Rat Killer Poisoning vs Liver Damage: A View in South Indian Patients of Tertiary Care Center
Received: 12-Jun-2018 / Accepted Date: 26-Jun-2018 / Published Date: 30-Jun-2018 DOI: 10.4172/2161-069X.1000569
Abstract
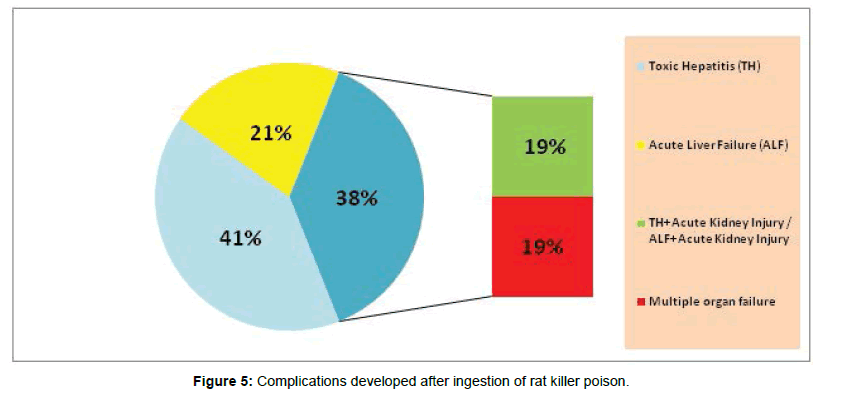
Background: Rodenticide ingestion is common suicidal poisoning. In the absence of antidote, consumption is fatal. We aimed at socio-demographic characteristics, analyzed predictive factors, biological elevation curve and its outcome. Methods: 101 patients admitted with rodenticide poisoning. Socio-demographic characteristics, probable predictive factors, Serial charting biological markers recorded. Standard care management was given. Results: Of the 101 patients 76% were from rural and 24% urban. 62% were female and male 38%. Mean age was 26.0 ± 10.467 years. Unmarried men and married women were higher. Higher number was literate 46% and Illiterate 28%. Higher number was salaried 45% and students 30%. 34% consumed raw, 30% mixed with water. 57% ingested <10 grams, 24% up to 20 and 20%, >20 grams. Mean dosage of 13.42 ± 7.069 grams. Mean care seeking time 6.0 ± 6.3702 hours. 46% sought <3 hours, 41% in 10 and 13% >10 hours. Chief symptom was vomiting in 33% patients, abdominal pain 36%, headache 27% and oral bleeding 4%. Biological markers in survivor and non-survivor showed, T bill, Albumin, AST, ALT, Creatinine, PT, INR and MELD were statistically significant. T protein, platelet and urea were not significant. 9 patients had MELD <10, 30-(11-20), 35-(21-30) and >30 MELD was in 27. All of those had a MELD of >40 died. 41% had toxic hepatitis, 21% acute liver failure, 19% toxic hepatitis with acute kidney injury/ALF with acute kidney injury and 19% developed multiple organ failure. Overall mortality rate was 19%, 81% recovered with 8.88 days mean hospital stay. Conclusions: Patient ingested yellow phosphorus had liver damage. Lethal dosage and late presentation to medical facility led to liver failure, multiple organ failure and mortality in spite of standard care. Creating awareness, promoting mental health, suicide prevention and framing proper guidelines of treatment are best cornerstones to reduce mortality by rat killer poisoning.
Keywords: Rodenticide; Lethal dosage; Toxic hepatitis; Acute liver failure; Acute kidney injury; Multiple organ failure; International normalized ratio
Introduction
Rodenticides for many years have been an important cause of significant morbidity and mortality in patients who present to an emergency room with deliberate self-harm. An annual incidence of 500,000 cases has been reported [1]. Reports showed that the rate of poisoning in developing countries ranges from 0.07 to 0.7% [2]. As per National Crime Records Bureau (NCRB) statistics, about 1,31,666 people lost their lives by committing suicide during the year 2014 in India. Poisoning was observed to be the second most common method of suicide (National Crime Records Bureau [3]. In India, suicidal or accidental poisoning with rodenticides containing metal yellow phosphorous (Ratol® which has ZnP in paste form) is a more frequent cause of drug-induced ALF than paracetamol [4]. Renal failure and cardiac failure due to toxic cardiomyopathy were the commonest secondarily affected systems leading to rapid mortality [5]. A recent study conducted in South India showed that yellow phosphorus was the most common rodenticide used in suicide attempts in the region and carried a 30% mortality despite maximal supportive therapy [6]. The severe clinical symptoms in patients with phosphine poisoning include circulatory collapse, hypotension, pulmonary edema, congestive heart failure, cardiac arrhythmia, and acute renal failure [7]. Both hyperglycemia and hypoglycemia have been reported as clinical features of phosphide poisoning [8]. No specific antidote has been identified; therefore, the main treatment is supportive care. Although some efforts have been made to establish more effective interventions and medications for management, the mortality rate remains high [9-11]. This fatal poison is freely available over the counter in toxic doses at very cheaper prices [12].
Materials and Methods
Study population
101 admitted patients who ingested rat killer poison with suicidal intention. Inform consent forms were received from all patients.
Sample collection and analysis
Patients were screened by clinicians for clinical findings. Patient’s age, socio-demographic, anthropometric, and biological markers were tested. Psychiatric analysis revealed Para suicide rather than true intention to die and none had underlying psychosis.
Lists of test conducted
Blood screening for Total protein [13], (Total bilirubin, Urea, Creatinine) [14], (Alanine aminotransferase (ALT), Alkaline phosphate (ALP) [15], Aspartate aminotransferase (AST) [16], Platelet count [17] Albumine [18], PT [19], INR [20] and MELD [21] were done and serial charting of biological markers were recorded. Standard care management was given.
Quality control
To ensure quality control, normal and abnormal assays were performed along with the test and recorded.
Statistical analysis
Continuous variables are expressed as means and standard deviations and categorical variables as numbers with percentages in brackets. Sub-group analysis of biological markers were done between survivor and non-survivor which was expressed as P-value (<0.005).
Results
Table 1 shows the socio-demographic characteristics of patients ingested rat killer poison. Of the 101 patients 77 (76%) were from rural areas and 24 (24%) were urban. Two thirds were female and the rest males with 62% and 38%. Age group ranged from 15-65 with mean value of 26.0 ± 10.467 years. Most of the patients (45%) ranged between 20-30 years of their age. Thinking that marital status may be a factor, we compared the marital status with the gender of the patients who ingested poison and found that unmarried men were higher among the men who ingested poison and among the women married women were higher than unmarried women. Whether women or men, literacy level of the them also studied which revealed that higher number of patients who ingested poison were literate with schooling 47 (46%). Illiterate with no formal education were 28 (28%). Details on patient’s occupation were collected and higher number of patients who ingested were Professionals or salaried 46 (45%) followed by students 30 (30%).
| Characteristics | All households | |
|---|---|---|
| n=101 | Percentage (%) | |
| Place of residence | ||
| Rural | 77 | 76 |
| Urban | 24 | 24 |
| Gender | ||
| Male | 38 | 38 |
| Female | 63 | 62 |
| Age group (in years) | ||
| <20 | 31 | 31 |
| 20-30 | 46 | 45 |
| 30-40 | 15 | 15 |
| >40 | 9 | 9 |
| Mean ± SD | 26.0 ± 10.467 | |
| Marital status | ||
| Unmarried men | 27 | 27 |
| Married men | 11 | 11 |
| Unmarried women | 28 | 28 |
| Married women | 35 | 35 |
| Literacy status of the patients | ||
| Illiterate with no formal education | 28 | 28 |
| Literate with schooling | 47 | 46 |
| Literate with graduation | 26 | 26 |
| Occupation | ||
| Housewives | 16 | 16 |
| Coolies | 9 | 9 |
| Professionals or salaried | 46 | 45 |
| Students | 30 | 30 |
Table 1: Socio-demographic characteristics of patients ingested rat killer poison.
Table 2 shows the mode of ingestion of rat killer poison, lethal dosage and its related profile. Of 101 patients, 34 (34%) of them had it raw, 30 (30%) ingested rat killer poison mixed with water. For any poison, lethal dosage is important to cause illness or death in human. In our study we found that 57 (57%) of the patients took only <10 grams and 24 (24%) of them took up to 20 grams and 20 (20%) of them took more than 20 grams. We found that mean dosage of 13.42 ± 7.069 grams can cause any illness or death to human. Followed by the ingestion, the care givers or parents or friends, carried the patient to health facility was calculated. The mean time taken for care seeking was 6.0 ± 6.3702 hours. The patients sought care in health facility from the onset of symptom were 88 (87%), of them 46 (46%) sought care with 3 hours and 42 (41%) within 10 hours. There were 13 (13%) of them who visited health facility only after 10 hours of poison ingestion.
| Related profile of ingestion of rat killer poison | All Households | |
|---|---|---|
| n=101 | Percentage (%) | |
| Mode of ingestion of rat killer poison | ||
| Raw | 34 | 34 |
| Mixed with water | 30 | 30 |
| Mixed with alcohol | 20 | 20 |
| Mixed with food | 17 | 17 |
| Lethal dosage (in grams) | ||
| <10 | 57 | 56 |
| 11-20 | 24 | 24 |
| >20 | 20 | 20 |
| Mean ± SD | 13.42 ± 7.069 | |
| Care seeking time (in hours) | ||
| <3 | 46 | 46 |
| 03-10 | 42 | 41 |
| after 10 | 13 | 13 |
| Mean time taken for care seeking (Mean ± SD) | 6.0 ± 6.3702 | |
| Time of manifestation of first chief symptoms (in hours) | ||
| <6 | 71 | 70 |
| 06-12 | 25 | 25 |
| >12 | 5 | 5 |
| Mean ± SD | 5.7 ± 6.3093 | |
| Most common chief symptoms* | ||
| Vomiting | 79 | 33 |
| Abdominal pain | 87 | 36 |
| Head ache | 65 | 27 |
| Oral Bleeding | 10 | 4 |
Table 2: Mode of ingestion of rat killer poison, lethal dosage and its related profile; [*Multiple responses].
After the patients arrived to health facility with the symptoms, details of time of manifestation of first chief symptoms was recorded. Time of manifestation of chief symptoms started in 71 (71%) patients within 6 hours, in 25 (25%) between 6-12 hours and in 5 (5%) of patients, manifestation of symptoms started only after 12 hours of ingestion of rat killer poisoning with the mean and standard deviation of 5.7 ± 6.3093 hours. Once the manifestation of symptoms started in patients, the symptoms were also recorded which revealed that most common presenting symptom was vomiting in 79 (33%) patients followed by abdominal pain in 87 (36%) and headache 65 (27%) Oral bleeding was also reported in 10 (4%) patients. Multiple responses were given by patients.
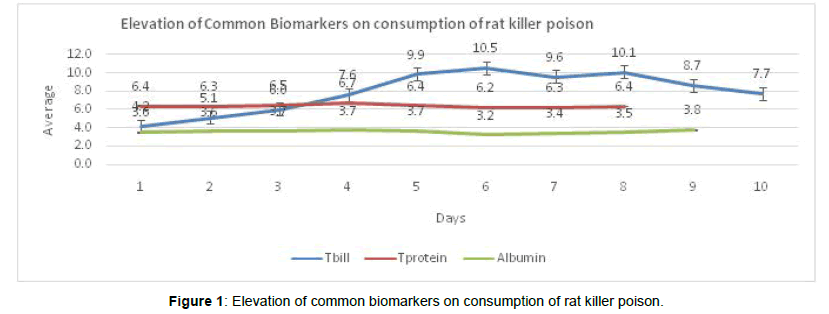
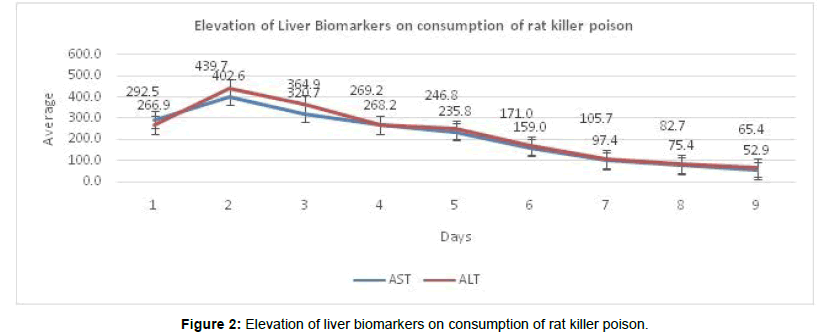
As soon as the symptoms started in patients there was a need for evaluation of biological markers. Samples were collected for all the biological markers and the results showed that T. billrubin were elevated from the 4th day to 8th day of ingestion of rat killer poison and there was high peck level on 6th day with the value of 10.5 mg/dl. Both T. protein and albumin did not show many changes during the hospital stay (Figure 1). Among the biological markers, enzymes like Aspartate amino transferase (AST) and Alanine aminotransferase (ALT) showed higher level of elevation on 2nd day of admission. Among the liver enzymes, ALT showed 439.7 Iu/ml and AST was 402.6 Iu/ml (Figure 2).
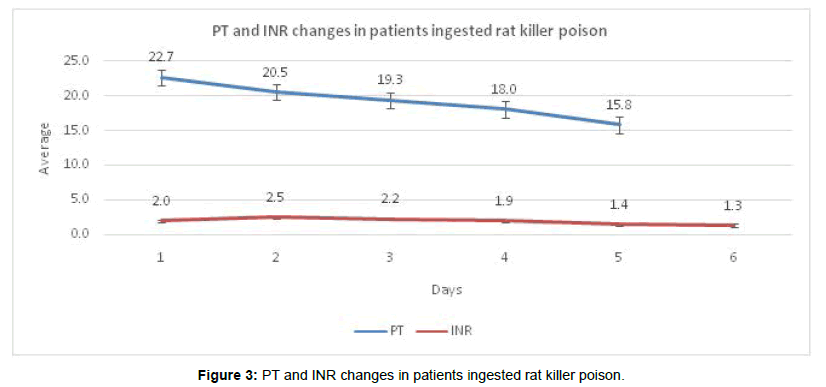
Along with biological marker, Prothrombine Time (PT) was also diagnosed and PT showed reduction and INR did not show any change. The International normalized ratio (INR) was <2 in 69 patients, 2-3 in 11 patients and >3 INR in 21 patients (Figure 3). We performed the sub-group analysis of biological markers recorded in patients who survived and non-survivor in spite of treatment. T. bill, Albumin, AST, ALT, Creatinine, PT, INR and MELD were statistical significant (P value=0.005). T. protein, platelet and urea did not show statistical significance. Among the 101 patients, 9 had a MELD of <10, 30 were in 11-20 range, 35 in 21-30 and >30 MELD was found in 27 patients. All of those having a MELD of >40 died (Table 3).
| Elevation of bio Markers | All Households (n=101) | P-value | |
|---|---|---|---|
| Bio markers | Outcome of treatment | ||
| Non-Survivors (n=19) 19% | Survivors (n=82) 81% | ||
| Mean ± SD | Mean ± SD | ||
| T. bill | 8.105 ± 5.3559 | 3.294 ± 3.8375 | 0.000* |
| T. protein | 6.232 ± 0.4750 | 6.442 ± 0.5924 | 0.153 |
| Platelet | 1844.1 ± 8029.06 | 5742.7 ± 19224.8 | 0.623 |
| Albumin | 3.299 ± 0.4225 | 3.639 ± 0.4662 | 0.005* |
| AST | 700.11 ± 518.728 | 198.05 ± 278.388 | 0.000* |
| ALT | 648.53 ± 418.914 | 178.41 ± 230.159 | 0.000* |
| Urea | 34.53 ± 13.773 | 26.90 ± 9.316 | 0.011* |
| Creatinine | 1.268 ± 0.8628 | 0.849 ± 0.2564 | 0.004* |
| PT | 31.606 ± 15.3415 | 20.503 ± 9.8842 | 0.006* |
| INR | 3.3816 ± 1.64122 | 1.6732 ± 0.75412 | 0.000* |
| MELD | 35.47 ± 8.455 | 21.43 ± 8.346 | 0.000* |
Table 3: Elevation of biological markers between recoded results of patients of non-survivor and survivor after ingestion of rat killer poison; [*p value <0.01 as statistical significant].
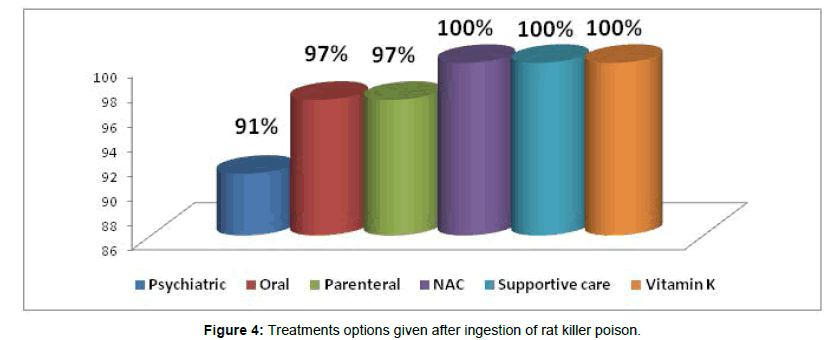
On the basis of biological markers the patients were treated with different method of treatment directed at removal of the poison and supportive therapy. 101 (100%) of patients received treatment like NAC, Supportive therapy and Vitamin-K. 97 (97%) received oral and parental treatment and 91 (91%) patients received Psychiatric treatment (Figure 4). In spite of effective treatment, 41% of patients developed Toxic Hepatitis (TH), 21% showed Acute Liver Failure (ALF) as soon as they ingested rat killer poison. Among the remaining 38% of patients, 19% developed Toxic Hepatitis along with Acute Kidney Injury/ALF along with Acute Kidney Injury. 19% of the patients who ingested rat killer poison developed multiple organ failure which was the reason for their death. The death rate in our study was 19% who developed multiple organ failure. The other 82 patients recovered with mean hospital duration of 8.88 days (Figure 5).
Discussion
Among the 101 patents in our study, Professionals or Salaried were higher followed by students. In a study by Suneetha et al. homemakers were higher followed by students [22]. Various studies on poisoning done in India Banerjee et al. [23] in west Bengal also noticed most commonly effected age group was 20-40 years. Our study was compatible with Banerjee et al. in the age group. In a study in Thailand by Satariya et al. [24] found that higher number of patient ingested rat killer poisoning mixing with alcohol but our study showed that, many patients ingested either raw or mixed with water.
New finding in our study was the mean lethal dosage (13.42 ± 7.069 gms) of rat killer poisoning which will cause damage to the organs once ingested. Other new finding of our study was manifestation of first chief symptoms which was 5.7 ± 6.3093 hours. “People must seek care in the health facility as soon as they have identified the ingestion of rat killer poison”. Saoji AA et al. [10] found in her study that the patients were usually asymptomatic during the initial 72 hour of ingestion, or they may have signs and symptoms of gastrointestinal irritation. Our patients in our study developed symptoms from 5 to 6 hours and vomiting was found in higher number in our patients.
Blotting the biological marker AST and ALT showed higher elevation in patients ingested rat killer poison which indicates that the first affecting organ was liver followed by kidney and other organs. AST was 402.6 on the 2nd day and on 6th day AST reduced to 159.0. Alt was 439.7 on the 2nd day and reduced on 6th day to 171.0. Bhat et al. [1] study showed, the mean admission ALT/AST was 306/451, discharge ALT/AST was 291/302, and peak ALT/AST was 451/655. Few other new findings in our study were elevation graphs were shown for T.bill, T.protein, Albumine, AST, ALT, urea, creatinine, PT and INR for all the patients who ingested rat killer poisoning. Our study again found the statistical significant elevation biological elevation between the survivor and non-survivor.
We found out of 100% patients received treatments like NAC, Vit-K, supportive, 82% of our patients survived and discharged. Mishra AK et al. [25] reveals best results seen among patients in whom NAC was started early in the course of illness. Guidelines do not exist regarding routine use of NAC in non-acetaminophen induced ALF, and in hepatic failure due to rodenticide consumption. Patients admitted with ALF after phosphorus ingestion has sometimes been managed with NAC [26]. We strongly recommend that it is a need of hour to frame proper guidelines of treatment that ingest rat killer poison. However in spite of manageable treatment, half of our patient developed Toxic Hepatitis, 1/3 developed Acute Liver Failure and ¼ developed Toxic Hepatitis along with Acute Kidney Injury / Acute Liver Failure along with Acute Kidney Injury. ¼ developed multiple organ failure which leads them to death. Murali et al. [6] showed 35.7% mortality rate whereas our study showed 19% mortality rate. Survived patients received psychiatric evaluation and were discharged in a stable condition.
Conclusion
Almost all patients with rodenticide poisoning containing yellow phosphorus had liver injury. Lethal dosage and late presentation to medical facility led to development of acute liver failure and mortality in spite of standard of care treatment. Multisystem involvement is almost always fatal. Creating awareness, promoting mental health and suicide prevention is the best option to reduce mortality from such poisonings.
Already Known
• Age, marital status, gender or education level did not play a role in suicidal intention in patients ingested rat killer poison.
• Lethal dosage like in grams were already known factor.
• Signs and symptoms of gastrointestinal irritation.
• Patients received treatments like NAC, Vitamin-K, supportive.
New Findings
• Mean dosage of 13.42 ± 7.069 grams can cause any illness or death to human.
• The mean time taken for care seeking was 6.0 ± 6.3702 hours.
• Manifestation of first chief symptoms which was 5.7 ± 6.3093 hours. “People must seek care in the health facility as soon as they have identified the ingestion of rat killer poison”.
• Elevations of Biomarkers during the hospital stay were blotted.
• However in spite of manageable treatment, half of our patient developed Toxic Hepatitis, 1/3 developed Acute Liver Failure and ¼ developed Toxic Hepatitis along with Acute Kidney Injury/Acute Liver Failure along with Acute Kidney Injury. ¼ developed multiple organ failure which leads them to death.
Ethical Clearance
Study was conducted in accordance with ethics research comity and ethical clearance was obtained from ethics research comity of institutional review board.
References
- Bhat S, Kenchetty KP (2015) N-acetyl cysteine in the management of rodenticide consumption-life saving? J Clin Diagn Res 9: OC10-13.
- Zöhre E, Ayrık C, Bozkurt S, Kose A, Narci H, et al. (2015) Retrospective analysis of poisoning cases admitted to the emergency medicine. Arch Iran Med 18: 117-122.
- National Crime Records Bureau (2015) Accidental deaths and suicides in India, 2014. Ministry of Home affairs, Govt. of India, New Delhi.
- Aniket AS, Anurag SL, Harsha RS (2014) A Case on suicidal poisoning associated with ratol and a perspective on yellow phosphorus poisoning. Int J Recent Trends Sci Technol 10: 223-225.
- Saraf V, Pande S, Gopalakrishnan U (2015) Acute liver failure due to zinc phosphide containing rodenticide poisoning: Clinical features and prognostic indicators of need for liver transplantation. Indian J Gastroenterol 34: 325-329.
- Nalabothu M, Monigari N, Acharya R (2015) Clinical profile and outcomes of rodenticide poisoning in tertiary care hospital. Int J Sci Res Publ 5: 1-12.
- Dogan E, Guzel A, Ciftci T (2014) Zinc phosphide poisoning. Case Rep Crit Care.
- Jamshed N, Ekka M, Aggarwal P (2014) Severe hypoglycemia as a presenting feature of aluminum phosphide poisoning. Ann Saudi Med 34: 189.
- Marashi SM (2015) What really happens after zinc phosphide ingestion? A debate against the current proposed mechanism of phosphine liberation in zinc phosphide poisoning. Eur Rev Med Pharmacol Sci 19: 4210-4211.
- Saoji AA, Lavekar AS, Salkar HR (2014) A case on suicidal poisoning associated with ratol and a perspective on yellow phosphorus poisoning. Int J Recent Trends Sci Technol 10: 223-225.Â
- Singh S, Bhalla A (2015) Aluminum Phosphide Poisoning. J Mahatma Gandhi Ins Med Sci 20: 15-19.
- Hu J, Zhang Q, Ren X (2015) Efficacy and safety of acetylcysteine in “non-acetaminophen†acute liver failure: A meta-analysis of prospective clinical trials. Clin Res Hepatol Gastroenterol 39: 594-599.
- Tietz NW (1970) Fundamentals of clinical chemistry. WB Saunders CoPhiladelphia, USA pp: 481-495.
- Tietz N W. (1986) Fundamentals of clinical chemistry. WB Saunders CoPhiladelphia, USA.
- Young DS (1990) Textbook of Clinical Chemistry, Effects of drugs on Clinical Laboratory Tests. (3rd edn), WB Saunders, USA.
- Ault KA, Mitchell J, Knowles C (1997) Implementation of the immunological platelet count on a haematology analyser, the Abbot CELL-DYN 4000. Lab Haematol 3: 125-128.
- Savory J, Hammond J (1980) Measurement of proteins in biological fluids.
- Kamal AH, Tefferi A, Pruthi RK (2007) How to interpret and pursue an abnormal prothrombin time, activated partial thromboplastin time, and bleeding time in adults. Mayo Clin Proc 82: 864-873.
- WHO Expert Committee on Biologic Standardization (1983) 33rd Report, Technical Report Series No 687. World Health Organization, Geneva.
- Malinchoc M, Kamath PS, Gordon FD (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31: 864.
- Suneetha (2016) Profile of rat killer poisoning cases in a tertiary care hospital at Mysore. Int J Sci Study 12: 264-267.
- Banerjee I, Tripathi SK, Roy AS (2014) Clinico-epidemiological profile of poisoned patients in emergency department: A two and half year's single hospital experience. Int J Crit Illn Inj Sci 4: 14-17.
- Trakulsrichai S, Ksanyawat N, Atikasawedparit P (2017) Clinical Characteristics of zinc phosphide poisoning in Thailand. Ther Clin Ris Mang 13: 335-340.
- Mishra AK, Devakiruba NS, Jasmine S (2016) Clinical spectrum of yellow phosphorous poisoning in a tertiary care centre in South India: A case series. Trop Doct 47: 245-249.
- Squires RH, Dhawan A, Alonso E (2013) Intravenous N-acetylcysteine in pediatric patients with non-acetaminophen acute liver failure: A placebo controlled clinical trial. Hepatology 57: 1542-1549.
Citation: Venugopal R, Narayanasamy K, Chezhian A, Senthil Kumar R, Jasmine JJ (2018) Rat Killer Poisoning vs. Liver Damage: A View in South Indian Patients of Tertiary Care Center. J Gastroint Dig Syst 8: 569. DOI: 10.4172/2161-069X.1000569
Copyright: © 2018 Venugopal R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 24313
- [From(publication date): 0-2018 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 23005
- PDF downloads: 1308