Prevalence of Pathologic Findings in Maxillary Sinuses in Asymptomatic Patients using Cone Beam Computed Tomography
Received: 05-Oct-2018 / Accepted Date: 17-Oct-2018 / Published Date: 25-Oct-2018 DOI: 10.4172/2161-0681.1000353
Keywords: Pathologic findings; Maxillary sinuses; Prevalencem; Asymptomatic; Anatomic variations; Complications; Cross sectional imaging; Cone beam computed tomography
Introduction
The paranasal sinuses are 4 paired sets of air filled cavities of craniofacial complex composed of maxillary, frontal, sphenoidal and ethmoidal air cells [1]. Amongst these, maxillary sinuses, also, called maxillary antra or, Antra of Highmore, are of clinical significance to the dental professionals because of their close proximity to the teeth and associated structures. In recent literature, increased risk of sinusitis has been reported due to trauma to the teeth, recent and complicated exodontias, teeth with pulpal and periodontal pathoses, periapical abscesses and invasive implant therapy, especially, when the schneiderian membrane is perforated. Consequently, diseases of the maxillary sinuses may mimic odontogenic disease and conversely, odontogenic disease may spread to the sinuses or, mimic sinus diseases. In this context, the close approximation of tooth roots in maxillary posterior segments is referred to as drapping [2]. Complications of maxillary sinuses are related to their anatomic and pathologic variations [3]. Pathologies of maxillary sinuses include the so called intrinsic (originating primarily from within the sinus walls) and extrinsic (those that originate outside the sinuses or, those which either impinge on or, infiltrate the sinuses) diseases such as mucosal thickening (MT), polypoidal mucosal thickening (PMT), partial opacification with liquid accumulation (PO), complete opacification (CO) and numerous other findings in the form of retention cysts, root stumps, impacted teeth, antroliths, exostosis, oro-antral fistulas and a plethora of benign and malignant diseases and further abnormalities [4]. It, thus, becomes important to study these sinuses even in situations when the patients reporting for dental complaints are asymptomatic for the sinuses. In the present scenario, cone beam computed tomography (CBCT) has emerged as the standard imaging modality for bone and soft tissue abnormalities offering multiple views with thin sectioning allowing the clinicians to assess the relationship of dental pathologies to the sinus abnormalities in patients who are asymptomatic for the sinuses viewing the vicinity of teeth with the sinus floor and any resultant changes in the soft tissue of the sinus. CBCT is, now-a-days, the imaging modality of choice for dental and maxillofacial imaging for the diagnosis and treatment planning in relation to sinus wall pathologies, sinus lift procedures, surgical removal of impacted teeth, visualizing mandibular canal and adjacent third molar, airway structures, TMJ anatomy, facial asymmetry, placement of dental implants, orthodontic procedures and orthognathic surgeries [5,6]. Pre-operative imaging of sinuses is highly important for the detection of maxillary sinus variations and pathology. With the advent of this convenient 3D imaging, the treatment plan can be modified and the outcome of the pre-prosthetic and orthognathic surgeries, especially, in relation to the posterior maxilla can become more predictable and with successful clinical outcomes, the major advantages of this imaging modality being lower cost, smaller device size and significantly less radiation exposures than the traditional CT. CBCT is, thus, an integrated diagnostic and treatment planning modality to have an accurate assessment of the possible risks and prognosis of the treatment provided [7]. The aim of the present study was to detect the prevalence of pathologic findings in maxillary sinuses in patients who were asymptomatic for the sinuses using cone beam computed tomography (CBCT).
Materials and Methods
The present study was a prospective study wherein CBCT scans of 150 patients between the ages of 18 and 70 years reporting for routine dental complaints were analysed for detecting pathologic findings in the maxillary sinuses. All the patients who fulfilled the inclusion criteria and agreed to participate voluntarily with a written informed consent were considered for the study. Images of patients with recent history of trauma, images with low resolution and those in which presence of metallic artifacts impaired sinus visualization were excluded. The research protocol was approved by the institutional ethics committee governing the use of human subjects in clinical research. A detailed case history was taken including chief complaint, history of presenting illness and medical and personal histories. A thorough clinical examination, including systemic and regional examination, was done. All the patients were, then, subjected to imaging with the help of i-CAT machine with Vision software (Imaging Sciences International).
Identification of intrinsic diseases of maxillary sinuses
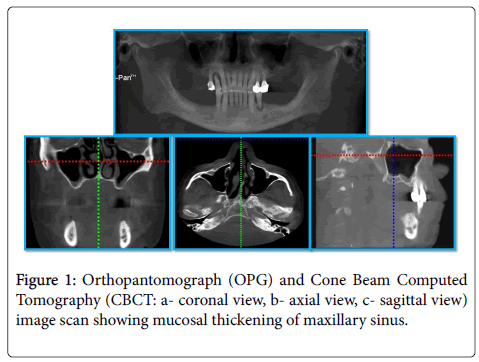
Criteria for identification of Mucosal Thickening (MT): MT was detected as non-corticated radiolucent bands, distinctly, more radiopaque than the air filled sinuses paralleling the bony walls of the sinuses with sinus walls intact. Mucosal thickening of >3 mm seen on any wall of the sinuses in all coronal, sagittal and axial views was considered pathologic. The thickness of the mucosa was determined at the maximum thickness from the sinus wall using the measurement tool provided in the i-CAT Vision software. All measurements were made perpendicularly to the underlying bone starting at the underlying bony plate and ending at the mucosal surface and the thickest area was recorded (Figure 1).
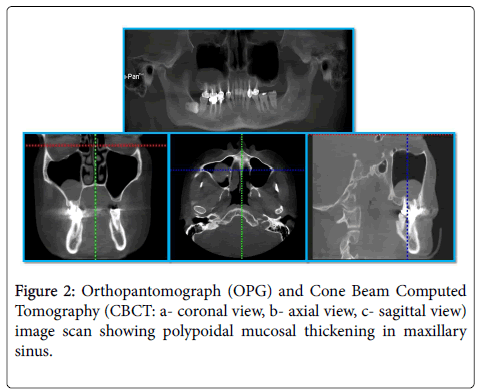
Criteria for identification of Polypoidal Mucosal Thickening (PMT): Presence of any dome shaped radiopacity with intact walls in all coronal, sagittal and axial views was considered as polypoidal mucosal thickening. Polyps and retention cysts seen as smooth, outwardly convex soft tissue masses at imaging were, also, included in polypoidal mucosal thickening (Figure 2).
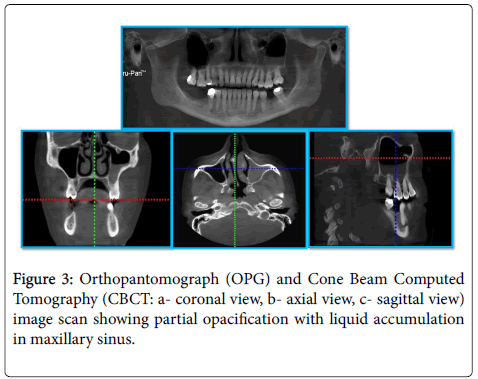
Criteria for identification of Partial Opacification with Liquid Accumulation (PO): Partial opacification resulting from accumulation of secretions appeared radiodense and occupied the inferior aspect of the sinuses. An air-fluid level was seen when scan was evaluated in all coronal, sagittal and axial views. The border between the radiodense fluid and the relatively radiolucent air filled sinuses appeared horizontal and straight with a meniscus. The remaining walls of the sinuses appeared intact (Figure 3).
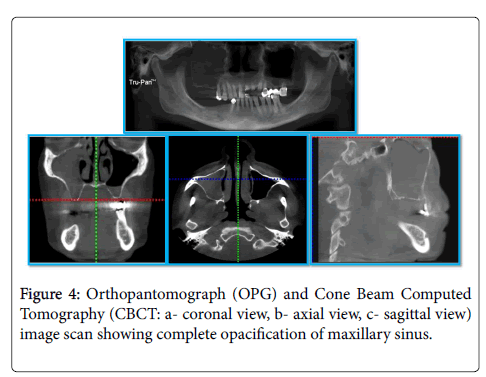
Criteria for identification of Complete Opacification (CO): Complete opacification of the sinuses appeared as totally radiodense sinuses as seen in all coronal, axial and sagittal views with the walls of maxillary sinuses intact (Figure 4).
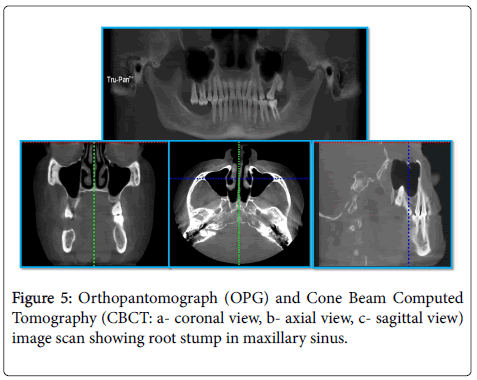
Other findings: These findings included impacted teeth, root stumps (Figure 5), antroliths and exostosis.
Impacted teeth were diagnosed as unusual shapes or, sizes of teeth with difference in radiographic density of enamel, dentin and pulp located within the sinus walls. Root stumps were diagnosed by the characteristic root morphology and anatomy showing root canals. Distinction between a foreign body and antroliths was made based on the extent of the density and opacity seen on the images while exostosis was diagnosed based on the presence of high-density structures or, radio-opacities on the images.
Identification of extrinsic diseases of maxillary sinuses
Extrinsic disease of the sinuses was identified as any lesion appearing to be having their origin other than the sinuses in the form of a break in the continuity of the corticated walls of the sinuses and/or, sinus floor or, the extraneous pathologies encroaching the air space of sinuses.
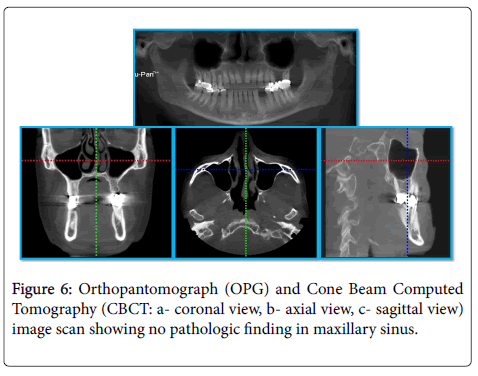
No pathologic findings: Maxillary sinuses showing no pathologic findings (intrinsic or, extrinsic diseases or, any other findings) were included in this group of observation (Figure 6).
Statistical analysis
The data was analyzed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA). The statistical software used for the analysis of the data included SAS 9.2, SPSS version 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment version 2.11.1 while Microsoft word and Excel were used to generate graphs, tables etc. Distribution of the overall prevalence of pathologic findings according to age and sex were calculated using Chi-Square test while p-value <0.05 was considered to be statistically significant.
Results
The present study included a total of 150 patients divided into 5 age groups wherein the minimum numbers of patients were in the age group of 19-29 years while maximum numbers of patients were in the age group of 60-69 years (Table 1).
| Age group (in years) | No. of subjects | % of subjects |
|---|---|---|
| 19 – 29 | 10 | 6.7 |
| 30 – 39 | 12 | 8.0 |
| 40 – 49 | 29 | 19.3 |
| 50 – 59 | 37 | 24.7 |
| 60 – 69 | 62 | 41.3 |
Table 1: Age distribution of the subjects studied.
The sex distribution of the study sample is shown in Table 2 wherein the prevalence of sinus pathologies was found to be more common in the female patients though the overall prevalence did not differ significantly between the male and female patients (p-value=0.098).
| Sex | No. of subjects | % of subjects |
|---|---|---|
| Male | 67 | 44.7 |
| Female | 83 | 55.3 |
| Total | 150 | 100.0 |
Table 2: Sex distribution in the obtained data.
Out of a total of 150 patients, 73 patients were advised CBCT for the planning of implant therapy (48.7%), 51 patients underwent CBCT analysis for prosthetic rehabilitations (34.0%), 16 patients underwent pre-surgical analysis (10.7%), 5 patients had orthodontic reasons (3.3%) while 4 patients had miscellaneous reasons for resorting to the CBCT analysis (Table 3).
| Reasons for CBCT | No. of subjects | % of subjects |
|---|---|---|
| Implant | 73 | 48.7 |
| Surgery | 16 | 10.7 |
| Orthodontic | 5 | 3.3 |
| Prosthetic | 51 | 34.0 |
| Miscellaneous | 5 | 3.3 |
Table 3: Distribution of reasons for CBCT.
Pathologies of maxillary sinuses include intrinsic and extrinsic diseases such as mucosal thickening (MT), polypoidal mucosal thickening (PMT), partial opacification with liquid accumulation (PO), complete opacification (CO) and a plethora of other findings including retention cysts, impacted teeth, root stumps, antroliths, exostosis, oro-antral fistulas and various benign and malignant diseases and further abnormalities. Furthermore, as per the aim of the present study, right and left maxillary sinuses were evaluated differently for detection of pathologic findings. Overall prevalence of pathologic findings was found to be 58% with the prevalence of mucosal thickening being 29.3%, polypoidal mucosal thickening, 36.7%, partial opacification with liquid accumulation, 2%, complete opacification, 0.7% and miscellaneous findings as 0.7%. 16% of the patients revealed mucosal thickening in relation to the right sinuses as against 20.7% in the left sinuses. Similarly, 24% of the patients revealed polypoidal mucosal thickening in relation to the right sinuses as against 20.7% seen in the left sinuses. Likewise, partial opacification with liquid accumulation was seen 1.3% of the left sinuses as against 0.7% of the right sinuses. Complete opacification as well as miscellaneous findings were, though, seen only in 0.7% of the right sinuses with zero prevalence in relation to the left sinuses (Table 4).
| Presence/Absence of Pathologic Findings |
Right Maxillary Sinus | Left Maxillary Sinus | Overall Findings | |||
|---|---|---|---|---|---|---|
| No. of subjects | % of subjects | No. of subjects | % of subjects | No. of subjects | % of subjects | |
| No pathologic findings | 89 | 59.3 | 89 | 59.3 | 63 | 42.0 |
| Mucosal thickening | 24 | 16.0 | 31 | 20.7 | 44 | 29.3 |
| Polypoidal mucosal thickening | 36 | 24.0 | 31 | 20.7 | 55 | 36.7 |
| Partial opacification with liquid accumulation | 1 | 0.7 | 2 | 1.3 | 3 | 2.0 |
| Complete opacification | 1 | 0.7 | 0 | 0.0 | 1 | 0.7 |
| Miscellaneous findings | 1 | 0.7 | 0 | 0.0 | 1 | 0.7 |
Table 4: Distribution of pathologic findings in maxillary sinus.
Considering the right and left maxillary sinuses, out of the total 150 patients, 58% of the patients showed the overall presence of pathologic findings as against 42% wherein no pathologic findings were seen (Table 5).
| Right Maxillary Sinus | Left Maxillary Sinus | Overall Findings | ||||
|---|---|---|---|---|---|---|
| Presence/Absence of Pathologic Findings |
No. of subjects | % of subjects | No. of subjects | % of subjects | No. of subjects | % of subjects |
| Overall Pathologic Findings |
61 | 40.7 | 61 | 40.7 | 87 | 58.0 |
| No Pathologic Findings |
89 | 59.3 | 89 | 59.3 | 63 | 42.0 |
Table 5: Distribution of overall prevalence of pathologic findings in maxillary sinus (Chi-square value=0.00, p-value=0.999. Comments: The overall prevalence of pathological findings did not differ significantly between right and left side of Maxillary Sinus, p-value >0.05).
Also, there was a significant difference in the observation of overall pathologic findings in relation to the sex wherein 65.7% of the male patients revealed the presence of overall pathologic findings as against the female patients wherein the prevalence was found to be 51.8%. On the contrary, 48.2% of the female patients were pathology free as against 34.3% of the male patients wherein no pathologic findings were seen (Table 6).
| Male | Female | |||
|---|---|---|---|---|
| Presence/Absence of Pathologic Findings |
No. of subjects | % of subjects | No. of subjects | % of subjects |
| Overall Pathologic Findings |
44 | 65.7 | 43 | 51.8 |
| No Pathologic Findings |
23 | 34.3 | 40 | 48.2 |
Table 6: Distribution of overall prevalence of pathologic findings according to sex (Chi-square value=2.925, p-value=0.098. Comments: The overall prevalence of pathological findings did not differ significantly between male and female subjects studied, p-value >0.05).
The present study included 150 patients divided into 5 age groups wherein the minimum number of patients who revealed pathologies in relation to maxillary sinuses were found to be in the age group of 19-29 years (30%) while the highest prevalence of sinus pathologies was seen in the age group of 30-39 years (50%). 48.6% of the patients in the age group of 50-59 years were the next in order followed by the patients in the age group of 40-49 years who revealed pathologies in 48.3% of the patients (Table 7).
| Age group (in years) | No. of subjects with Pathologic findings | % of subjects with Pathologic findings | No. of subjects with No pathologic findings | % of subjects with No pathologic findings |
|---|---|---|---|---|
| 19 – 29 | 7 | 70.0 | 3 | 30.0 |
| 30 – 39 | 6 | 50.0 | 6 | 50.0 |
| 40 – 49 | 15 | 51.7 | 14 | 48.3 |
| 50 – 59 | 19 | 51.4 | 18 | 48.6 |
| 60 – 69 | 40 | 64.5 | 22 | 35.5 |
| Total | 87 | 100.0 | 63 | 100.0 |
Table 7: Distribution of overall prevalence of pathologic findings according to age groups (Chi-square value=3.127 p-value=0.537. Comments: The overall prevalence of pathological findings did not differ significantly across different age groups of the subjects studied, p-value >0.05).
Discussion
The aim of the present study was to detect the prevalence of pathologic findings in maxillary sinuses in patients who were asymptomatic for the sinuses using cone beam computed tomography (CBCT) wherein CBCT scans of 150 patients between the ages of 18 and 70 years reporting for routine dental complaints were analyzed for detecting pathologic findings in the maxillary sinuses. In the present study, out of 150 patients, 44.7% were male patients and 55.3% were female patients. There was no statistically significant difference obtained in the present study in terms of age and sex similar to the findings of the studies conducted by Raghav et al. [8] and Dobele et al. [9]. Ritter et al. [10] and Vallo et al. [11], though, found higher prevalence of pathologic findings in the male patients than as compared to the female patients. Ritter et al. [10], also, found higher prevalence of pathologic findings in patients above 60 years of age in contrast with the present study wherein the highest prevalence of sinus pathologies was seen in the age group of 30-39 years (50%). As per the findings of the present study, out of a total of 150 patients, 73 patients were advised CBCT for the planning of implant therapy (48.7%), 51 patients underwent CBCT analysis for prosthetic rehabilitations (34.0%), 16 patients underwent pre-surgical analysis (10.7%), 5 patients had orthodontic reasons (3.3%) while 4 patients had miscellaneous reasons for resorting to the CBCT analysis. Considering the reasons for CBCT indication, maximum number of patients were advised CBCT for the planning of implant therapy (48.7%) similar to the findings of the studies conducted by Raghav et al. [8] and Kihara et al. [12] wherein implant therapy was the major reason for advising CBCT in the patients. Ritter et al. [10], however, found trauma and implant treatment together as the major reasons for the indication of CBCT scans. Alamri et al. [13], on the contrary to these studies, found pre-surgical analysis as the major reason for advising CBCT scans followed by implant treatment and forensic dentistry purpose which was the least advised reason for CBCT analysis. The overall prevalence of incidental pathologic findings in the present study was 58% which was in concordance with the study conducted by Kihara et al. [12] which showed a similar prevalence of 58% in their study. The overall prevalence of incidental pathologic findings in the present study was, also, found to be in accordance with the studies conducted by Raghav et al. [8] showing 59.7% prevalence and Ritter et al. [10] showing 56.3% prevalence. In other studies conducted by Vallo et al. [11], an overall prevalence of 19%, Cha et al. [14], 24.6% and Lim and Spangera [15], 27.5% of prevalence has been reported. The results of these studies have shown comparatively lower prevalence of incidental pathologic findings than was seen in the present study. The variations in the results of the present study comparing the above mentioned studies could be attributed to the different populations addressed in the present study with different imaging modality, variation in the sample size, sample distribution and definition of the abnormality being the other significant reasons to be considered. Rege et al. [16] reported an overall prevalence of 68.2% of such incidental findings which was quite higher than the present study and other similar studies aforementioned which might be attributed to the fact that they had investigated a greater number of possible causes of alterations in the maxillary sinuses including the congenital and acquired lesions, bone related abnormalities and traumatic and iatrogenic lesions which were included in the exclusion criteria in the present study. The present study revealed polypoidal mucosal thickening (PMT) as a major finding with a prevalence of around 36.7% similar to the study conducted by Shiki et al. [17] who reported an overall prevalence of 25% while contradictory results with lower prevalence were found in the study conducted by Raghav et al. [8] who reported an overall prevalence of 7.2% for polypoidal mucosal thickening. An overall prevalence of polypoidal mucosal thickening was found to be 15% in the study conducted by Kihara et al. [12], 8% in the study conducted by Lim and Spangera [15] and 10.1% in the study conducted by Rege et al. [16]. This variation in results might be due to different definitions of polypoidal mucosal thickening, different locations considered and different measurement criteria used in the different studies. In the present study, mucosal thickening was found to be the second most common incidental pathologic finding which showed a prevalence of about 29.3% in accordance with the studies conducted by Raghav et al. [8] who found 35.1% and Carmeli et al. [18] who found 36.1% prevalence. The prevalence of mucosal thickening, though, was a little higher in the studies conducted by Dobele et al. [9] who found 48.5%, Kihara et al. [12] who found 43% and Shiki et al. [17] who reported 49% of mucosal thickening, though, in all the studies reported, mucosal thickening was the second most common incidental pathologic finding in the maxillary sinuses. Contrary to the findings of the aforementioned studies, Vallo et al. [11] found 12% and Lim and Spangera [15] found 16.8% prevalence of mucosal thickening in their studies. Highest prevalence of mucosal thickening was found in the study conducted by Rege et al. [16] who reported 66% prevalence of mucosal thickening in their study. The huge variation in the overall prevalence of mucosal thickening in the present study and other studies and in between the said studies might be due to the differences in the pathological criteria which was used to measure the mucosal thickening. In the present study, prevalence of partial opacification with liquid accumulation was found to be 2% which was in accordance with the study conducted by Lim and Spangera [15] who found a prevalence of 2.3% while contradictory to the results of the study conducted by Shiki et al. [17] who reported 0% prevalence of partial opacification in their study. The said variations might be due to the difference in season or, climate during the period the studies were conducted. Complete opacification was the least found incidental finding in the present study in concordance with the studies conducted by Dobele et al. [9] who found 2.9% of total opacity, Kihara et al. [12] who found 2% antral opacification and Lim and Spangera [15] who found 2.7% of complete opacification in their study. Rege et al. [16], though, found 7.8% of complete opacification in their study in concordance with the studies conducted by Raghav et al. [8] who found 16.6% prevalence and Shiki et al. [17] who reported 18% prevalence of complete opacification in their studies. The said variations in these studies might be due to the differences in the geographic area of population studied, the sample size of the study and the criteria used to consider pathologic findings in the maxillary sinuses. Similarly, the overall prevalence of miscellaneous findings, also, presented huge variations with an overall prevalence of 0.7% in the present study similar to the studies conducted by Raghav et al. [8] which showed 0.7% prevalence, Kihara et al. [12] who found 2% prevalence of foreign bodies and 13% prevalence of root protrusion into the sinuses and Shiki et al. [17] who reported 5% prevalence of antroliths in their studies. 42% of the sinuses did not reveal any pathologic finding in the present study in close approximation to the studies conducted by Raghav et al. [8] wherein 40.2% and Ritter et al. [10] wherein 43.7% of the sinuses did not reveal any pathologic finding. In the present study, prevalence of extrinsic diseases appeared to be 0% as none of patients’ scans fulfilled the criteria in the present study for extrinsic disease identification. Also, Vallo et al. [11] showed a significant association between pathologic dental findings and mucosal thickening in the maxillary sinuses while Maloney and Doku [19] indicated that 10% to 12% of the sinusitis cases had an odontogenic origin, however, direct comparison of other studies with the current study was inappropriate because of the different age distribution and geographic origin of the sample and different imaging modalities and different age and patient groups because of which the existing data varied among the said studies and the present study. Furthermore, the definitions of pathological changes varied among the said studies and the present study and in some cases, were not adequately described for a clear distinction. To conclude, higher prevalence of pathologies in asymptomatic maxillary sinuses found in the present study emphasized the significance of a thorough examination of the routine dental patients by the dento-maxillofacial radiologists with necessary investigations in the form of higher imaging modalities like CBCT and a thorough interpretation of the whole volume scans including a proper differentiation of pathologic lesions from anatomic variations as it might have an impact on patient’s medical status and/or, prove of clinical relevance in planning treatment in such patients. The present study, also, highlighted the clinical implications, dental pathologies might have, in relation to the maxillary sinuses underlying the significance of their accurate assessment in the perspective of dental and maxillofacial and ENT problems with a multi-disciplinary approach of treatment for the successful treatment of chronic sinus pathoses.
References
- Van Cauwenberge P, Sys L, De Belder T, Watelet JB (2004) Anatomy and physiology of the nose and the paranasal sinuses. Immunol Allergy Clin North Am 24: 1-17.
- Kretzschmar DP, Kretzschmar JL (2003) Rhino-sinusitis: Review from a dental perspective. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96: 128-135.
- Zijderveld SA, van den Bergh JP, Schulten EA, ten Bruggenkate CM (2008) Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J Oral Maxillofac Surg 66: 1426-1438.
- White SC, Pharoah MJ (2004) Oral Radiology, Principles and Interpretation. (5thedn), Mosby, St Louis, USA, pp.586-594.
- Mehra P, Murad H (2004) Maxillary sinus disease of odontogenic origin. Otolaryngol Clin North Am 37: 347-364.
- Tetradis S, Anstey P, Graff-Radford S (2010) Cone beam computed tomography in the diagnosis of dental disease. J Calif Dent Assoc 381: 27-32.
- De Vos W, Casselman J, Swennen GRJ (2009) Cone-beam computerized tomography (CBCT) Imaging of the Oral and Maxillofacial Region: A Systematic Review of the Literature. Int J Oral Maxillofac Surg 38: 609-625.
- Raghav M, Karjodkar FR, Sontakke S, Sansare K (2014) Prevalence of incidental maxillary sinus pathologies in dental patients on cone beam computed tomographic images. Contemp Clin Dent 5: 361-365.
- Ilze Dobele, Ligija Kise, Peteris Apse, Gints Kragis, Andris Bigestans (2013) Radiographic assessment of findings in the maxillary sinus using cone beam computed tomography. Stomatologija (Baltic Dent Maxillofac J) 15: 119-122.
- Ritter L, Lutz J, Neugebauer J, Scheer M, Dreiseidler T, et al. (2011) Prevalence of pathologic findings in the maxillary sinus in cone beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111: 634-40.
- Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A (2010) Prevalence of mucosal abnormalities of maxillary sinus and their relationship to dental disease in panoramic radiography: Results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109: e80-87.
- Kihara E, Chindia M, Ocholla T, Parker M (2014) Clinical Significance of Pathological and Anatomical Findings in Cone Beam CT Scans of the Maxillary Sinus. J Stomatol 4: 285-290.
- Alamri HM, Sadrameli M, Alshalhoob MA, Sadrameli M, Alshehri MA (2012) Applications of CBCT in dental practice: A review of the literature. Gen Dent 60: 390-400.
- Cha JY, Mah J, Sinclair P (2007) Incidental findings in the maxillofacial area with 3-dimensional cone beam imaging. Am J Orthod Dentofacial Orthop 132: 7-14.
- GT Lim C, Spangera M (2012) Incidental maxillary sinus findings in patients referred for head and neck CT angiography Incidental maxillary sinus findings in patients referred for head and neck CT angiography. Singapore Dent J 33: 1-4.
- Rege IC, Sousa TO, Leles CR, Mendonça EF (2012) Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health 12:30.
- Shiki K, Tanaka T, Kito S, Wakasugi-Sato N, Matsumoto-Takeda S, et al. (2014) The significance of cone beam computed tomography for the visualization of anatomical variations and lesions in the maxillary sinus for patients hoping to have dental implant-supported maxillary restorations in a private dental office in Japan. Head Face Med 10: 20.
- Carmeli G, Artzi Z, Kozlovsky A, Segev Y, Landsberg R (2011) Antral computerized tomography pre-operative evaluation: Relationship between mucosal thickening and maxillary sinus function. Clin Oral Implants Res 22: 78-82.
- Maloney PL, Doku HC (1968) Maxillary sinusitis of odontogenic origin. J Can Dent Assoc 4: 591-603.
Citation: Nayyar A (2018) Prevalence of Pathologic Findings in Maxillary Sinuses in Asymptomatic Patients using Cone Beam Computed Tomography. J Clin Exp Pathol 8: 353. DOI: 10.4172/2161-0681.1000353
Copyright: © 2018 Nayyar A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5677
- [From(publication date): 0-2018 - Dec 22, 2025]
- Breakdown by view type
- HTML page views: 4634
- PDF downloads: 1043