Pathogenesis and Treatment of Diabetic Gastro-Paresis Associated With Gastro-Paresis Cardinal Symptom Index and Health-Related Quality of Life
Received: 02-Mar-2022 / Manuscript No. JGDS-22-55894 / Editor assigned: 04-Mar-2022 / PreQC No. JGDS-22-55894(PQ) / Reviewed: 18-Mar-2022 / QC No. JGDS-22-55894 / Revised: 23-Mar-2022 / Manuscript No. JGDS-22-55894(R) / Published Date: 30-Mar-2022 DOI: 10.4172/2161-069X.1000674
Abstract
The review covers the pathophysiology and treatment aspects of the diabetes gastro-paresis. Diabetic gastro-paresis is a clinical ailment characterized by delayed gastric emptying in the non-appearance of mechanical hindrance of the stomach linked with cardinal symptoms, like nausea, vomiting, postprandial fullness, early satiety, and bloating. Diabetic gastro-paresis (DG) affects patient population with long established diabetes mellitus. Delayed gastric emptying in patients suffering from diabetes mellitus may lead to badly off glycemic control, malnutrition and dehydration, which in turn may result in poor quality of life (QOL), recurrent hospitalization and dropping productivity and is linked with higher morbidity rate and mortality rate because of difficulty in reaching glucose control. The gold standard or ideal technique for estimating gastric emptying rate is by gastric scintigraphy. Although, this technique needs specialized expensive equipment and inflicts low but measurable radiation exposure. So, it is sensible to pre-select diabetic patient population for gastric scintigraphy based on symptoms the patients are experiences. A newly evolved validated symptom severity instrument or scale (GCSI), for utilization in gastro-paresis clinical research studies, which is on the upper gastrointestinal symptoms a patient experience. The GCSI (Gastro-paresis Cardinal Symptom Index) was developed as part of a large patient population outcomes project, development of the (PAGI-SYM) Patient Assessment of Upper Gastrointestinal Disorders Symptom Severity Index. Numerous studies indicated that the females generally have a slower solid and liquid GER (Gastric Emptying Rate) than the males. The root mechanism for this phenomenon is not completely understood and may be related to estrogen levels in patients. Age, BMI, duration of diabetes, FBG, HbA1c and gender were incriminated in the gastro-paresis research studies. It was seen in research studies that the study participants (subjects) have the presence of at least one gastro-paresis symptom. The bad glycemic control, hyperglycemia and high duration of diabetes mellitus were the significantly linked with the factors and quality of life (QOL) in diabetes patients.
Keywords: GCSI; Cardinal symptoms; Quality of life; Diabetes mellitus; Qiabetic gastro-paresis; Gastro-paresis Symptoms; Idiopathic gastro-paresis; Gastro-paresis treatment; Pathogenesis
Introduction
The alliance between delayed gastric emptying and diabetes mellitus has been known for a century now. Delayed gastric emptying was first observed in patients with diabetes and reported by Boas in 1925 [1]. The symptoms like nausea and vomiting are the two prevalent symptoms in Gastro-paresis patients. Abdominal pain is getting recognized as the third most common symptom as well, with some studies reporting abdominal pain in 90% of their sample size [2]. Patients with established diabetes mellitus diagnosed with diabetic gastro-paresis usually disturbed by retinopathy, neuropathy and nephropathy in their life [1].
Diabetic gastro-paresis is a clinical syndrome characterized by delayed or abnormal gastric emptying in the void of mechanical obstruction of the stomach associated with symptoms like nausea, vomiting, postprandial fullness, early satiety and bloating. Most familiar etiologies include diabetes, postsurgical and post-infectious, but in many cases it is found idiopathic. Clinical sign and symptoms and natural history differ by the etiology. There is significant morbidity found and healthcare expenditure associated with gastro-paresis. Mechanistic studies from diabetic animal models of delayed GE as well as human full thickness biopsies have notably advanced our perception of this disorder [3]. As much as 50% of patients with type 1 and type 2 DM and suboptimal glycemic control have delayed gastric emptying (GE), which can be written with scintigraphy, 13C breath tests, or a wireless motility capsule; the remaining have normal or fast gastric emptying. Many patients with delayed Gastric Emptying are not symptomatic but some others have dyspepsia (i.e., mild to moderate indigestion issues, with or without a mild delay in GE) or gastro-paresis, which is a syndrome, characterized by moderate to severe upper gastrointestinal symptoms and delayed Gastric Emptying that indicate, but are not escorted by, gastric outlet obstruction. Gastro-paresis can strongly disturb quality of life, and up to 50% of patient population has crucial anxiety and/or depression. Most of the time differentiation between dyspepsia and gastro-paresis is based on clinical judgment rather than suggested criteria [4]. The 3 main reasons are diabetic, postsurgical, and idiopathic. Final diagnosis is established by demonstrating delayed gastric emptying. Gastric emptying rates measured by gastric motor testing generally correlate very less with symptoms and quality of life in patients suffering from gastro-paresis [5].
Gastro-paresis should be considered in finding out the final diagnosis of a patient suffering from these symptoms after mechanical and structural lesions have been rule out [6]. Symptoms of gastro-paresis are nonspecific, including nausea, vomiting, early satiety, bloating, and/or abdominal pain. Ideally gastric motor function and sensory function depend on a complex systematization between the enteric and central nervous system. The pathogenesis of delayed gastric emptying and the symptoms of gastro-paresis, includes antropyloroduodenal dysmotility, impaired gastric accommodation, visceral hypersensitivity, and autonomic dysfunction all together contribute to the pathogenesis. The underlying pathophysiology of gastro-paresis is complex and is the result from many different factors [7]. Considering that Idiopathic gastro-paresis (IG) is an ordinary but poorly understood condition with highly significant morbidity. The mean age of patients with IG studied in a study was 41 years in which 88% were females, 46% patients were overweight, 50% of patients had acute onset of symptoms, and 19% patients reported an initial infectious prodrome. Drastic delay in gastric emptying (>35% retention at 4 hours) was observed in 28% of patients in a study in 2010. Predominant presenting symptoms were nausea (34%), vomiting (19%), an abdominal pain (23%) was also observed. Women patients had more acute nausea, satiety, constipation, and overall gastro-paresis symptoms. Patients in the study who experienced acute onset IG had worse nausea than those with subtle onset. Overweight patients or patients with obesity had more bloating and gastric retention at 2 hours but less severe loss of appetite was observed in the study by the clinicians [8].
A study shows that African American patient’s population with gastroparesis like symptoms were more likely to suffer from diabetic gastro-paresis than patients or population of other races (P=0.01) in two thousand twenty one. Among a large urban population of different races, patients with delayed gastric emptying do carry comorbid conditions that can be considered as risk factors for the development of gastro-paresis, including prescriptions for narcotic medication. Significantly larger numbers of these comorbid conditions are assessed as more severe disease condition. Demographics are mostly associated with the etiology and severity of gastroparesis in particular, African American patients are more likely to suffer from diabetic gastro-paresis than patients of other races as assessed by the researchers [9-16].
Pathogenesis
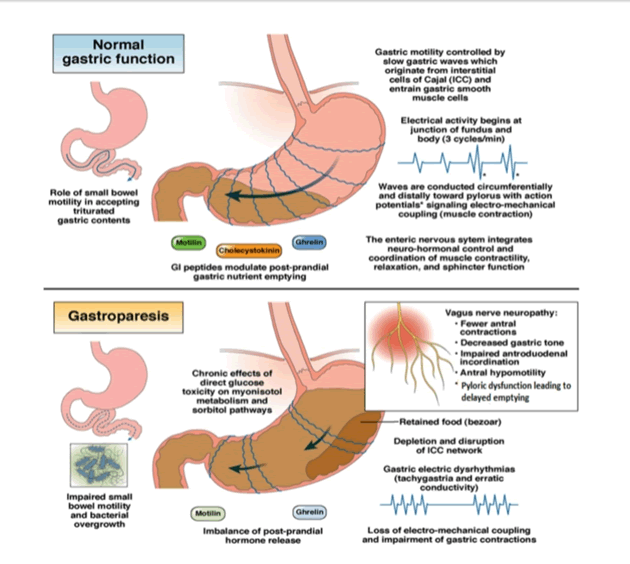
In spite of the fact that the mechanism of gastric dysfunction and symptom generation in Diabetic gastro-paresis is untold, a list of contributing factors have been offered, vagal dysfunction, counting hyperglycemia, loss of neural nitric oxide synthase expression in the myenteric plexus, ICC network disturbances and oxidative stress (Figure 1).
An acute change in blood glucose levels (double or half of the normal blood glucose level, 4 mmol/l) may end in respectively very much delayed or increased gastric emptying. Delayed or accelerating gastric emptying by diabetic gastro-paresis patients can come up with fluctuations in their blood glucose that can later on impair the gastric emptying rate, thus generating a vicious circle for the patient population. Delayed emptying of stomach can be due to the pyloric contractions and antral hypomotility persuaded by the hyperglycemic state. Hypoglycemia is a major cause that can also excite the vagal nerve that can lead to a major change in gastric emptying rate. It is vague however whether chronically increased blood glucose levels have effects of similar magnitude on gastric emptying. As in the case of other diabetic complications, strictly control on blood glucose is the best prevention. Regrettably, once gastric function is severely compromised or deviated, generally strict control may become difficult [17].
Vagal dysfunction has also been suggested to play a significant role in Diabetic gastro-paresis. When food is ingested and gastric accommodation is spoiled, subjects may feel symptoms such as untimely satiation, discomfort and fullness. Human and animal data propose that vagal neuropathy can finishes in depletion in impaired antral contraction, pyloric relaxation and disturbed antropyloric coordination. This concludes vagal neuropathy a significant contender mechanism underlying disturbed gastric emptying and symptom generation in Diabetic gastro-paresis.
ENS deformities also play a major role in Diabetic gastro-paresis pathogenesis. A significant constituent of the ENS is the myenteric plexus, a number of nerves that is superimposed between the longitudinal and circular muscle layer of the gastrointestinal tract and synchronizes gastric motor function. The myenteric plexus involves excitatory (purinergic and cholinergic) and inhibitory motor neurons, also primary afferent neurons and many classes of interneurons. The excitatory motor neurons give rise to muscle contractions through release of neurotransmitters like acetylcholine and substance P, while on the contrary the inhibitory neurons will relax the muscle tissue through release of nitric oxide (NO) and as well as ATP and vasoactive intestinal peptide. Pathologic switches in these pathways, mainly the nitergic nerves that will affect motor control and may lead to issues like delayed emptying, gastric dysrhythmia and impaired accommodation.
Treatment
About treatment of gastro-paresis, electrical stimulation and gastric pacing are an evolving treatment option for patients who do not respond to medical regimen [10].
Electric Stimulation is a non-pharmacological therapy for patients with medication resistant gastro-paresis. Gastric electric stimulation has evolved over the few decades. Depend on the frequency of the electrical stimulus, gastric electric stimulation can be divided into low and high frequency gastric electric stimulation. The first method goals to normalize gastric dysrhythmia and entrain gastric slow waves and accelerates gastric emptying, whereas high frequency gastric electric stimulation is unable to restore normal gastric emptying, but nevertheless stunningly reduces symptoms, such as vomiting, nausea and, re-establishes quality of life, nutritional state in all patients, and metabolic control in patients with diabetic gastro-paresis. Gastric electric stimulation presents a new possibility in the treatment of gastro-paresis [11].
One of the studies used the GCSI to monitor symptoms of the suffering individuals and during follow up evaluation. In the description of the GCSI, a decline in symptom severity of 0.75 points in the mean GCSI total score was taken as improvement in clinical representation by physicians as well as individuals. However, many studies using larger numbers of gastro-paresis patients and an interventional arm have suggested that this number may be too low [12] (Table 1).
Table 1: Gastroparesis severity.
| Grade 1 | Grade 2 | Grade 3 |
|---|---|---|
| Mild Gastric Neuromuscular Dysfunction Symptoms relatively easily controlled by the person. | Compensated Gastric Neuromuscular Dysfunction Moderate symptoms with partial control are present. | Chronic Gastric Failure Refractory symptoms are present. |
| Can maintain weight and nutrition on a regular basis diet plan. | Can maintain nutrition with diet plan and lifestyle adjustments. | Inability of the person to maintain nutrition in body via oral route of administration. |
Gastro-paresis has few treatment options for management and cure. Relamorelin is one of the drugs used to decrease the symptoms of gastroparesis in diabetes patients with safety and it is well tolerated by diabetic patients. It is a pro-kinetic agonist of ghrelin; hence it can be given to Grade 2 and Grade 3 category patients. [13].
Discussion
It has been estimated that prevalence of gastro-paresis due to frequent use of drug metformin by diabetic patients is 6% in Saudi adults. Therefore, it can affect the patient’s quality of life very badly and patients will feel low while confidently tackling to their problems. The symptomatic screening is a must for these patients and also the use of metformin must be regulated by the patient or the patient’s family [14].
Gastric peroral endoscopic myotomy (G-POEM) is also considered as a potential treatment alternative for diabetic gastro-paresis [15]. Patient Assessment of Upper GI Symptoms (PAGI-SYM) questionnaire assesses symptoms suggestive of gastro-paresis on the basis of the response given by the diabetic patient and his/her discomfort and after that scores and sub-scores are measured. Patient is assessed by Upper Gastrointestinal Disorders Quality of Life (PAGI-QOL) survey for disease specific Quality of Life. Tricyclic antidepressants, Anti-emetics, Neuropathic pain modulators, Pro-kinetics, Narcotic pain medications are some of the frequently medication used by the gastro-paresis patient. Neuropathy, Migraine, Fibromyalgia, Cholecystectomy, Inflammatory Bowel Syndrome is other pain related conditions faced by the suffering patients. It has been observed that abdominal pain is the most common symptom reported by the gastro-paresis patients. Abdominal pain is mostly reported as severe on the basis of GCSI score [16].
Conclusion
As we have discussed about the treatment options and how it affects the quality of life of the diabetic patients learning more about the diabetic gastro-paresis pathogenesis and treatment options can lead to a significant change in the patient’s life and can help clinical researchers significantly in finding or discovering better treatment options for diabetic gastro-paresis disorder. Newer treatment options can change the world for the needy patients who are unable to experience relief from present treatment options or modifications of present treatment options can be considered for those. Understanding patient’s pathology is equally important for physicians or care givers in order to provide best patient care and treatment to the suffering patients. GCSI score can help the physicians in assessing the exact condition of the particular patient and for providing individualized treatment option and care in each case.
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
References
- Krishnasamy S, Abell TL (2018) Diabetic gastroparesis: Principles and current trends in management. Diabetes Ther 9:1-42.
[CrossRef] [Google Scholar] [Pubmed]
- Liu N, Abell T (2017) Gastroparesis updates on pathogenesis and management. Gut Liver 11(5):579-589.
[CrossRef] [Google Scholar] [Pubmed]
- Grover M, Farrugia G, Stanghellini V (2019) Gastroparesis: A turning point in understanding and treatment. Gut 68(12):2238-2250.
[CrossRef] [Google Scholar] [Pubmed]
- Bharucha AE, Kudva YC, Prichard DO (2019) Diabetic Gastroparesis. Endocr Rev 40(5):1318-1352.
[CrossRef] [Google Scholar] [Pubmed]
- Pasricha PJ, Parkman HP (2015) Gastroparesis: Definitions and diagnosis. Gastroenterol Clin North Am 44(1):1-7.
[CrossRef] [Google Scholar] [Pubmed]
- Hornbuckle K, Barnett JL (2000) The diagnosis and work-up of the patient with gastroparesis. J Clin Gastroenterol 30(2):117-124.
[CrossRef] [Google Scholar] [Pubmed]
- Nguyen LA, Snape WJ Jr (2015) Clinical presentation and pathophysiology of gastroparesis. Gastroenterol Clin North Am 44(1):21-30.
[CrossRef] [Google Scholar] [Pubmed]
- Parkman HP, Yates K, Hasler WL (2011) Clinical features of idiopathic gastroparesis vary with sex, body mass, symptom onset, delay in gastric emptying, and gastroparesis severity. Gastroenterology 140(1):101-115.
[CrossRef] [Google Scholar] [Pubmed]
- Duffey K, Hannon M, Yoo J (2020) The impact of risk factors on gastroparesis at an urban medical center. Ann Gastroenterol 33(3):250-256.
[CrossRef] [Google Scholar] [Pubmed]
- Ali T, Hasan M, Hamadani M, Harty RF (2007) Gastroparesis. South Med J 100(3):281-286.
[CrossRef] [Google Scholar] [Pubmed]
- Monnikes H, van der Voort IR (2006) Gastric electrical stimulation in gastroparesis: where do we stand? Dig Dis 24(4):260-266.
- Pasricha PJ, Yates KP, Nguyen L (2015) Outcomes and factors associated with reduced symptoms in patients with gastroparesis. Gastroenterology 149(7):1762-1774.
[CrossRef] [Google Scholar] [Pubmed]
- Camilleri M, McCallum RW, Tack J, Spence SC, Gottesdiener K, et al. (2017) Efficacy and Safety of relamorelin in diabetics with symptoms of gastroparesis: A randomized, placebo-controlled study. Gastroenterology 153(5):1240-1250.
[CrossRef] [Google Scholar] [Pubmed]
- AlOlaiwi LA, AlHarbi TJ, Tourkmani AM (2018) Prevalence of cardiovascular autonomic neuropathy and gastroparesis symptoms among patients with type 2 diabetes who attend a primary health care center. PLoS One 13(12):e0209500.
- Xu J, Chen T, Elkholy S, Xu M, Zhong Y, et al. (2018) Gastric Peroral Endoscopic Myotomy (G-POEM) as a treatment for refractory gastroparesis: Long-term outcomes. Can J Gastroenterol Hepatol 2018:6409698.
[CrossRef] [Google Scholar] [Pubmed]
- Parkman HP, Wilson LA, Hasler WL, McCallum RW, Sarosiek I, et al (2019) Abdominal Pain in patients with gastroparesis: Associations with gastroparesis symptoms, etiology of gastroparesis, gastric emptying, somatization, and quality of life. Dig Dis Sci 64(8):2242-2255.
[CrossRef] [Google Scholar] [Pubmed]
- Oh JH, Pasricha PJ (2013) Recent advances in the pathophysiology and treatment of gastroparesis. J Neurogastroenterol Motil 19(1):18-24.
[CrossRef] [Google Scholar] [Pubmed]
Citation: Shivaji DR, Malik N (2022) Pathogenesis and Treatment of Diabetic Gastro-Paresis Associated With Gastro-Paresis Cardinal Symptom Index and Health-Related Quality of Life. J Gastrointest Dig Syst.12:674 DOI: 10.4172/2161-069X.1000674
Copyright: © 2022 Shivaji DR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4502
- [From(publication date): 0-2022 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 3779
- PDF downloads: 723