Pelvic Girdle Myopathy Caused by Isotretinoin: Case Report and Discussion of Pathophysiology
Received: 15-Jan-2014 / Accepted Date: 11-Feb-2014 / Published Date: 13-Feb-2014 DOI: 10.4172/2161-0681.1000160
Abstract
Introduction: Isotretinoin is the mainstay therapy for severe and nodulocystic acne. Myalgia and muscle stiffness have been reported in 16-51% of patients treated with isotretinoin, while elevated serum Creatine Kinase (CK) levels have been found in up to 41%. In this paper, we report, for the first time, the occurrence of myopathy limited to the pelvic-girdle muscles in a teen who received isotretinoin therapy.
Methods: This was a case study conducted at King Khalid Hospital.
Results: Histopathology and other laboratory data were consistent with an inflammatory myopathy based on a vasculitic process.
Conclusion: Our data indicate that the myopathy caused by isotretinoin is an inflammatory process based on vasculitis, resulting in ischemic muscle necrosis.
Introduction
Isotretinoin is the mainstay therapy for severe and nodulocystic acne. Myalgia and muscle stiffness have been reported in 16-51% of patients treated with isotretinoin, while elevated serum Creatine Kinase (CK) levels have been found in up to 41% [1,2]. Furthermore, it has been suggested that exercise in patients receiving isotretinoin may trigger increased serum CK levels [3]. There have been several reports of severe and debilitating muscular symptoms due to isotretinoin where CK levels were normal [4,5]. In such patients, myopathy or a disorder of myoneural junction was suggested by muscle biopsy. Queries regarding the clinical significance of elevated CK in isotretinoin-treated acne patients had already been made as early as mid- 1980’s [6], but no satisfactory answers have been given so far. In this paper we report, for the first time, the occurrence of severe pelvic girdle myopathy caused by isotretinoin. We also discuss the pathophysiological mechanisms of this myopathy.
Case Report
A 14-year-old Saudi male came to the outpatient clinic on Feb 22, 2012 with lower limb weakness and lower back pain.
He had a history of nodulocystic acne vulgaris for which he had been taking Isotretinoin for 1 month. Two weeks prior to the outpatient visit he began to notice muscular aches which prompted the attending dermatologist to discontinue the isotretinoin and make a referral to neurology.
Birth history revealed that he was born with a right Erb’s palsy. General physical examination was normal. The patient was alert. He had reached his expected developmental milestones. Vital signs were normal. Nodulocystic acne was present.
Neurological examination showed normal cranial nerves. Evaluation of the motor system showed weakness of shoulder abduction, external rotation, forearm flexion and supination on the right consistent with congenital Erb’s palsy. In the lower extremities there was weakness of glutei and adductors of the thighs resulting in a waddling gait. There was also moderate weakness of quadriceps femoris bilaterally. There was no atrophy and no fasciculation’s. Deep tendon reflexes were 2 plus bilaterally and symmetrically. There were no Hoffmann’s or Babinski’s. Sensation and cerebellar functions were normal.
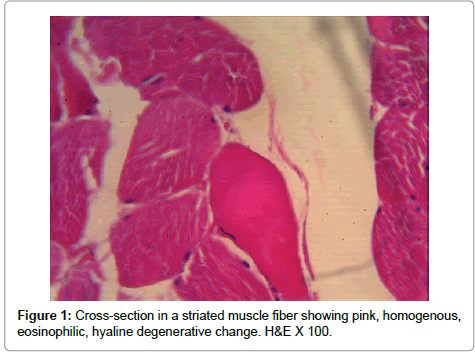
Laboratory studies showed normal blood chemistry with slightly increased LDH (258 u/L), CK of 80 u/L (normal), ESR of 85 MM/HR, negative CRP and a normal thyroid profile. There were no ANA or anti-DNA antibodies detected. MRI of the lumbar spine showed no abnormalities. An EMG of the left gluteus maximus and rectus femoris showed a normal recruitment pattern, Individual motor unit potentials were low in amplitude and short in duration, consistent with myopathy. There were no denervation potentials. Muscle biopsy taken from right upper thigh (H&EX 100) showed pink, homogeneous, eosinophilic, non-specific hyaline degenerative changes with opaque cytoplasm. Sarcolemmal membrane showed large and vesicular nuclei (Figure 1).
The patient received physical therapy, and made a remarkable recovery within the ensuing weeks.
Discussion
Isotretinoin, 13-cis-retinoic acid, is a retinoid which is quite effective in the treatment of acne vulgaris [7]. It counteracts the pathogenic factors that contribute to the development of acne [8]. Myalgia occurs in up to 15% of patients who are treated with isotretinoin [9]. This can be associated with elevated Creatine Phosphokinase levels (CK), especially after intense exercise. By-and-large, the severity of muscle involvement and the CPK levels are not concordant in isotrenointreated patients (Kamak). For example, it is not unusual to find seemingly asymptomatic patients despite a significantly elevated CK in this population. In the trials in which information about muscle aches and pains were solicited, the pain did not require discontinuation of the drug, and a simple analgesic was sufficient to alleviate the symptoms in most patients [10]. Paradoxically, a single case report of rhabdomyolysis during isotretinoin therapy has been published [11].
Muscle injury causes depletion of ATP and/or rupture of plasma membrane, and the latter may even enhance ATP depletion. ATP depletion leads to dysfunction of Na/K-ATPase andCa2-ATPase pumps resulting in myocyte injury and the release of entocytes (CPK and other muscle enzymes, myoglobin, and various electrolytes) into the circulation. Even though rhabdomyolysis is multifactorial, the final common pathway for muscle injury is an increase in intracellular free ionized cytoplasmic and mitochondrial calcium caused by ATP depletion. The increased intracellular calcium leads to activation of protease, increased skeletal muscle cell contractility, mitochondrial dysfunction, and the production of reactive O2 species resulting in necrosis (Zhang, Miller). Etiology of rhabdomyolysis is manifold ranging from traumatic causes (e.g. crush injuries) to nontraumatic causes (e.g. strenuous exercises, metabolic myopathies and hyperthermia) and non-traumatic non-exertional factors (e.g. drugs, toxins, viral/bacterial infections, electrolyte disorders, inherited disorders of metabolism).
It has been theorized that all therapeutic as well as adverse effects of isotrenoin are caused by “proapoptotic mechanisms” mediated by forkhead box O (Fox O) and its isoforms (Melnik). The latter are proteins that are involved in regulating gene expression in a variety of conditions including inflammatory and immune-mediated processes.
Several cases of systemic vasculitis have been linked to isotretinoin therapy [12,13]. In our patient histopathology showed hyaline degenerative changes consistent with inflammatory myopathy which in this case was caused by isotretinoin. The absence of inflammatory cells on the muscle biopsy does not rule out an inflammatory process [14]. Moreover, the ESR/ CRP dissociation (elevated ESR despite a negative CRP) is consistent with vasculitis [14]. Thus, we believe that the myopathy in our patient was inflammatory on a vasculitic basis, resulting in ischemic muscle necrosis. The fact that tissue findings were disproportionately mild signifies a patchy distribution of the ischemic muscle lesions, consistent with vasculitis. At this time we are unable to reconcile our proposed pathogenic mechanism of isotretinoin-induced myopathy with the Fox O theory. In other words, the question remains as to how “up-regulation” of Fox O with its “anti-inflammatory” properties could paradoxically induce an “inflammatory” myopathy.
Several measures for the treatment of isotretinoin-induced myopathy have been suggested including dose reduction, temporary medication suspension, and the use of L-carnitine (Natural Medicines). Due to the inflammatory nature of our patient’s myopathy, we could have elected to treat the patient with immunosuppressants or immunomodulating agents, however, because of lack of data in the literature we decided against this treatment strategy. Future studies of similar cases should address the potential role of these agents in the treatment of this type of iatrogenic myopathy.
Conclusion
Our patient developed severe pelvic girdle myopathy during isotretinoin therapy. Our data indicate that the myopathy caused by isotretinoin is an inflammatory process based on vasculitis. Our data also suggest that immunosuppressants or immunomodulating agents may have a place in the treatment of this type of myopathy.
References
- Heudes AM, Laroche L (1998) [Muscular damage during isotretinoin treatment]. Ann Dermatol Venereol 125: 94-97.
- McBurney EI, Rosen DA (1984) Elevated creatine phosphokinase with isotretinoin. J Am Acad Dermatol 10: 528-529.
- Hodak E, Gadoth N, David M, Sandbank M (1986) Muscle damage induced by isotretinoin. Br Med J (Clin Res Ed) 293: 425-426.
- Fiallo P, Tagliapietra AG (1996) Severe acute myopathy induced by isotretinoin. Arch Dermatol 132: 1521-1522.
- Chen D, Rofsky HE (1985) Elevated CPK and isotretinoin. J Am Acad Dermatol 12: 582-583
- Kapadia N, Khalid G, Burhany T (2003) 13-cis retinoic acid (Ro acutance) a miracle drug in nodulocystic acne. Ann Abbassi Shaheed Hospital, Karachi 8: 432-434.
- Ward A, Brogden RN, Heel RC, Speight TM, Avery GS (1984) Isotretinoin. A review of its pharmacological properties and therapeutic efficacy in acne. Drugs 28: 6-37.
- PDR Staff (1999) Isotretinoin. In: PDR Staff, editor. Physicians' Desk Reference. New Jersey: Medical Economics Co, 2651-2653.
- McLane J (2001) Analysis of common side effects of isotretinoin. J Am Acad Dermatol 45: S188-194.
- Trauner MA, Ruben BS (1999) Isotretinoin induced rhabdomyolysis? A case report. Dermatol Online J 5: 2.
- Aractingi S, Lassoued K, Dubertret L (1990) Post-isotretinoin vasculitis. Lancet 335: 362.
- Chochrad D, Langhendries JP, Stolear JC, Godin J (1997) Isotretinoin-induced vasculitis imitating polyarteritis nodosa, with perinuclear antineutrophil cytoplasmic antibody in titers correlated with clinical symptoms. Rev Rhum Engl Ed 64: 129-131.
- Kiely PD, Heron CW, Bruckner FE (2003) Presentation and management of idiopathic inflammatory muscle disease: four case reports and commentary from a series of 78 patients. Rheumatology (Oxford) 42: 575-582.
Citation: Janati A, Naif AG, Ghorbel S, Al-Emadi BA, Al-Shurtan KS, et al. (2014) Pelvic Girdle Myopathy Caused by Isotretinoin: Case Report and Discussion of Pathophysiology. J Clin Exp Pathol 4:160. DOI: 10.4172/2161-0681.1000160
Copyright: © 2014 Ghorbel S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 17657
- [From(publication date): 3-2014 - Aug 29, 2025]
- Breakdown by view type
- HTML page views: 12942
- PDF downloads: 4715