Pyopneumothorax Caused by Streptococcus Constellatus: A Case Report and Literature Review
Received: 06-Sep-2022 / Manuscript No. jcidp-22-75673 / Editor assigned: 08-Sep-2022 / PreQC No. jcidp-22-75673 (PQ) / Reviewed: 21-Sep-2022 / QC No. jcidp-22-75673 / Revised: 26-Sep-2022 / Manuscript No. jcidp-22-75673 (R) / Published Date: 30-Sep-2022
Abstract
Background: Streptococcus constellatus is a member of Streptococcus anginosus group (SAG) that tends to cause pyogenic infections in various cavities. However, Streptococcus constellatus is not easily detected as a pathogen in the routine laboratory tests. As a member of SAG, it is the rarest to cause severe infections, which lead to ICU hospitalization. This case report adds valuable information to the current body of knowledge of these infective diseases.
Case presentation: A 61-year-old woman was admitted to the hospital due to fever, chest pain and shortness of breath for 1 week. Chest x ray showed right-sided pleural effusion and an irregularly shaped cavity with an air-fluid level, so the patient underwent open thoracotomy and decortication surgery for open drainage. 2 chest tubes were inserted, and purulent fluid was aspirated. Postoperatively, the patient remained intubated due to septic profile and was admitted to the ICU. Intravenous broad-spectrum antibiotics were used. The routine etiological examinations of the pleural effusion were all positive and detected Streptococcus constellatus. On the 3rd day of ICU stay, the patient deteriorated, and the surgical site showed signs of infection. A subsequent chest CT showed patchy opacities with air bronchogram, a new cavity on the outside of the postoperative lesions (possible relapse of previously treated abscess) and subcutaneous emphysema. Deep vein thrombosis in the left internal jugular vein was also confirmed in the chest CT. The patient underwent a 2nd surgery and PDR A.baumanii was detected and treated with targeted intravenous antibiotics. The patient recovered and was dismissed from hospital after 41 days of hospitalization.
Conclusions: We reported a case of pyopneumothorax secondary to Streptococcus constellatus infection, which was identified by bacterial culture. This case highlights the SAG group members’ potential of causing rare severe infections in the respiratory system and how important is early surgical approach in combination with intravenous antimicrobial treatment on the clinical outcome.
Keywords
Streptococcus constellatus; Streptococcus anginosus group; Pyopneumothorax; Lung abscess
Background
Pyopneumothorax (also known as infected hydropneumothorax or empyemic hydropneumothorax) is a pleural collection of pus and gas. It may be thought of a variant of a thoracic abscess with gas-containing components although the etiology may be different. As a clinical manifestation, it is a rare complication of pyogenic infections.
Streptococcus constellatus (S.constellatus) is a member of one of the Streptococcus anginosus group (SAG), a subgroup of viridans streptococci, widely distributed in the oral cavity, nasopharynx, gastrointestinal tract, and vagina in 15–30% of healthy people [1]. The members of SAG group are considered responsible for various pyogenic infections, mainly reported at the oral, thoracic, and abdominal cavity. Of all pyogenic infections caused by SAG pathogens, empyema and lung abscess represent only 20% [2]. Predispositional factors for severe infection are COPD, HIV infection, diabetes mellitus, alcohol abuse and periodontal diseases.
As a member of SAG, S.constellatus induces abscesses mainly in respiratory tract, brain, liver, bone and soft tissues. Symptoms of pulmonary infection include shortness of breath, chest pain, cough, and fever. Laboratory tests often suggest neutrophilic leukocytosis, abnormal liver function, and elevated CRP. The median stay in hospital is 34 days [3, 4].
This case report adds valuable information to the current body of knowledge of the SAG group potential of causing severe pyogenic infections in the respiratory system.
Case Presentation
In the era of SarS-Cov2 pandemic, a 61-year-old woman presented at a primary care unit, in the begging of April 2021, with high grade fever, shortness of breath and progressively worsening right sided chest pain for a week. Rapid antigen test for Covid was negative. The patient was referred to a tertiary hospital for further examination.
The patient’s medical record included hypertension, dyslipidemia, and obesity. The patient was an active smoker. No relevant travel history or contact history were detected. 2 weeks ago, the patient visited the dentist and had a tooth extraction. No food or drug allergies were mentioned.
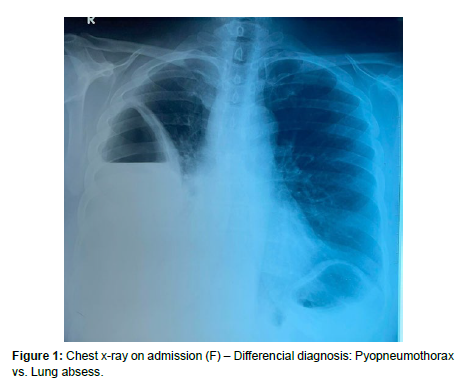
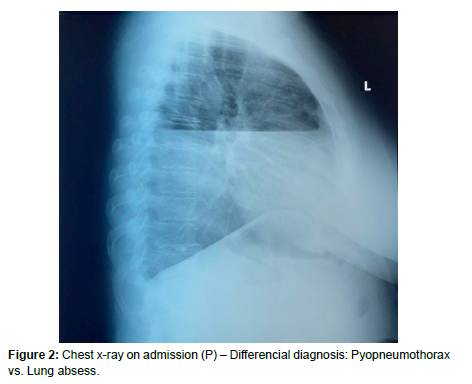
On admission, the patient was febrile (38.7 oC), hemodynamically stable (NBP 150/110), although tachycardic (HR 100 bpm), and hypoxic (Spo2 88%). From auscultation of respiratory system, breath sounds were absent of right chest wall. Other physical examination results were reported as normal. Initial blood test showed elevated white blood cell (WBC) counts (18.6× 109 /L) with neutrophilic type (91.5%) and C-reactive protein (CRP) was elevated. Other laboratory test results were normal. Chest x ray showed right-sided pleural effusion and an irregularly shaped cavity with an air-fluid level, raising suspicion for pyopneumothorax or lung abscess [Figures 1, 2]. Intravenous Ciprofloxacin 400mg every 12 hours was used as broadspectrum antimicrobial therapy.
The patient underwent open thoracotomy for drainage and 2 chest tubes were inserted for purulent fluid was aspirated. Right lung decortication was performed. Postoperatively, the patient remained intubated due to septic profile and was admitted to the ICU.
Gram stain of the fluid showed signs of polymicrobial infection, but the routine etiological examination of the effusion isolated only S.constellatus, susceptible to the intravenous antibiotics that the patient was receiving [Table 1].
| 1strcsc | ||
| MIC | Cat. | |
| Ampicillin | <=0.25 | S |
| Benzyl penicillin | <=0.12 | S |
| Cefotaxime | 0.5 | S |
| Ceftriaxone | 1 | S |
| Chloramphenicol | 2 | S |
| Clindamycin | <=0.25 | S |
| Erythromycin | <=0.12 | S |
| Levofloxacin | 0.5 | S |
| Linezolid | <=2 | S |
| Moxifloxacin | 0.12 | S |
| Tetracycline | 0.5 | S |
| Tigecycline | <=0.06 | S |
| Vancomycin | 0.5 | S |
| Isolate Number 1: Streptococcus constellatus ssp constellatus <strcsc> | ||
However, the patient’s status was not improving. On the 3rd day of ICU stay, on mechanical ventilation support, the patient had impaired oxygenation (AVC mode FiO2 100% PaO2/FiO2 = 125). Hemodynamically, intravenous vasopressors were used at a rate of 20μcg/ml/kg. From routine blood count examination, the patient maintained a septic profile, with progressively elevating WBC count (20.9 x 109 – neutrophilic type 93.5%). Examining the surgical site, it showed signs of surgical tissue infection and from the basal chest tube, outflow of purulent fluid were detected. New blood, bronchial and cultures from aspirated fluid and surgical site were received. Also, pathological levels of D-dimers were detected and from the examination of lower limbs with ultrasound Doppler, deep vein thrombosis (DVT) of posterior tibial vein was confirmed. The patient was then started on therapeutic dose of low molecular weight heparin (LMWH).
Intravenous antibiotics were upgraded due to the severity of the case (Meropenem – Clindamycin – Linezolid – Colistin) and the patient received for 3 days pleura irrigation with NaCl 0.9% as suggested by the thoracic surgeons.
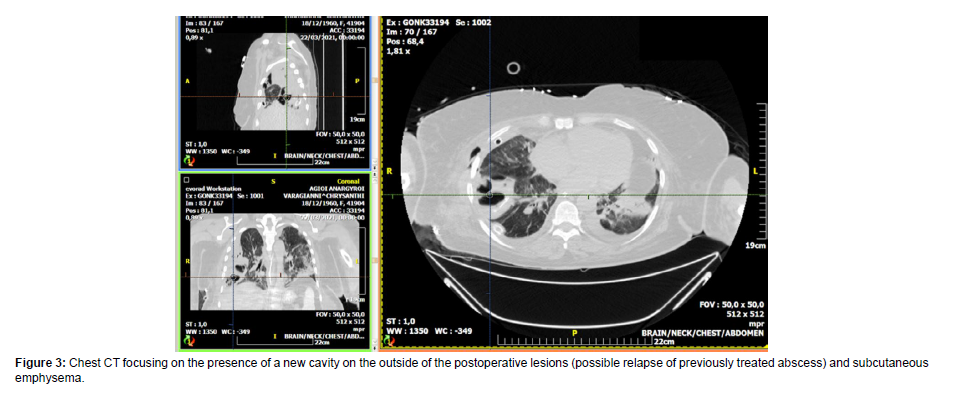
A subsequent chest CT was performed that showed patchy opacities with air bronchogram, a new cavity on the outside of the postoperative lesions (possible relapse of previously treated abscess) and subcutaneous emphysema. Deep vein thrombosis in the left internal jugular vein was also confirmed in the chest CT [Figure 3].
The patient continued to deteriorate clinically and underwent a 2nd surgery. Intraoperatively, the surgical site was cleansed, and fluid cultures were received. The chest tubes were removed and replaced, after the rejuvenation of the wound entrance. Because of the prolonged stay on mechanical ventilation, surgical tracheostomy was also performed.
Blood cultures isolated Acinetobacter baumanii PDR (A.baumanii) and Enterococcus faecalis (E.faecalis) and the antimicrobial combination changed in Meropenem – Tygecycline – Colistin + Vancomycin. A.baumanii was also isolated from fluid and pleura tissue cultures, thus the patient’s deterioration was attributed to a polymicrobial re-infection.
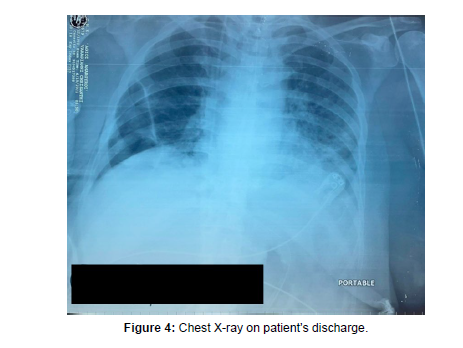
A week later, the patient started improving and the rest postoperative period was uncomplicated. She was hospitalized in ICU for 1 month. The tracheostomy was closed. The patient continued intravenous targeted therapy for 4 weeks. Subsequent follow-up showed improving chest X-ray [figure 4] and general health. The patient recovered and was dismissed from hospital after 41 days overall length of stay.
Discussion and Conclusions
In this case, we reported a case of pyopneumothorax caused by S. constellatus. As a member of SAG, it is widely distributed in the oral cavity and nasopharynx.
Lung abscesses are referred as a complication of aspiration pneumonia, caused mainly by mouth anaerobes such as Peptostreptococcus, Bacteroides, and Fusobacterium species. Aerobic bacteria that infrequently cause lung abscess include Staphylococcus aureus, S. pyogenes, S. pneumoniae, Klebsiella pneumoniae, Haemophilus influenzae, Actinomyces species, Nocardia species, and Gram-negative bacilli [3].
The identification of S. constellatus can be quite difficult with the routine methods, because of the prolonged anaerobic culture environment, although in our patient it was isolated in the etiological exams of the effusion received surgically. The abovementioned explains the reason why SAG is often underestimated as pathogens in the pathophysiology of severe infections of lower respiratory tract [2].
According to the literatures, among a collection of 423 clinical infections related to SAG, 1.4% of the strains were of intermediate susceptibility to penicillin and none exhibited high-level resistance to gentamicin. All the strains were susceptible to cefotaxime, vancomycin and teicoplanin. Clindamycin, doxycycline, amoxicillin, and metronidazole could be used for S. constellatus infection [1].
Although S. constellatus is not a commonly detected pathogen causing pleural effusion, we still need to pay attention to its pathogenicity in clinical practice. Empyema caused by S.constellatus should be treated with a combination of antimicrobial therapy and early surgical eradication of the primary source [4]. In our case, open thoracotomy was preferred due to the severity of the case, pyopneumothorax was drained and lung decortication was performed.
Pathophysiology of the infection of lower respiratory tract involves translocation of the pathogen from the oral cavity to the lungs. Patients who develop lung abscess commonly have periodontal disease. Our patient according to past medical history, several days before, had visited the dentist because of a dental infection that was partially treated with oral antibiotics and after the affected tooth was extracted. According to literatures, patients with concomitant dental infections are more susceptible to polymicrobial infections [3]. There were also cases of septic shock due to S. constellatus bacteremia following tooth extraction.
Severe infections due to S.constellatus are related with prolonged hospitalization [4]. Our patient was admitted to ICU after the 1st surgery. On the 3rd day of ICU stay; her case was complicated by a Gram negative polymicrobial infection (A.baumanii and E.faecalis) which caused the patient’s 2nd deterioration that led her to a concurrent surgery. The patient was hospitalized in the ICU for 30 days and was discharged from hospital after 41 days overall stay.
Collectively, this case reported pyopneumothorax secondary to S. constellatus infection, which was treated with a combination of early surgical approach and intravenous antibiotics. We expect to raise awareness in the role of SAG in the pathogenesis of severe respiratory infections and also add further valuable information to the current body of knowledge of this infective disease.
Learning Points
• Pyopneumothorax in S. constellatus infection is a rare but severe manifestation
• Early eradication of the primary source of infection and surgical approach is crucial in determining the clinical outcome.
• In order to achieve full recovery, the combination of targeted intravenous antibiotic therapy and surgical approach is important.
References
- Kobo O, Nikola S, Geffen Y, Paul M (2017) The pyogenic potential of the different Streptococcus anginosus group bacterial species: retrospective cohort study. Epidemiol Infect 145:3065-3069.
- Noguchi S, Yatera K, Kawanami T, Yamasaki K, Naito K, et al. (2015) The clinical features of respiratory infections caused by the Streptococcus anginosus group. BMC Pulm Med. 26:115:133.
Indexed at, Google Scholar, Crossref - Yamasaki K, Kawanami T, Yatera K, Fukuda K, Noguchi S, et al. (2013) Significance of anaerobes and oral bacteria in community-acquired pneumonia. PLoS One 8: e63103.
- Junckerstorff RK, Robinson JO, Murray RJ (2014) Invasive Streptococcus anginosus group infection-does the species predict the outcome? Int J Infect Dis18: 38-40.
- Okada F, Ono A, Ando Y, Nakayama T, Ishii H, et al. (2013) High-resolution CT findings in Streptococcus milleri pulmonary infection. Clin Radiol. 68: e331-337.
- Gogineni VK, Modrykamien A (2011) Lung abscesses in 2 patients with Lancefield group F streptococci (Streptococcus milleri group). Respir Care 56: 1966-1969.
- Kobashi Y, Mouri K, Yagi S, Obase Y, Oka M (2008) Clinical analysis of cases of empyema due to Streptococcus milleri group. Jpn J Infect Dis61:484-486.
- Shinzato T, Saito A (1994) A mechanism of pathogenicity of "Streptococcus milleri group" in pulmonary infection: synergy with an anaerobe. J Med Microbiol 40:118-123.
- Zhang Z, Xiao B, Liang Z (2020) Successful treatment of pyopneumothorax secondary to Streptococcus constellatus infection with linezolid: a case report and review of the literature. J Med Case Rep. 14:180.
- Che Rahim MJ, Mohammad N, Wan Ghazali WS (2016) Pyopneumothorax secondary to Streptococcus milleri infection. BMJ Case Rep bcr 2016217537.
- Xia J, Xia L, Zhou H, Lin X, Xu F (2021) Empyema caused by Streptococcus constellatus: a case report and literature review. BMC Infect Dis 21:1267.
- Lee YJ, Lee J, Kwon BS, Kim Y (2021) An empyema caused by Streptococcus constellatus in an older immunocompetent patient: Case report. Medicine (Baltimore) 100: e27893.
- George B, Tanveer N, Boyars M (2021) Streptococcus Constellatus Empyema Presenting With Undulant Fever Pattern- A Case Report and Literature Review. Int J Respir Pulm Med. 8:160.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Alevrogianni F, Psallida V, Fildisis G (2022) Pyopneumothorax Caused by Streptococcus Constellatus: A Case Report and Literature Review. J Clin Infect Dis Pract, 7: 162.
Copyright: © 2022 Alevrogianni F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 2401
- [From(publication date): 0-2022 - Sep 01, 2025]
- Breakdown by view type
- HTML page views: 1921
- PDF downloads: 480