Pancreatic Isle Cell Transplantation as a Treatment for Brittle Kind One Diabetes: A Case Report and Review of the Literature
Received: 01-Aug-2022 / Manuscript No. TROA-22-72914 / Editor assigned: 03-Aug-2022 / PreQC No. TROA-22-72914 / Reviewed: 17-Aug-2022 / QC No. TROA-22-72914 / Revised: 22-Aug-2022 / Manuscript No. TROA-22-72914 / Published Date: 27-Aug-2022 DOI: 10.4172/troa.1000148
Abstract
Purpose: To report a case of epithelium keratoplasties (EKs) performed in a very four month previous with a posterior polymorphous tissue layer dystrophy.
Observations: A four month previous baby underwent Descemet membrane epithelium plastic surgery (DMEK) for posterior polymorphous tissue layer dystrophy. The graft was found to be disjointed on day five post-operatively and an endeavor to unfold the DMEK scroll and re-bubble wasn't made. The patient was then treated with success with bilateral Descemet denudation machine-controlled epithelium plastic surgery (DSAEK). At three years of follow-up, her vision was 20/70 within the right and 20/60 within the left eye with sensible epithelium cell counts.
Conclusions and importance: This study reports the youngest case of EKs performed at the age of four months in associate degree baby. this is often additionally the primary reportable case of tried DMEK light its challenges in infants.DSAEK remains a decent treatment choice for epithelium pathology secondary to posterior polymorphous tissue layer dystrophy in infants even when failing DMEK.
Posterior polymorphous tissue layer dystrophy (PPCD) is one amongst the tissue layer epithelium dystrophies transmitted in associate degree chromosome dominantly manner. The clinical presentation of PPCD varies from symptomless tissue layer epithelium changes to non-heritable tissue layer puffiness, peripheral iridocorneal adhesions and eye disease. reconstructive surgery is needed in 20–25% of patients with PPCD WHO developed tissue layer puffiness.1Corneal puffiness caused by PPCD will have a large impact on the visual development of kids thanks to vision defect. so surgical interventions like reconstructive surgery is also thought of to revive tissue layer clarity and stop vision defect.
Keywords
Descemet membrane epithelium plastic surgery; Descemet epithelium plastic surgery; Posterior polymorphous tissue layer dystrophy; Infant
Introduction
The classic surgical procedure of PPCD has been penetrating plastic surgery (PKP). However, if the tissue layer clarity permits, full thickness transplantion has been outdated by partial thickness transplants. The procedure most generally applied currently for epithelium dystrophies is Descemet denudation machine-controlled epithelium plastic surgery (DSAEK). DSAEK involves transplant a skinny layer of stroma, Descemet's membrane and epithelium and has been with success performed in youngsters. In recent years, the technique of Descemet membrane epithelium plastic surgery (DMEK) has been developed, that involves transplant solely Descemet's membrane and epithelium. This system has shown potential for quicker and improved visual outcomes compared with DSAEK [1].
We report the case of associate degree baby with PPCD treated at the start with DMEK that was unsuccessful followed by made bilateral DSAEK. To the simplest of our information this is often the youngest case report of epithelium plastic surgery (EK) within the literature.
Case report
A 15-year-old Caucasian male given with progressive redness and pain of the left eye for five days. His pediatrist prescribed moxifloxacin ophthalmic resolution and oral penicillin at some point before presentation. Past ocular history was ordinary. Medical record was important for WAS. The patient was at the same time being managed by associate degree specialist for chronic sinus infections and undergoing iron infusion medical aid for iron-deficiency anemia [2].
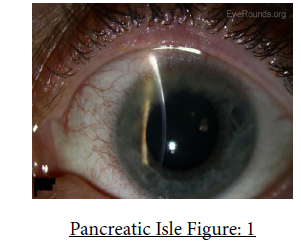
Uncorrected vision was 20/25 within the right eye and 20/25 within the left. On slit lamp examination, mixed anterior and posterior inflammation was gift in each eye with gentle flaking on the patient's lashes. No telangectatic vessels were noted. the correct tissue layer showed atiny low inferior pannus with non-injected mucous membrane. The mucous membrane of the left eye showed diffuse injection. The left tissue layer displayed five areas of ulceration of that three were situated superiorly and a couple of inferiorly (Figure 1). All ulcers stained with fluorescent dye. Each anterior chamber was quiet. The patient was diagnosed with tissue layer ulcers of the left eye, possibly thanks to associate degree enlarged susceptibleness and abnormal immunologic response to the common infectious agent coccus aureus related to chronic inflammation [3].
Treatment consisted of continuing topical moxifloxacin and oral Augmentin as preliminarily specified by the pediatrician. An expansive discussion took place with the case and his mother regarding lid hygiene practices. The authority to be used included warm compresses morning and night with good lid hygiene.
At the follow- up visit, the corneal ulcers had dropped in size with point staining along with quiet conjunctiva. Topical moxifloxacin and prednisolone acetate were phased and the ciprofloxacin ointment was continued. At 1 week follow- up, the ulcers were significantly bettered; still, supplemental corneal thinning was apparent. As the corneal thinning was attributed to the topical steroid, prednisolone acetate was discontinued and no farther thinning reenacted on follow- up examinations [4].
Two months latterly, the patient presented with greensickness and discomfort in the left eye of one days duration. The right eye remained quiet. The case was diagnosed with episcleritis of the left eye. Treatment comported of prednisolone acetate ophthalmic suspense twice a day; a lower cure due to the former corneal thinning noted. At follow- up 4 days latterly, the left eye's condition hadn't bettered and prednisolone acetate was increased to 1 drop four times daily. Posterior follow- up showed that the condition was markedly bettered and the drug was phased over the course of two weeks with no rush [5].
One week after the occasion of episcleritis resolved, the patient presented with a painful red right eye of 2 days duration. Vision remained unchanged. The conjunctiva of the right eye showed verbose injection more concentrated nasally. Tear beacon examination of the left eye was normal. Both anterior chambers were quiet. Treatment comported of prednisolone acetate ophthalmic suspense and moxifloxacin result both four times daily to the right eye. At follow- up 4 days latterly, the condition showed only slight enhancement and the case was asked to continue on the same drug course. At posterior follow- up, 5 days latterly, the condition was markedly bettered; the specifics were phased with no rush of the condition [6].
Discussion
This case report describes DMEK in a 4- month-old case with PPCD that was unprofitable due to detachment of the graft, followed by uncomplicated DSAEK in both eyes with good outgrowth. To our knowledge, this is the only DMEK case reported in a child, the youthful DSAEK treated case with PPCD in the literature with long term follow up on visual perceptivity and ECC and only the alternate report of DSAEK in PPCD in a child.
DMEK is arising as the keratoplasty of choice for the conditions which affect the endothelium. DMEK had a better visual perceptivity, achieved more snappily and with a better case satisfaction than DSAEK.13 also, the rejection rate is lower in DMEK than DSAEK.13 still, DMEK is a more demanding surgical fashion with advanced rate of graft disturbance Andre-bubbling as well as with further endothelial cell loss compared with DSAEK in early reports [7].
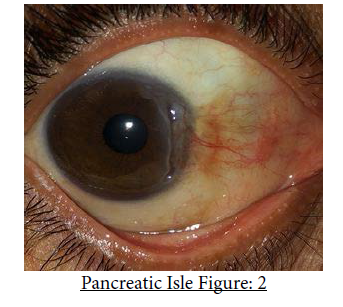
Endothelial keratoplasty is more grueling in children than grown-ups because of lower cornea size, shallower anterior chamber, phakic status, soft sclera and difficulties maintaining post-operative supine positioning. Likewise, any attempt atre-bubbling or indeed examination is delicate and may bear the use of general anesthesia. 15 reported the first case of successful DMEK in a 12 time old with Kearns- Sayre pattern and corneal edema. In this report the transplant remained clear 6 months after the surgery with a best- corrected vision of20/100. Our case is the alternate report of DMEK in children and the first reported in a child. Although our case had a good cornea size, deep anterior chamber and a technically uncomplicated DMEK procedure, graft disturbance and unprofitable-bubbling redounded in surgical failure [8]. Graft relegation in our case is less likely to be due to shy marshland of viscoelastic circulating in the anterior chamber because expansive marshland of cohesive viscoelastic was performed with confidence that it was all removed. A clear cornea and good outgrowth with posterior DSAEK was achieved in our case indeed though the overall postoperative corneal consistence(Figure 2)was still fairly high. There are only five reports including one series8 published in the literature of DSAEK in babies for CHED and PPCD with a followup from 3 to 24 months showing good graft survival without cataract conformation. Reported vision of20/40 at two times follow- up after DSAEK performed in a 8 month old case with CHED [9].
Posterior polymorphous corneal dystrophy is one of the corneal endothelial dystrophies with wide range of clinical donation. PPCD is generally an asymptomatic complaint with normal vision, unless there's asymmetric complaint, corneal edema, visual axis nebulosity or refractive error causing amblyopia at early age.16, 17 surgical operations similar as corneal transplant is needed when the threat of amblyopia is high.
Conclusion
Our single case doesn't allow any conclusions to be drawn regarding the DMEK fashion as a feasible option for babies. The eventuality for better visual perceptivity and lower rejection rate in children would be a major advantage of DMEK over DSAEK. It may be that unborn advances and adding moxie in DMEK leads to better outgrowth for children. It would be profitable to have ready access to hand held anterior SD- OCT and test under anesthesia to more assess DMEK adhesion and performer-bubbling procedure in babies. It's encouraging still, that good visual issues are attainable with posterior DSAEK, indeed if DMEK is unprofitable in babies [10].
Conflict of Interest
None. The authors have no financial exposures.
References
- Bolzano G, Maffi P, Nano R, Zerbi A, Venturini M, et al. (2013) Extending indications for islet autotransplantation in pancreatic surgery. Ann Surg 258: 210-218.
- Balzano G, Maffi P, Nano R, Mercalli A, Melzi R, et al. (2016) Autologous Islet Transplantation in Patients Requiring Pancreatectomy: A Broader Spectrum of Indications Beyond Chronic Pancreatitis. Am J Transplant 16:1812-1826.
- Chaouch MA, Leon P, Cassese G, Aguilhon C, Khayat S, et al. (2022) Total pancreatectomy with intraportal islet autotransplantation for pancreatic malignancies: a literature overview. Expert Opin Biol Ther 22: 491-497.
- Siegel M, Barlowe T, Smith KD, Chaidarun SS, LaBarre N, et al. (2020) Islet autotransplantation improves glycemic control in patients undergoing elective distal pancreatectomy for benign inflammatory disease. Clin Transplant 34: 13891.
- Tanhehco YC, Weisberg S, Schwartz J (2016) Pancreatic islet autotransplantation for nonmalignant and malignant indications. Transfusion 56: 761-770.
- Zureikat AH, Nguyen T, Boone BA, Wijkstrom M, Hogg ME, et al. (2015) Robotic total pancreatectomy with or without autologous islet cell transplantation: replication of an open technique through a minimal access approach. Surg Endosc 29: 176-183.
- Bhayani NH, Enomoto LM, Miller JL, Ortenzi G, Kaifi JT, et al. (2014) Morbidity of total pancreatectomy with islet cell auto-transplantation compared to total pancreatectomy alone. HPB (Oxford) 16: 522-527.
- Morgan KA, Nishimura M, Uflacker R, Adams DB (2011) Percutaneous transhepatic islet cell autotransplantation after pancreatectomy for chronic pancreatitis: a novel approach. HPB (Oxford) 13: 511-516.
- Jin SM, Oh SH, Kim SK, Jung HS, Choi SH, et al. (2013) Diabetes-free survival in patients who underwent islet autotransplantation after 50% to 60% distal partial pancreatectomy for benign pancreatic tumors. Transplantation 95: 1396-1403.
- Muratore S, Zeng X, Korc M, McElyea S, Wilhelm J, et al. (2016) Metastatic Pancreatic Adenocarcinoma After Total Pancreatectomy Islet Autotransplantation for Chronic Pancreatitis. Am J Transplant16: 2747-2752.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Gitman MR (2022) Pancreatic Isle Cell Transplantation as a Treatment for Brittle Kind One Diabetes: A Case Report and Review of the Literature. Transplant Rep 7: 148. DOI: 10.4172/troa.1000148
Copyright: © 2022 Gitman MR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3161
- [From(publication date): 0-2022 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 2613
- PDF downloads: 548