Polycystic Disease of the Pancreas: A Case Report
Received: 29-Jan-2018 / Accepted Date: 08-Feb-2018 / Published Date: 15-Feb-2018 DOI: 10.4172/2161-069X.1000552
Abstract
Polycystic disease of the pancreas is a rare disease most often seen in association with polycystic kidney disease and Von Hippel Lindau syndrome. It is characterized by the presence of single or multiple simple congenital cysts in the pancreatic parenchyma secondary to developmental defects. These cysts are benign in nature and do not communicate with the main pancreatic duct. We report a case of an elderly male with autosomal dominant polycystic kidney disease incidentally detected to have multiple simple pancreatic cysts.
Keywords: Pancreatic cysts; Polycystic disease; Von Hippel Lindau disease
Introduction
The estimated prevalence of asymptomatic pancreatic cyst is 2.2% on computed tomography and 19.6% on magnetic resonance imaging (MRI) [1,2]. Pseudocysts and cystic neoplasms of the pancreas such as serous cystadenoma, mucinous cystadenoma and intraductal pseudopapillary mucinous neoplasm constitute more than 95% of the pancreatic cysts. However, rarely cysts in the pancreas can be due to the developmental defects causing sequestration of pancreatic ducts leading to the formation of polycystic pancreas [3].
Polycystic disease of the pancreas (PDP) is a rare condition which mimics pseudocyst and cystic neoplasm of pancreas on radiological imaging. The exact incidence of this disease is not known. It has been found to be associated with polycystic kidney disease (ADPKD), cystic fibrosis and Von Hippel Lindau (VHL) syndrome [4-6]. In most of the cases, these cysts are asymptomatic [3]. However, if they are large in size, then can lead to symptoms secondary to compression of surrounding structures such as the main pancreatic duct, stomach [3,4]. We report a case of an elderly male with an incidental diagnosis of PDP in association with ADPKD.
Case Report
A 83-year-old gentleman presented with chief complaints of loose stools and generalized weakness for one month. Physical examination was unremarkable. Colonoscopy revealed few small superficial ulcers in the terminal ileum. Biopsy from these ulcers showed nonspecific ileitis. Ultrasound of the abdomen suggested cystic lesion of 19 × 14 mm in the head and uncinate process of the pancreas.
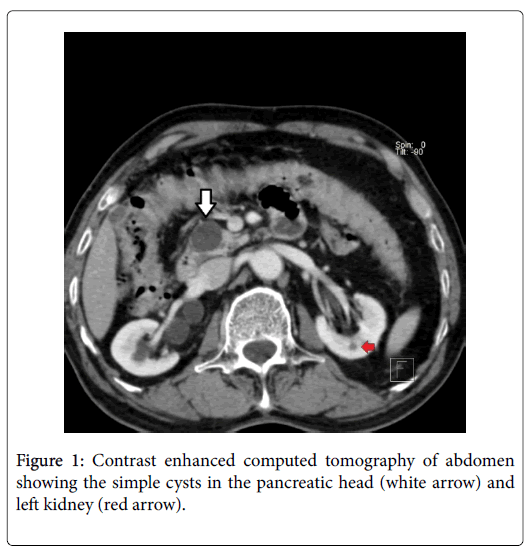
Contrast-enhanced computed tomography of the abdomen showed the presence of multiple cysts throughout the pancreas with largest measuring 2.2 × 1.7 × 2.1 cm located in the head and uncinate process. There was no calcification, fat density or enhancing soft tissue component seen within the cysts. Rest of the pancreas was normal in outline and attenuation pattern. The main pancreatic duct was not dilated (Figure 1).
In addition, multiple bilateral small renal cysts (5 cysts in each kidney) (Bosnaik type 1) and small ureteric calculi (3 mm on the right side and 1.9 mm on the left side) were present. A small 5 mm cyst was located in the segment II of the liver. Magnetic resonance imaging of the abdomen confirmed the presence of cysts in the liver, pancreas and kidneys.
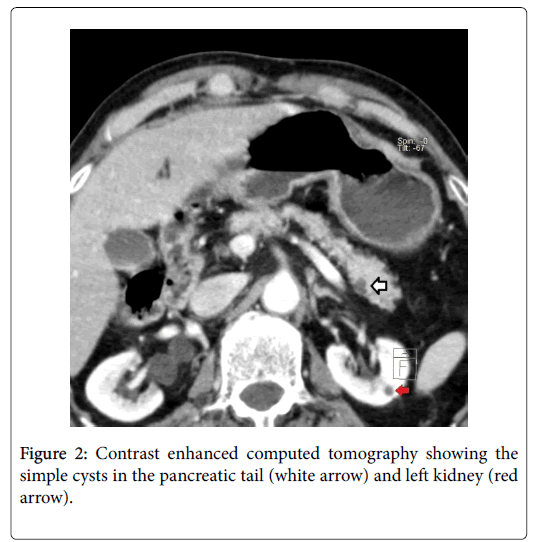
These pancreatic cysts exhibited hypointense peripheral and hyperintense central signals on T2WI while peripheral isointense and central hypointense signals on T1WI sequences. There was no evidence of septations or calcification within these cysts. These cysts were located in the head, uncinate process, body and tail of the pancreas (Figure 2)
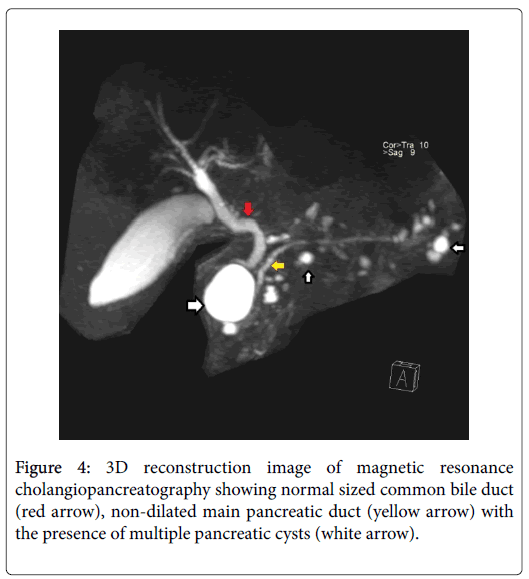
Rest of the pancreas was normal with the main pancreatic duct diameter of 1.7 mm. There was no evidence of communication between the cysts and the main pancreatic duct. Tumor markers (CA 19-9 and CEA) were normal.
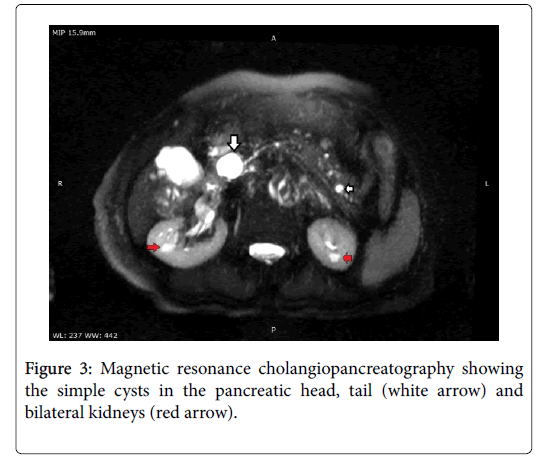
In view of the above findings and ultrasonographic diagnostic criteria for ADPKD [7], diagnosis of ADPKD with co-existent pancreatic and hepatic cysts was made. The patient was treated medically for loose stools and was symptom free till the last follow up at one month (Figures 3 and 4).
Discussion
Polycystic pancreas occurs due to abnormal development of pancreatic ductal system secondary to ciliopathy [3,8,9]. Recent studies have revealed that deficiency of hepatocyte nuclear factor 6, and gain of function of Forkhead box-containing protein predisposes to the development of pancreatic cysts [8,9]. These cysts lack primary cilia similar to that seen in ADPKD [3].
Radiological it is difficult to differentiate congenital cysts from pseudocysts. But unlike congenital cysts, pseudocysts have amylaserich fluid. Hence, cyst fluid analysis along with history of pancreatitis can help in making the diagnosis. On the other hand, malignant pancreatic cysts usually have intramural nodules, thickened irregular cyst wall, enhancing septae, main pancreatic duct dilatation or calcifications which help to differentiate them from congenital cysts. In the present case, none of the above-mentioned features were present. Hence, the diagnosis of the simple congenital cyst was made.
Pancreatic cysts have been most commonly found to be associated with ADPKD [4,5]. Although pancreatic cysts have been observed in patients with both PKD1 and PKD2 gene mutations, patients of PKD2 gene mutation are five times more likely to have pancreatic cysts [5]. Patients with PKD1 gene mutation have a single pancreatic cyst in about 75% cases with those with PKD2 gene mutation have two or more pancreatic cysts in more than 60% cases [5]. The size and distribution of cysts in patients with ADPKD are similar to those seen in patients without ADPKD.
Pancreatic cysts have also been found to be associated with VHL [6]. VHL is an autosomal dominant disease with the occurrence of 1 in 36000 live births and 90% penetrance by 65 years of age [10]. The mean age of detection of pancreatic cyst is 36 years [10]. In VHL, although the presence of simple pancreatic cyst is the most frequent pancreatic manifestation (88%), there can be the presence of associated complex cystic or solid enhancing masses in the pancreas [4]. In most of the VHL cases, two or more pancreatic cysts are found.
Due to its benign nature, asymptomatic PDP with or without ADPKD do not require surgery or surveillance as seen in our case. However, the patients of PDP with VHL require regular radiological surveillance as they are likely to develop other complex cystic or solid masses during follow up [4]. Symptomatic pancreatic cysts can be treated by deroofing or resection. Pancreatic cysts with suspicion of malignancy should be resected.
Conclusion
PDP is a rare disease which should be included in differential diagnosis while evaluating a patient with pancreatic cysts. It is most frequently associated with ADPKD or VHL. Radiological imaging and cyst fluid analysis are very useful in differentiating these congenital cysts from pseudocyst and cystic pancreatic neoplasm.
Author Contributions
Piyush Verma, Rahul Gupta, Arvind K Singh and Kewal Mistry collected data. Rahul Gupta, Arvind K Singh and Piyush Verma drafted the manuscript. Kewal Mistry and Pradip Pokharia edited the manuscript and figures. All the authors read and approved the final manuscript.
Conflict of Interest
The authors declare no conflict of interest.
References
- Zanini N, Giordano M, Smerieri E, Cipolla d'Abruzzo G, Guidi M, et al. (2015) Estimation of the prevalence of asymptomatic pancreatic cysts in the population of San Marino. Pancreatol 15: 417-422.
- Moris M, Bridges MD, Pooley RA, Raimondo M, Woodward TA, et al. (2016) Association between advances in high-resolution cross-section imaging technologies and increase in prevalence of pancreatic cysts from 2005 to 2014. Clin Gastroenterol Hepatol 14: 585-593.
- Sonavane AD, Amarapurkar DN, Amarapurkar AD (2016) Polycystic pancreas. ACG Case Rep 3: 199-201.
- Malka D, Hammel P, Vilgrain V, Flejou JF, Belghiti J, et al. (1998) Chronic obstructive pancreatitis due to a pancreatic cyst in a patient with autosomal dominant kidney disease. Gut 42: 131-134.
- Kim JA, Blumenfeld JD, Chhabra S, Dutruel SP, Thimmappa ND, et al. (2016) Pancreatic cysts in autosomal dominant polycystic kidney disease: Prevalence and association with PKD2 gene mutations. Radiology 280: 762-770.
- Davenport MS, Caoili EM, Cohan RH, Hoff CN, Ellis JH (2010) Pancreatic manifestations of von Hippel Lindau disease effects of imaging on clinical management. J Comput Assist Tomogr 34: 517-522.
- Ravine D, Gibson RN, Walker RG, Sheffield LJ, Kincald-Smith P, et al. (1994) Evaluation of ultrasonographic diagnostic criteria for autosomal dominant polycystic kidney disease 1. Lancet 343: 824-827.
- Kikuchi O, Kobayashi M, Amano K, Sasaki T, Kitazumi T, et al. (2012) FoxO1 gain of function in the pancreas causes glucose intolerance, polycystic pancreas, and islet hypervascularization. PLoS One 7: e32249.
- Pierreux CE, Poll AV, Kemp CR, Clotman F, Maestro MA, et al. (2006) The transcription factor hepatocyte nuclear factor-6 controls the development of pancreatic ducts in the mouse. Gastroenterol 130: 532-41.
- Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, et al. (2003) Von Hippel-Lindau disease. Lancet 361: 2059-2067.
Citation: Gupta R, Singh AK, Verma P, Mistry K, Pokharia P (2018) Polycystic Disease of the Pancreas: A Case Report . J Gastrointest Dig Syst 8: 552. DOI: 10.4172/2161-069X.1000552
Copyright: © 2018 Gupta R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 8976
- [From(publication date): 0-2018 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 7886
- PDF downloads: 1090