the proximal 1/3rd shaft of humerus.
Case entity 2–Aneurysmal bone cyst
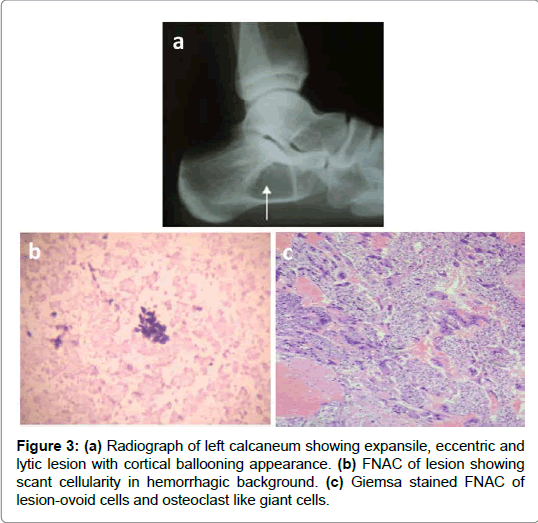
A 21 year old female patient came with chief complaints of pain over left heel since 5 months and inability to bear weight over left foot. The patient had radiographic evaluation which showed a lytic lesion over anterior aspect of left calcaneum without any pathological fracture over the lesion. FNAC of the lesion showed scant cellularity with hemorrhagic background and occasional osteoclastic type of giant cell (Figure 3).
The patient has been treated with aggressive curettage of the lesion and cancellous bone grafting of left calcaneum. The biopsy material subjected for histopathological examination confirmed the diagnosis of aneurysmal bone cyst (Figure 4).
Case entity 3–Giant cell tumour of tendon sheath
A 27 year old male patient came with chief complaints of swelling over right ring finger of 8 months duration. On examination, the swelling was mobile in both directions, non-compressible and nontranslucent. The radiographic evaluation showed a slight tissue swelling over DIP joint of right ring finger without any bony involvement. The swelling was subjected for FNAC which showed osteoclast like giant cells admixed with mononuclear cells. Then the patient was managed with excisional biopsy of the lesion and chemical cauterization with hydrogen peroxide sponging. The histopathological examination of the lesion showed abundant mononuclear cells and osteoclast type of giant cells along with thick fibrous septa which was suggestive of giant cell tumour of tendon sheath (Figure 5).
A total of 25 cases of soft tissue swelling over fingers were diagnosed as giant cell tumour of tendon sheath and were managed with excisional biopsy of lesion and chemical cauterization with hydrogen peroxide sponging. No recurrence of lesion was observed in 3 years follow up (Figure 6).
Case entity 4–Fibrous dysplasia
A 20 years old female patient presented with pain and deformity over right arm and forearm of 5 years duration. The patient noticed a visible deformity over right arm which was gradually progressive and associated with increased intensity of pain. On examination, diffuse tenderness and visible deformity were noted over right arm and forearm. The range of movements over right shoulder, right elbow and right wrist were near normal with terminal painful movements. Elevation of serum ALP and low levels of vitamin D3 were noticed. Radiography of right arm and forearm showed the evidence polyostotic pattern of fibrous dysplasia of whole length humerus and radius with ulnar sparing. The patient had an open biopsy of distal humerus and histopathological examination which confirmed the diagnosis. Pattern with spindle shaped cells in stromal background (Figure 7).
The patient has been managed with bisphosphonates (Tab. Risedronate 35 mg once weekly for 24 weeks), calcium and vitamin D3 supplementation for 24 weeks. Every month patient is assessed with radiographs and serum vitamin D3, calcium, phosphorus and alkaline phosphate. The patient is followed up for one year which shows no recurrence, decreased pain and improved functional quality of life (Figure 8).
Figure 8: (a) FNAC showing bony trabeculae mimicking Chinese letter pattern with spindle shaped cells in stromal background. (b) HPE (40x) shows trabeculae of woven bone which lacks osteoblastic rimming in a Chinese letter pattern surrounded by fibroblastic proliferation admixed with few osteoclast like giant cells.
Case entity 5–Lipoma arborescens
A 47 years old female patient came with complaints of left knee swelling and occasional pain with mild restriction of movements in left knee joint since 1 year. Examination revealed soft boggy swelling in the suprapatellar fossa with effusion. Plain radiograph of left knee joint showed the features of grade 3 osteoarthritis of bilateral knee joints (reduction of medial joint space with osteophytes). MRI left knee shows well defined heterogeneous multiloculated signal intensity lesion with septations noted in medial aspect of suprapatellar pouch with minimal joint effusion (Figure 9).
The patient underwent open synovectomy. Histopathology of the synovectomy specimen shows hypertrophic villous projections of fat lined by synovial cells with variable scattered inflammatory cells. The postoperative period was uneventful and the patient had good range of movements over left knee without recurrence in 2 years of follow up period (Figure 10).
Case entity 6–Giant cell tumour
A 34 years old male patient came with complaints of swelling over medial aspect of left knee swelling and occasional pain with restriction of movements in left knee joint since 1 year. Examination revealed ballooned out bony swelling with effusion. Plain radiograph of left knee joint showed an eccentric, expansile and lytic lesion with soap bubble appearance over medial aspect of proximal tibia which was suggestive of giant cell tumour. MRI of left knee showed the features of giant cell tumour without cortical breach. FNAC of the lesion showed osteoclastic giant cells with characteristic nuclei (Figures 11 and 12).
The patient had bony curettage and cortico-cancellous bone grafting. Histopathology of the bone specimen showed numerous osteoclast like giant cells uniformly distributed throughout the tumour and are admixed with spindle to ovoid benign mononuclear cells. In 2 year follow up period, osteointegration of bony chips were seen over medial condyle of left tibia (Figure 13).
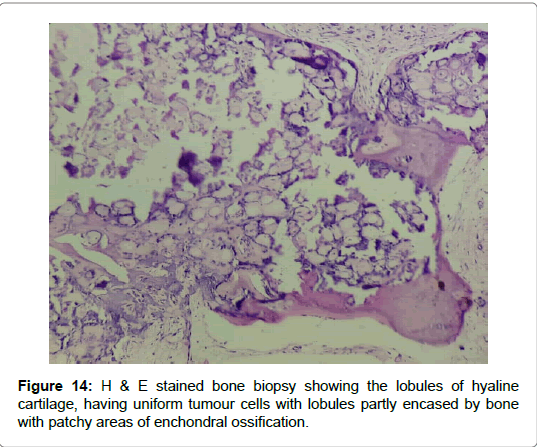
Case entity 7–Enchondroma
A 19 years female patient came with complaints of pain and swelling over middle phalanx of ring finger of right hand from past 8 months. Examination revealed ballooned out bony swelling over middle phalanx. Plain radiograph of right hand shows expansile lytic lesion of middle phalanx of ring finger. The patient was sent for FNAC, which showed cellular smear which had predominantly cartilage tissue fragment with uniform tumour cells, focal fragments of calcification and myxoid change. The patient underwent excisional biopsy and PMMA filling of the cavity. No recurrence was observed in the follow up period. Histopathology of the lesion showed lobules of hyaline cartilage, having uniform tumour cells with lobules encased by bone with patchy areas of enchondral ossification (Figure 14).
Case entity 8–Exostosis
A 29 year old female patient came with complaints of bony swelling over middle phalanx of middle finger from past 2 years. The swelling was not associated with pain. The patient underwent excisional biopsy of the lesion. The biopsy showed benign tumour composed of wellformed cartilaginous cap with underlying mature bone separated by distinct transition zone. No recurrence was observed in the follow up period of 1 year (Figures 15 and 16).
Case entity 9–Hereditary multiple exostosis
A 37 years old male came with complaints of bilateral multiple swellings around the elbows and the knees. The swellings were noticed by the patient at the age of 14 years. On examination, all the swellings were globular and bony hard in consistency. The radiograph of right and left knee joint show multiple swelling arising from metaphyseal end towards diaphysis with a cartilage cap at the end. Due to pain over right elbow, excision biopsy of two globular swellings were performed. The histopathology of the biopsy showed hyaline cartilage capping with well defined perichondrium, normal primary trabeculae and linear clusters of active chondrocytes (Figure 17).
The patient was under regular surveillance for increase in pain around the swelling or increase in size of the swelling for early diagnosis and prompt management of malignant change of the tumour.
Case entity 10–Osteosarcoma
A 49 years old male came with complaints of swelling and pain over right knee joint since 9 months. The patient looked cachetic and had loss of weight & appetite. On examination, an irregular swelling of 9x6x4 cm which was smooth, non-mobile with ill-defined edges, variable in consistency, was seen over medial aspect of the proximal 1/3rd of the right leg. There was diffuse thickening and irregularity of proximal one third of the tibia. There was no enlargement of regional lymph nodes (Figure 18).
Radiograph of right leg showed eccentric and lytic lesion on the proximal one third of right tibia and soft tissue swelling. Laboratory investigations showed increased serum calcium, serum phosphate and serum alkaline phosphatase. FNAC of the lesion showed markedly cellular smear composed of pleomorphic cells tumours cells which predominantly spindle shaped and few round shaped with numerous mitotic bodies with malignant osteoid in the background, suggestive of osteosarcoma of right tibia. Skeletal survey showed no metastasis of osteosarcomal tumour tissue. MRI scan of knee in coronal section showed an osseous overgrowth in the medial condyle of the knee. PET scan showed no regional uptake in activity in search of metastatic activity of the tumour (Figure 19).
The patient underwent incisional biopsy which showed pleomorphic spindle shaped cells arranged in sheets with malignant osteoid formation amid the tumour cells. Then the patient was referred for palliative management in the form of chemoradiation and counselled for en-bloc resection and combination of autologous bone grafting with bone substitutes. The patient was followed up for development of metastasis (Figure 20).
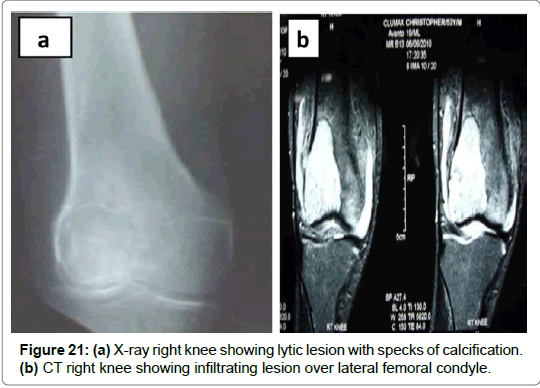
Case entity 11–Chondrosarcoma
A 36 old female patient came with complaints of pain and swelling over right knee from past 3 months. The patient had loss of weight & appetite. On examination, an irregular swelling of 7x6x4 cm which was bosselated, non-mobile with ill-defined edges, variable in consistency, was seen over medial aspect of the proximal 1/3rd of the right leg. There was diffuse thickening and irregularity of proximal one third of the tibia. The radiograph of right knee showed diffuse lytic lesion over lateral condyle of right femur with specs of calcification. The CT scan of right knee showed infiltrating lesion over lateral femoral condyle of right knee (Figures 21 and 22).
FNAC of the lesion showed cellular smear with tumour cell small clusters and occasionally in singles. These cells are large, pleomorphic with nucleus showing hyperchromasia, karyomegaly and abundant eosinophilic vacuolated cytoplasm with background showing chondromyxoid matrix. The patient underwent incisional biopsy of the lesion which showed lobules of large pleomorphic chondrocytes against chondroid matrix. The patient was referred for neoadjuvant chemotherapy followed by surgical management with en-bloc tumour resection and custom mega prosthesis fixation. The patient was given post-op chemotherapy for 6 cycles. The patient was under sentinel surveillance for development of metastasis (Figure 23).
Case entity 12–Ewing’s sarcoma
A 26 year old female came with complaints of sudden onset of pain over left hip since 1 month. The patient got treated with analgesics and antibiotics for 1 week duration. Then they noticed gradually increased swelling over left hip and was unable to bear weight on left lower limb. Then the patient underwent radiological screening in which they found permeative lytic lesion of left ilium. CT left hip showed lytic and sclerotic lesion of left ilium with soft tissue expansion (Figure 24).
The patient underwent CT guided biopsy which showed small round tumourigenic cells suggestive of ewing’s sarcoma. It was confirmed with immunohistochemical staining with CD 99 which turned to be positive. The patient was advised for high dose chemotherapy to control the proliferation of cells in the surrounding soft tissues and high voltage radiotherapy for immediate cytoreduction of the tumour. The patient expired after 6 months of follow up due to enormous cellular proliferation, development of metastasis and radioresistant cells (Figure 25).
Case entity 13–Multiple myeloma
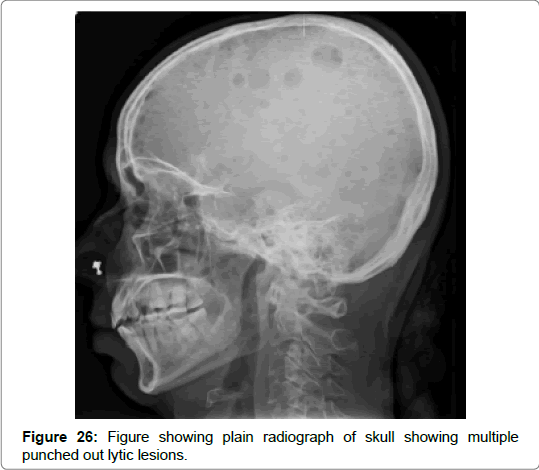
A 21 years old male came with complaints of high grade fever, recurrent infections and ecchymosis around left elbow and right thigh from past 6 months. Initially the patient was managed conservatively for 3 weeks duration. Then hematological and biochemical analysis showed increased ESR, CRP, serum alkaline phosphatase. Serum electrophoresis showed prominent M band. Urine analysis showed the presence of bence jones proteins. X ray of the skull revealed multiple punched out lytic lesions. All these findings were suggestive of multiple myeloma (Figure 26).
The bone marrow aspirate study revealed the presence of multinucleated plasma cells and differentiated myeloma with plasmablastic cells having a prominent nucleus. Then the patient was referred to medical oncologist for management and was followed up every 3 months with serum β2 microglobulin and urine bence jones proteins. All patients proved immediate cytoreduction in tumourigenic cells and improvement in physical condition (Figure 27).
Case entity 14-Metastatic adenocarcinoma of tibia
A 65 year old male patient came with complaints of pain and swelling on the medial aspect of the upper 1/3rd of right leg since 2 months which was the size of peanut and gradually increased in size to attain the size of 8×8 cm. The patient had decreased breath sounds with dull resonant in percussion over the right infra-mammary and right infra-axillary region. On examination, a solitary oval swelling of 8x8 cm which was smooth, non-mobile with ill-defined edges, firm in consistency, nonreducible and non-compressible, was seen over medial aspect of the proximal 1/3rd of the right leg. There was thickening and irregularity of the anteromedial aspect of proximal one third of the tibia. There was enlargement of right superficial group of inguinal lymph nodes.
Radiograph of right leg showed eccentric and lytic lesion on the proximal one third of right tibia with periosteal reaction and soft tissue swelling. CT scan of the right leg report showed an evidence of a soft tissue density mass lesion likely to be arising from the leg muscle on the medial side of the tibia, measuring approximately 31×32 mm with numerous tiny calcific lesions within the tumorigenic mass and infiltrated into the medullary cavity and given probability of myosarcomatous tumour or osteogenic sarcoma. FNAC of the lesion showed marrow elements in the form of normoblast and myeloid series of cells along with there were foreign cell clusters having high N:C ratio, karyomegaly, anisonucleosis with mitotic figures and gland formation which was suggestive of metastatic adenocarcinoma of right tibia (Figure 28).
To rule out primary lesion, a skeletal survey was done which showed a well defined, coin shaped lesion in the right lower lobe. Contrastenhanced CT of chest showed features of multiple nodular metastatic lesions in both lung fields which confirmed primary pulmonary malignancy with pulmonary and mediastinal nodal metastases. CECT of abdomen report showed few small minimally enhancing lesions largest measuring approximately 6×5 mm seen in left lobe of liver with left retrocrural necrotic lymph node approximately 23×25 mm suggestive of metastasis. CT guided FNAC of the mass of the right lower lobe of the lung reported similar histological features of swelling of the leg suggesting non-small cell carcinoma–Adenocarcinoma of the lung. The incisional biopsy report of the swelling on the right leg showed similar histological features as that of FNAC of the pulmonary lesion and swelling on the right leg, suggestive of metastatic adenocarcinoma of tibia. The patient underwent palliative management in the form of chemoradiative therapy and the patient was under follow up (Figures 29 and 30).
Figure 30: (a) CT guided FNAC of lung mass showing clusters of malignant cells with coarse chromatin and glandular cells with attempt to form acini and macrophages. (b) H & E stained cellular smear of lung FNAC shows pleomorphic tumour cells in dyscohesive clusters against haemorrhagic background with numerous pigment laden (anthracotic) macrophages.
Results
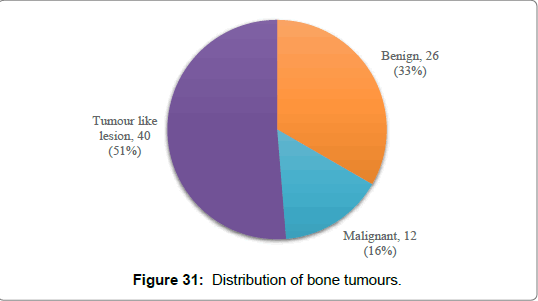
Out of 76 cases in this study, 24 cases (31.57%) were benign, 12 cases (15.78%) were malignant bone tumours and 40 cases (52.63%) were tumour like lesions of bone and soft tissues. Out of 76 cases, 49 cases (64.47%) were males and 27 cases (35.52%) were females (Figures 31 and 32) (Table 1).
| Classification | Clinical entity | No of cases | |
|---|---|---|---|
| Osteogenic | Malignant | Osteosarcoma | 6 |
| Chondrogenic | Benign | Enchondroma | 2 |
| Osteochondroma | 4 | ||
| Multiple hereditary exostosis | 2 | ||
| Malignant | Chondrosarcoma | 2 | |
| Hematopoietic | Malignant | Multiple myeloma | 6 |
| Lipogenic | Benign | Lipoma arborescens | 2 |
| Unknown origin | Benign | Giant cell tumour | 8 |
| Malignant | Ewings sarcoma | 3 | |
| Tumour like lesions | Fibrous dysplasia | 7 | |
| Giant cell tumour of tendon sheath | 25 | ||
| Simple bone cyst | 5 | ||
| Aneurysmal bone cyst | 3 | ||
| Metastasis | Adenocarcinoma of tibia | 1 | |
Table 1: Classification of musculoskeletal tumours in our series.
Statistical analysis
All the cases were subjected for histopathological screening and tests were applied which were tabulated in the below table (Table 2).
| Studies | Histopathological correlation | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|---|
| Verma [7] | 90.91% | 90.00% | 91.67% | 90.00% | 91.67% |
| Nirmala [8] | 82.6% | 91.60% | 90.90% | 91.65% | 90.90% |
| Mahajan [9] | 93.75% | 92.85% | 94.44% | - | - |
| Kujur [10] | - | 96.66% | 95.23% | 97.75% | - |
| Current study | 95.37% | 97.25% | 95.41% | 97.01% | 95.41% |
Table 2: Role of histopathological studies in diagnosing bone tumours.
The strength of agreement between clinico-radiological and histopathological diagnosis by Cohen’s kappa value was very good (κ=0.817).
Discussion
The proper and prompt diagnosis of bone tumour is imperative and warrants a multi-diagnostic approach ranging from hematological diagnosis (Hb, ESR, CRP, serum calcium, serum phosphates, serum alkaline phosphatase, tumour markers), radiological diagnosis (radiographs, CT, MRI, PET and bone scan) and tissue diagnosis (FNAC, biopsy and gross morphology) [11]. Out of all these modalities, tissue diagnosis is a critical step in the diagnosis of musculoskeletal tumours.
A biopsy is indicated when a mass has biological activity and further treatment will be based on the biopsy report. All musculoskeletal lesions have to be treated as malignant lesions unless and until it is proved otherwise. The staging of lesion helps to determine the exact anatomical approach to tumour spread and specifies the regional location of tumour which represents the underlying pathology. Since musculoskeletal tumours are heterogeneous in nature, a multiple number of samples are required to establish the proper diagnosis [12]. In our study series, the bone tumours were graded according to WHO classification (Table 3).
| Swelling of bone or soft tissue ↓ Thorough history taking, physical and clinical examination ↓ Laboratory hematological, tumour biology profile, radiological diagnosis |
||
| Negative results ↓ Review diagnosis and treat the underlying pathology |
Positive results ↓ Perform Fine Needle Aspirate Biopsy (FNAB) ↓ Perform percutaneous core needle biopsy under fluoroscopic guidance if FNAB is inadequate or inconclusive |
|
| Benign histopathological report ↓ Excisional biopsy |
Malignant histopathological report ↓ Incisional biopsy and treat accordingly |
|
Table 3: Algorithm for diagnosing musculoskeletal tumours.
In our present study, non neoplastic lesions (n=40, 52.63%) out numbered neoplastic lesions (n=36, 47.36%). In present study, out of total 76 cases, maximum number of cases were tumour like lesions (n=40, 52.63%) followed by chondrogenic tumours (n=10; 13.15%). Bamanikar et al. study showed highest number of chondrogenic tumours [13] and Settakorn et al. presented highest number of hematologic neoplasms [14] which were in contrast to our study.
Osteogenic neoplasms
In our series, 6 cases of osteosarcoma have been encountered in our study duration. All cases underwent tissue diagnosis and treatment were instituted according to the tumour encasement and tumour margin clearance. Out of 6 cases, 1 case presented with fungating lesion from right distal femur with uncontrolled proliferation of malignant tissue for which debulking of the tumour were done and referred for chemoradiation therapy. The prognosis of osteosarcoma depends on the cell type. Godley et al. reported that 26% of osteosarcoma arise from distal femur with osteosarcoma as the most common histological diagnosis and the median survival was 12 months [15].
Chondrogenic neoplasms
A total of 8 benign and 2 malignant cases of chondrogenic tumours were followed up in our study duration. All benign cases (2 cases of enchondroma and 4 cases of osteochondroma) were offered excisional biopsy except 2 cases of hereditary multiple exostosis for which treatment were given when intensity of the symptoms increases. Malignant cases were operated with en-bloc resection under neoadjuvant chemotherapy coverage and post-operative chemotherapy. The patients were under routine surveillance for development of metastasis. Bamanikar et al. [13] reported 30 cases of osteochondroma and 5 cases of chondrosarcoma out of 216 cases of bone and soft tissue tumours. They had instituted surgical management along with neoadjuvant chemotherapy cycles which is in par with our study.
Hematopoietic neoplasms
All 6 cases were diagnosed clinically, hematological investigations and bone marrow biopsy. All cases were treated with medical management. Early diagnosis and management improve the quality of life of patients. Ames et al. suggested that PET/CT, which is now recommended as the preferred method of monitoring therapy response given its ability to differentiate metabolically active from inactive disease of multiple myeloma. They suggested medical management for multiple myeloma as the standard treatment option than radiotherapy [16].
Lipogenic neoplasms
Lipoma arborescens comprise of <0.5% among all lipomatous lesions. MRI of the affected knee appear to be the most sensitive diagnostic modality of choice. 2 cases of lipoma arborescens were observed and treated with synovectomy of knee joint. Both the cases were followed up without any recurrences. Liddle et al. emphasised MRI scan for lipoma arborescens were consistent with histomorphological appearance of biopsied specimen [17].
Neoplasm of unknown origin
A total of 8 cases of giant cell tumour were observed and were diagnosed accurately with combination of radiological and histopathological studies. The number of stromal cells against giant cell background per high power field were taken into consideration for grading of giant cell tumour. All these cases were operated with curettage and bone grafting or PMMA cementing. No recurrences were observed. Zhen hua Gao et al. reported lower recurrence rate with the use of bone cement than bone grafting following aggressive intralesional curettage of benign giant cell tumours of the long bone [18].
All 3 cases of malignant Ewing’s sarcoma were studied during our study period. Out of 3 cases, 2 cases were misdiagnosed as acute osteomyelitis for which accurate diagnosis were encountered using histopathological reporting. An average of 8 cycles of chemotherapy were given for cytoreduction. Since these tumours were radiosensitive, the patients were referred to radiotherapy units where high dose radiation were given. Khaliq et al. suggested early diagnosis with PET scan helps in diagnosing the early micrometastasis and increase the quality of life of patients by providing appropriate chemoradiotherapy [19].
Tumour like lesions
Out of 7 fibrous dysplasia cases, 5 cases (3 polyostotic and 2 monostotic) were managed with tablet risedronate 35 mg once weekly for 6 months which showed ossification & mineralization and improvement in deformity at the end of follow up. The other 2 cases were operated with prophylactic internal fixation due to progressive deformity at the time of presentation. Nixon et al. presented two cases of polyostotic FD with epiphyseal lesions and reported that fibroosseous aberration initially occurred in the epiphyseal growth plate and occasionally showed a bidirectional extension into the metaphysis and epiphysis across the growth plate [20].
Out of 25 cases of giant cell tumour of tendon sheath, all cases underwent surgical excision with chemical cauterization (hydrogen peroxide sponging). There were 2 cases of recurrence during one year follow up period. Those 2 recurrence cases were re-operated with thorough excision along with native tissue. Madhan et al. have concluded that thorough dissection of tumorous mass with chemical cauterization reported no recurrence in the follow up period [21].
All 5 simple bone cyst cases were diagnosed radiographically and operated with percutaneous steroid injection, curettage and either internal fixation or bone grafting after thorough radiological and tissue diagnosis. Noordin et al. suggested that plain roentgenograms are the diagnostic modality of choice for simple bone cysts. Surgical management of simple bone cyst depends on the signs of impending pathological fractures based on Mirel’s criteria [22].
All 3 cases of aneurysmal bone cyst were studied histopathologically and radiologically for appropriate diagnosis. Kaplanoğlu et al. concluded that correlation of the clinical presentation, anatomical localization, radiological profile and histological evaluation are required for an aneurysmal bone cyst for appropriate diagnosis [23].
Metastatic neoplasm
A single case of metastatic adenocarcinoma of tibia secondary to non-small cell adenocarcinoma of lung was identified. Since adenocarcinoma of tibia is very rare, the biopsies of tibial lesion were consistent with CT guided biopsy of lung lesion, which led to diagnose the clinical entity. The patient was advised for palliative management in the form of chemoradiation. Sugiura et al. found a favourable prognosis which was more likely in women and in patients with PS 1 or less, adenocarcinoma, solitary bone metastasis, no metastasis to the appendicular bone, no pathologic fracture and the use of systemic chemotherapy. They suggested treatment with EGFR inhibitor improves survival after bone metastasis [24].
Our current study showed histopathological correlation of 95.37% with 97.25% sensitivity, 95.41% specificity, 97.01% positive predictive value and 95.41% negative predictive value in diagnosing musculoskeletal tumours. The strength of agreement between clinicoradiological and histopathological diagnosis by Cohen’s kappa value was very good (κ=0.817) which is similar to study conducted by Bayush et al. (κ=0.82) [25].
Conclusion
The management of tumours and tumour like lesions of bone pose a greater challenge for an orthopaedic surgeon in instituting treatment modalities. Since all the tumours share the same clinical features, the clinical diagnosis will be inconclusive and misguide in some instances while making diagnostic decisions. The tumour markers, metabolic panel (serum calcium, serum phosphates, serum alkaline phosphatase), special staining (Giemsa & Leishman) and immunohistochemistry of the tumour delineate the tumour lineage of specific variety. To trace out the exact diagnosis of bone tumours, cellular and tissue diagnosis is of utmost importance. The exact goal of tissue diagnosis is to obtain diagnostic tissue while minimizing morbidity, limiting potential tumour spread and avoiding interference with future treatment prospects. The successful diagnosis of bone tumour and its management depends on collaboration between the orthopaedic surgeon and the pathologist who determine the need for secondary biopsy in diagnosing bone and soft tissue tumours.
Acknowledgements
Nil
Conflicts of Inter
Nils.
References
- Katchy KC, Ziad F, Alexander S, Gad H, Abdel Mota'al M (2005) Malignant bone tumors in Kuwait: a 10- year clinicopathological study. Int Orthop 29:406-411.
- Fletcher CDM, Unni KK, Mertens F (2002) World Health Organization classification of tumours: Pathology and genetics of tumours of soft tissue and bone. IARC Press: Lyon. 225-232.
- Mohammed A, Isa HA (2007) Patterns of primary tumours and tumour-Like lesions of bone in Zaria, Northern Nigeria: A review of 127 cases. Wesr Afr J Med 26:37-41.
- Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F (2013) WHO Classification of tumours of soft tissue and bone. Lyon: IARC Press 240-365.
- Mohammed A, Sani MA, Hezekiah IA, Enoch AA (2010) Primary bone tumours and tumour-like lesions in children in Zaria, Nigeria. Afr J Paediatr Surg 7:16–18.
- Verma N, Tyagi A, Singh P, Tyagi M, Rathi M, et al. (2018) Incidence of bone tumors and tumor like lesions at a tertiary centre – a study of 64 cases. Int J Res Med Sci 6: 533-538.
- Nirmala C, Patil P, Sejekin SV, Raghupathi AR (2014) Technical challenges and spectrum of lesions in fine needle aspiration cytology of bone lesions. Int J Cur Res Rev 6: 25-31
- Mahajan S, Saoji AA, Agrawal A (2015) Utility of Fine Needle Aspiration Cytology in Diagnosing Bone Tumors. Cancer Transl Med 1: 166-169.
- Kujur P, Kosam S (2016) Fine Needle Aspiration Cytological Study of Bone Tumors and Tumor-like Lesions: A Review of Cases with Cytologicalhistopathological Correlation. Int J Sci Stud 4: 214-219.
- Rosenberg AE (2010) Bones, joints and soft tissue tumors. Pathologic Basis of disease. Elsevier Reed Elsevier India private limited 1205–1256.
- Jain K, Ravishankar R, Rupakumar CS, Gadiyar HB, Manjunath GV (2011) Bone tumours in a tertiary care hospital of south India: a review 117 cases. Indian J Med Paediatric Oncol 32: 82.
- Bamanikar SA, Pagaro PM, Kaur P, Chandanwale SS, Bamanikar A, et al. (2015) Histopathological Study of Primary Bone Tumours and Tumour-Like Lesions in a Medical Teaching Hospital. JKIMSU 4: 46-55.
- Settakorn J, Lekawanvijit S, Arpornchayanon O, Rangdaeng S, Vanitanakom P, et al. (2006) Spectrum of Bone Tumors in Chiang Mai University Hospital, Thailand According to WHO Classification 2002: A Study of 1,001 Cases. J Med Assoc Thai 89: 780.
- Godley K, Watts AC and Robb JE (2008) Pathological Fracture of the Femur as a Presenting Feature of Primary Bone Tumor. Bone Joint J 90: 400.
- Ames J, Al-Samaraee A, Takahashi T (2017) Extraosseous Multiple Myeloma: Case Report of Presentation in the Lower Extremity Soft Tissues with Literature Review. Case Rep Radiol.
- Liddle A, Spicer D, Somashekar N, Chirag T (2012) Lipoma Arborescens of both Knees-Case report and Literature Review. J Orthop Case Rep 2:28–30.
- Gao ZH, Yin JQ, Xie XB, Zou CY, Huang G, et al. (2014) Local control of giant cell tumour of the long bone after aggressive curettage with or without bone cement. BMC Musculoskeletal Disorders 15:330.
- Khaliq W, Bahador MF, Laurence TN, Sapiente RA, Lewis JS, et al. (2012) Ewing's sarcoma: A case report of a 52-year-old woman with recurrent tumor and literature review. Oncol Lett 3: 155–158
- Nixon GW, Condon VR (1973) Epiphyseal involvement in polyostotic fibrous dysplasia. A report of two cases. Radiology 106: 167–170.
- Jeyaraman M, Ramesh R, Chaudhari K, Ajay SS, Prajwal GS (2019) Surgical Management of Giant Cell Tumour of Tendon Sheath (GCT-TS) of Hands – An Institutional Experience. Orthop Surg Traumatol 2: 396-404.
- Noordin S, Allana S, Umer M, Jamil M, Hilal K, et al. (2018) Unicameral bone cysts: Current concepts. Ann Med Surg 34: 43–49.
- KaplanoÄŸlu V, Ciliz DS, KaplanoÄŸlu H, Elverici E (2014) Aneurysmal bone cyst of the calcaneus. J Clin Imaging Sci 14: 60.
- Sugiura H, Yamada K, Sugiura T, Hida T, Mitsudomi T (2008) Predictors of survival in patients with bone metastasis of lung cancer. Clin Orthop Relat Res 466: 729–736
- Negash BE, Admasie D, Biruk L, Wamisho, Mihiret W et al. (2009) Bone tumours ar Addis Ababa University, Ethiopia: agreement between radiological and histopathological diagnoses, a 5 year analysis at Black Lion Teaching Hospital. Int J Med Med Sci 1: 119-125.
Citation: Jeyaraman M, Ramesh R, Chaudhari K, Ajay SS, Mendiratta D, et al. (2019) Overview of Bone Tumours in a Tertiary Care Hospital. J Orthop Oncol 5: 130. DOI: 10.4172/2472-016X.1000130
Copyright: © 2019 Jeyaraman M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4719
- [From(publication date): 0-2019 - Nov 10, 2025]
- Breakdown by view type
- HTML page views: 3765
- PDF downloads: 954