"Real World" Factors Influencing Dropout from Opiate Treatment with Methadone and Buprenorphine
Received: 26-Feb-2018 / Accepted Date: 18-Apr-2018 / Published Date: 25-Apr-2018 DOI: 10.4172/2155-6105.1000360
Abstract
Background and objective: Comparison of retention in office-based, private-pay, outpatient opiate treatment programs with methadone or buprenorphine. Methods: Descriptive study with a prospective design comparing treatment retention in a licensed Opiate Treatment Program (OTP) and buprenorphine program (BUP) offered in the same office-based setting. Over a period of 4.5 years, 1,372 patients were observed from program admission until six months or dropout, whichever was earlier. Results and conclusion: OTP had greater retention than BUP (36% vs. 15.8%); however, in both programs, retention was lower than reported elsewhere. Hispanic ethnicity, being married, and being unemployed correlate with significant dropout in OTP. Causes of early drop out in BUP were unclear. Percent of positive urine drug screens were significantly associated with drop out in both modalities. Significance: Results reflect the situation in a private pay outpatient program where patients are financially responsible for medications, transportation, and services. This, in addition to higher percentage of Hispanic ethnicity in study population and continuation of abuse of illicit substances, might explain overall low retention. Government supported treatment should improve retention in “real world” opiate dependence maintenance treatment.
Keywords: Opiate dependence; Methadone; Psychiatric illness
Background and Objective
Treating heroin addicted patients pharmacologically with methadone had been the standard of care since the late 1960’s [1]. The Drug Addiction Treatment Act (DATA) of 2000 permits qualified physicians to obtain a waiver to prescribe opioid medications to treat opioid addiction [2]. This allowed qualified physicians to prescribe and dispense buprenorphine in an office-based setting.
Unlike methadone treatment, which is highly restricted, buprenorphine expands treatment opportunities to primary and specialty physician offices [3,4]. Opiate-dependent patients that are prescribed buprenorphine are not required to attend the prescriber’s office daily (as with methadone). Buprenorphine has other major advantages over methadone: withdrawal symptoms are milder, so reducing doses is easier; the duration of action is longer; and buprenorphine is less likely to cause respiratory depression, overdose, and death [4]. However, it is still unclear if patients will stay in treatment with buprenorphine as long as with methadone, and what factors determine early dropout [3].
This study focused on comparing retention in treatment at 3 and 6 months in 1,392 patients over a period of 4.5 years in a private practice that prescribed both buprenorphine and methadone as primary pharmacologic treatment. “Real world” factors that may have influenced the retention were examined.
Methods
The study was carried out in a large Texas metropolitan community with a large Hispanic population. We compared retention in treatment at 3 and 6 months in an Opiate Treatment Program (OTP) and a buprenorphine office-based program that operated at the same central city site and employed shared professional staff. The same two physicians treated all of the study patients with either buprenorphine (BUP) or methadone (OTP). The remaining staff consisted of licensed vocational nurses (LVNs), licensed chemical dependency counselors (LCDCs) and front office personnel.
The Texas Department of State Health Services (TDSHS), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Commission on Accreditation of Rehabilitation Facilities (CARF) and the Drug Enforcement Agency (DEA) credentialed the OTP to dispense methadone. The physicians were credentialed under the DATA 2000 Act to prescribe buprenorphine medication, and each physician had a 100 patient waiver [2].
Both OTP and BUP had the same hours of operation (5:30 AMnoon weekdays, 6:30 AM-10 AM Saturdays, and 8 AM-10 AM Sundays). Both groups of patients had access to at least one physician during office hours. A physician was on call 24 h/day, 7 days a week.
Patients were admitted to either program based on minimum standards for narcotic treatment programs according to 25 Texas Administrative Code (§§229.141-229.153); SAMSHA: 42 CFR part 8 rules; CARF regulations; and Diagnostic and Statistical Manual of Mental Disorders (DSM-IV TR) criteria for opioid dependence [5-7]. Admission criteria for both programs were DSM-IV-TR diagnostic criteria for substance dependence confirmed by the physician [7]. These were also considered as inclusion criteria for our study. Pregnant patients were not included in the study. Patients with severe psychiatric illness; known past, current, or threatened violence; refusal of consent for release of information from previous health providers or clinics; or inability or unwillingness to sign informed consent were not admitted and thus excluded from the study. Patients were only admitted for maintenance therapy and were not admitted for detoxification or treatment for other substances of abuse (such as alcohol, cocaine or amphetamines).
Factors taken into consideration for program selection by patients and physicians were (a) cost of medications and transportation; (b) potential complications and risks from either treatment; (c) details of current and prior substance abuse treatment; (d) preferences and reliability for prescription BUP vs. daily OTP dispensing (e) importance of counselling (f) medical and psychiatric needs of the patient. Once a decision was made for admission, patients underwent induction as per the orders from the physician.
In both treatment modalities, patients were given doses for induction and maintenance that controlled symptoms and signs of withdrawal and reduced cravings. Physician saw OTP patients regularly every three months unless there were requested dose changes or medical/psychological issues. BUP patients were required to see a physician each month before they could receive a prescription for buprenorphine. LCDC saw patients from both groups on a monthly basis during maintenance phase.
LCDCs counseled both groups of patients in (a) developing treatment plans, (b) provided patients with information on substance abuse prevention, employment, and rehabilitation, (c) provided legal information regarding probation and parole, and (d) discussed psychosocial issues with patients and families. Efforts were made to improve patients’ family relationships, provide referral to community resources and to primary and secondary care providers. Almost all of the patients from both groups felt very positive about their LCDC relationship. Under no show for counseling appointments, attempts were made to contact them by phone to reschedule the visit.
Cash or credit card payments for both OTP and BUP were due at the time of clinic visit. Starting fee was $100 for OTP and $200 for BUP. In both programs, each patient received a physical examination, tuberculosis skin test, electrocardiogram, complete blood count, chemistry panel, routine urinalysis, syphilis serology, and a urine drug screen (UDS) on admission. OTP patients paid $10/day for methadone, medical services from the 2 board-certified physicians, and for counseling. BUP patients paid $150 for each follow up visit plus the cost of the buprenorphine prescription. Thus, on a monthly basis, clients from both OTP and BUP would pay approximately $300 per month. The clinic was not a Medicare or Medicaid provider, and did not bill insurances, but patients with insurance could submit a claim themselves.
Nurses observed and dispensed the methadone for OTP patients daily throughout their time in the treatment. Unstable patients or those requesting dose adjustments required a physician visit before dosing.
The physician saw the BUP patients during induction, then once a month during maintenance. If they had a positive drug screen for other than buprenorphine, or did not have buprenorphine present, they would have to been seen more frequently. In BUP, nurses and counselors saw patients only prior to monthly physician visits, unless clients made special appointments with their counselor for specific issues.
Induction doses of methadone given initially were 10 to 30 mg/day depending on the degree of estimated tolerance and were raised over the first several weeks to a maintenance dose level. The mean maintenance dose of methadone (including induction doses) was 60 mg/day. Buprenorphine mean maintenance dose was 12 mg/day with initial induction doses adjustments. All patients in BUP group were prescribed a non-generic buprenorphine-naloxone combination.
Monthly UDS for OTP patients were requested randomly to total 12 drug screens per year. In addition, some patients required UDS exam by dipstick when they appeared unstable. Urine samples for BUP patients were examined only during monthly physician visits by dipstick method prior to the physician visit. The results would determine the buprenorphine dose and time to next visit. In both programs, observed urine collections were done if there was suspicion of tampering. All OTP urine samples were tested qualitatively (positive/negative) for opiates, methadone metabolite, barbiturates, benzodiazepines, amphetamines, and cocaine. Urine samples of BUP patients were tested for the presence of all the above-mentioned drugs except methadone metabolite and for presence of BUP to confirm compliance.
Clinic policy was to discharge clients from the OTP program if they failed to show up for treatment for 14 consecutive days, and BUP clients were discharged after no show/no contact for two consecutive months. These were also considered as end points for drop out from our study. Other than discharge for non-payment, administrative discharges were very uncommon and thus were included in the study. Patients readmitted to either program after initial drop-out was not included for analysis in the study. Very few patients switched the programs and were not included in the study.
The clinic utilized an electronic medical record system to store patient records.
Informed consent
Written informed consent for usage of the data was obtained for each patient, and the Institutional Review Board of the University of Texas School Of Public Health, Houston, approved the collection and analysis of the data. Anonymity was protected for each patient and all were de-identified throughout the analysis. No patient under 18 years of age was included in the data set.
Data Analysis
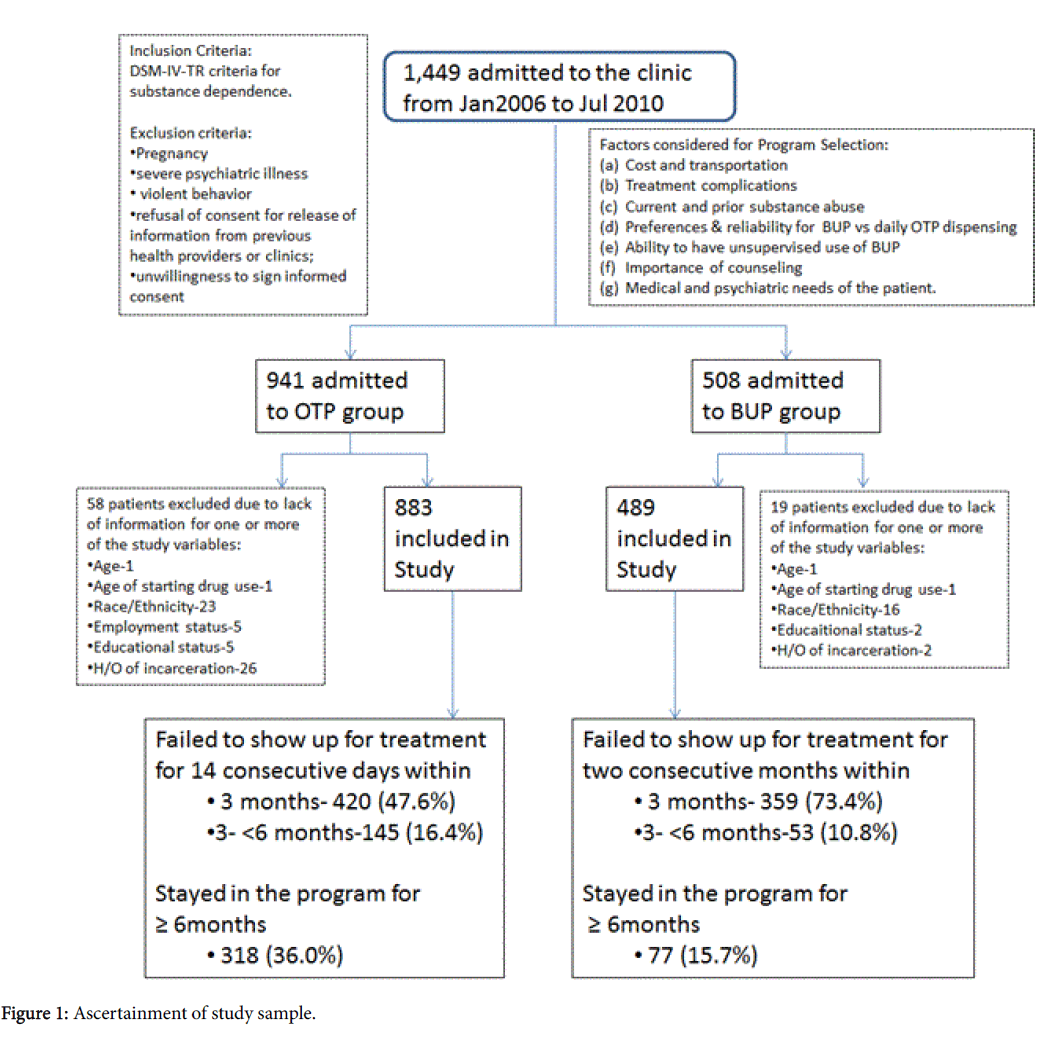
De-identified data of 1,449 patients admitted to the clinic were obtained from clinic’s electronic medical records. Nine hundred and forty one (941) of these patients were in the OTP group and 508 were in the BUP group. Seventy-seven patients (58 in OTP and 19 in BUP) were excluded from the statistical analysis because of lack of information on one or more of the study variables. Figure 1 shows in detail the ascertainment of the study sample. Descriptive tables and Cox proportional hazard models were constructed on the remaining 1,372 patients using STATA Version 12 statistical program to estimate the association between the study variables (ethnicity, marital status, employment, education, history of incarceration, age of starting drug use, route of drug administration, positive urine drug screens) and dropout rate among participants [8-10].
Results
Of the 1372 participants, 883 (64%) were in the methadone (OTP) subsample; 489 (36%) were in the buprenorphine (BUP) subsample. Table 1 compares the demographic and clinical characteristics of the patients at baseline for both groups. The two treatment modalities differed significantly for all study variables except age and gender. The OTP group had high percentages of Hispanic ethnicity (62.5% vs. 33.5%), unemployment (54.5% vs. 41.5%), and less than high school education (30.8% vs. 11.9%) as well as higher rates of incarceration (69.3% vs. 48.1%) compared to the BUP group. Although the mean age of starting drug use (21.7 years vs. 25.6 years) and years of addiction (10.8 vs. 6.9) also differed significantly between the groups, these might not translate to clinical relevance. Intravenous drug use (heroin) was high in the OTP group compared to the BUP group (80.0% vs. 49.3%). There was less prescription drug abuse in the OTP group (12.4%) than in the BUP group (52.8%). Concomitant use of cocaine was high in OTP group (31.5% vs. 17.2%) while the BUP group had high percentages of benzodiazepine abuse (26.1% vs. 38.9%).
| Characteristics | OTP (N=883) | BUP (N=489) | p-value* | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age at Admission (Years) | 32.5 | 10.3 | 32.5 | 11.1 | 0.4459 |
| N | % | N | % | p-valueƗ | |
| Female Gender | 298 | 33.8 | 180 | 36.8 | 0.254 |
| Hispanic Ethnicity | 552 | 62.5 | 164 | 33.5 | <0.001 |
| Unemployed | 481 | 54.5 | 203 | 41.5 | <0.001 |
| 27230.85811.9<0.001 | |||||
| Married | 460 | 52.1 | 223 | 45.6 | 0.021 |
| With H/O Incarceration | 612 | 69.3 | 235 | 48.1 | <0.001 |
| Mean | SD | Mean | SD | p-value* | |
| Age of Starting Drug use | 21.7 | 7.2 | 25.6 | 10.2 | <0.001 |
| Years addicted | 10.8 | 9.7 | 6.9 | 8.2 | <0.001 |
| N | % | N | % | p-valueƗ | |
| IV Drug use (Heroin) | 701 | 80 | 240 | 49.3 | <0.001 |
| Prescription drug abuse | 109 | 12.4 | 257 | 52.8 | <0.001 |
| Amphetamine abuse | 57 | 6.5 | 26 | 5.3 | 0.397 |
| Benzodiazepine abuse | 230 | 26.1 | 190 | 38.9 | <0.001 |
| Cocaine abuse | 278 | 31.5 | 84 | 17.2 | <0.001 |
Table 1: Demographic and clinical characteristics of the subjects by treatment group at the time of admission into the program; *p-values from Wilcoxon rank sum test, Ɨ p-values from Chi Sq. test.
Of the OTP group, 565 (64%) dropped out less than 6 months after admission; in the BUP group, 412 (84.2%) dropped out before 6 months. Mean duration in OTP was 103.2 days; mean duration in BUP was 55 days. Table 2 summarizes the retention rates in both groups at less than 3 months, 3 to 6 months, and greater than 6 months and compares them by study variable characteristics within each group. Almost 73.4% of the BUP program participants dropped out by 3 months while 52.4% of OTP participants dropped out in less than 3 months. In the OTP group, the retention rates at these time intervals were found to be significantly associated with Hispanic ethnicity, unemployment, education, marital status, concomitant use of cocaine and percent of positive UDS. In the BUP group, heroin use, prescription drug abuse, concomitant cocaine use and percent of positive UDS were reversely associated with length of stay in the program.
| Characteristics | OTP (n=883) | BUP (n=489) | ||||||
|---|---|---|---|---|---|---|---|---|
| 3 to>=6 months 318 (36.0%) 3 to>=6 months 77 (15.7%) | ||||||||
| Age at Admission (Years) | Mean (SD) | Mean (SD) | Mean (SD) | p-valuea | Mean (SD) | Mean (SD) | Mean(SD) | p-valuea |
| 31.8 (10.3) | 32 (10.2) | 33.7 (10.3) | 0.01 | 31.3 (10.9) | 36.6 (13) | 35 (9.9) | <0.001 | |
| N (%) | N (%) | N (%) | p-valueb | N (%) | N (%) | N (%) | p-valueb | |
| Female Gender | 147 (35) | 50 (34.5) | 101 (31.8) | 0.641 | 133 (37.1) | 17 (32.1) | 30 (39) | 0.714 |
| Hispanic Ethnicity | 302 (71.9) | 89 (61.4) | 161 (50.6) | <0.001 | 130 (36.2) | 15 (28.3) | 19 (24.7) | 0.105 |
| Unemployed | 269 (64.1) | 73 (50.3) | 139 (43.7) | <0.001 | 160 (44.6) | 18 (34) | 25 (32.5) | 0.074 |
| 154 (36.7)192 (34)192 (34)0.00243 (12)48 (11.7)48 (11.7)0.82 | ||||||||
| Married | 249 (59.2) | 64 (44.1) | 147 (46.2) | <0.001 | 162 (45.1) | 22(41.5) | 39 (50.7) | 0.554 |
| With H/O Incarceration | 305 (72.6) | 97 (66.9) | 210 (66) | 0.125 | 178 (49.6) | 21 (39.6) | 36 (46.8) | 0.387 |
| Mean (SD) | Mean ( SD) | Mean (SD) | p-valuea | Mean (SD) | Mean (SD) | Mean (SD) | p-valuea | |
| Age of Starting Drug use | 21.4 (7.1) | 22 (7.1) | 21.8 (7.4) | 0.558 | 24.9 (9.7) | 27.7 (12.2) | 27.6 (10.6) | 0.091 |
| Years addicted | 10.3 (9.6) | 10.1 (10.3) | 11.9 (9.5) | 0.001 | 6.5 (8) | 8.9 (10.5) | 7.3 (7.3) | 0.074 |
| Length of Stay (Days) | 37.1 (22.6) | 126 (25) | -(-) | 16.9(22.8) | 131.3(26.1) | -(-) | ||
| % Positive UDS | 90.3 (26.3) | 68.3 (32.8) | 59.2 (32.9) | <0.001 | 73.4 (36.5) | 49.7 (32.7) | 35.2 (28.7) | <0.001 |
| N (%) | N (%) | N (%) | p-valueb | N (%) | N (%) | N (%) | p-valueb | |
| IV Drug use (heroin) | 341 (81.2) | 112 (77.2) | 248 (80) | 0.446 | 193 (53.8) | 24 (45.3) | 23 (29.9) | 0.004 |
| Prescription drug abuse | 56 (13.3) | 21 (14.5) | 32 (10.1) | 0.36 | 168 (46.8) | 30 (56.6) | 59 (76.6) | <0.001 |
| Amphetamine abuse | 25 (6) | 9 (6.2) | 23 (7.2) | 0.775 | 24 (6.7) | 1 (1.8) | 1 (1.3) | 0.08 |
| Benzodiazepine abuse | 113 (26.9) | 38 (26.2) | 79 (24.8) | 0.818 | 138 (38.4) | 23 (43.4) | 29 (37.7) | 0.766 |
| Cocaine abuse | 172 (41) | 33 (22.8) | 73 (23) | <0.001 | 72 (20.1) | 5 (9.4) | 7 (9.1) | 0.02 |
Table 2: Descriptive statistics by length of stay in the program and by treatment group; aKruskal-Wallis test p-values, bChi Sq. test p-values.
Cox proportion hazard model (Table 3) for failure to show up for treatment for 14 consecutive days within 6 months in OTP group demonstrated that after adjusting for age, gender and other covariates, patients of Hispanic ethnicity were more likely to drop out from OTP (Hazard Ratio: 1.52 (CI: 1.25-1.84, p<0.001)). Being married (Hazard Ratio: 1.48 (CI: 1.25-1.75, p<0.001)) and being unemployed (Hazard Ratio: 1.43 (CI: 1.20-1.71, p<0.001)) were also associated with significant dropout hazard ratios. For each 10% increase in positive UDS, the odds of dropping out of the OTP program within six months increased by 22% (Hazard Ratio: 1.22 (CI: 1.18-1.26, p<0.001)).
| Variables | Failure within 6 months (OTP)* | Failure within 6 months (BUP)** | ||||
|---|---|---|---|---|---|---|
| Hazard Ratio | (95% CI) | p-value | Hazard Ratio | (95% CI) | p-value | |
| Age at Admission | 0.99 | (0.98-0.99) | 0.022 | 0.99 | (0.97-1.00) | 0.089 |
| Gender (Female) | 1.05 | (0.88-1.25) | 0.618 | 1.04 | (0.79-1.38) | 0.77 |
| Race/Ethnicity (Caucasian) | 1.53 | (1.26-1.86) | <0.001 | 0.92 | (0.70-1.22) | 0.569 |
| Marital status (Other) | 1.46 | (1.24-1.73) | <0.001 | 0.85 | (0.65-1.10) | 0.221 |
| Unemployment (Employment) | 1.44 | (1.21-1.71) | <0.001 | 1.07 | (0.82-1.39) | 0.612 |
| Education (0.94(0.78-1.13)0.5061.09(0.73-1.61)0.674 | ||||||
| H/o Incarceration | 1.11 | (0.92-1.33) | 0.291 | 1.03 | (0.79-1.34) | 0.826 |
| Age of starting drug use | 1.01 | (1.00-1.03) | 0.064 | 1.01 | (0.99-1.03) | 0.39 |
| Route of Drug Administration (Non IV Users) | 1.05 | (0.85-1.31) | 0.635 | 1.18 | (0.88-1.58) | 0.27 |
| % Positive UDS (10) | 1.22 | (1.17-1.26) | <0.001 | 1.15 | (1.11-1.20) | <0.001 |
Table 3: Cox Regression analysis for failure to show up for treatment in OTP and BUP groups; Reference values in parenthesis; *Failure to show up for treatment for 14 consecutive days; **Failure to show up for treatment for two consecutive months.
Cox regression for BUP patients showed that for each 10% increase in positive UDS, the odds of dropping out of the program within six months increased by 15% (Hazard Ratio: 1.15 (CI: 1.11-1.20, p<0.001)).
Discussion
This report observed treatment retention with methadone and buprenorphine in a real world private practice setting and examined some of the factors that may have been responsible for the very high dropout rate in both OTP and BUP programs.
Retention in treatment at six months for OTP in this study was 36%, much lower as compared to those reported in literature and to the recent Cochrane review by Mattick et al. [11] which found 56.5% retention at similar methadone dose ranges of 50-80 mg/day as in our study. Our percent retention of 36% was similar only to that reported by Ball and Ross [12] in 1993 in new admissions to their methadone program.
In the OTP group of the present study, comparison of those who dropped out within 3 months, those who dropped out in 3 to 6 months, and those who stayed more than 6 months, revealed significant statistical differences. The differences in mean age at admission and mean years of addiction may not be clinically relevant. More clinically relevant were the differences in ethnicity, unemployment, lack of high school education, marital status, and percent of positive UDS. Failure to complete high school directly reduces opportunities for employment but the effect of Hispanic ethnicity alone on dropout from substance abuse treatment is less clear.
Hispanic ethnicity is consistent with lower income level and could negatively impact access to health care and treatment retention in the South Texas region where income is a great divider [13,14]. Being married could relate to dropout since this might create a situation leaving individuals with less money for treatment, especially during economic crises.
These factors remained to be significantly associated with failure to retain in treatment for 6 months after being adjusted for age, gender, and other covariates. The Cox regression also showed that for each 10% increase in positive UDS, the odds of dropping out of the OTP program before 6 months increased by 22% (HR: 1.22 (CI: 1.18-1.26, p<0.001)) This is consistent with literature that shows a significant association of positive urines for illicit substances with attrition from treatment [15,16].
The retention of 15.8% at six months in BUP was the lowest reported in the literature. As in the OTP, the low retention may have been also due to continuation of illicit drugs The Cox regression model in the BUP group supports this theory since each 10% increase in positive UDS, the odds of dropping out of the BUP program before 6 months increased by 15% (HR: 1.15 (CI: 1.11-1.20, p<0.001)). Like the OTP patients, the clinic may have missed the illicit drug use during non-appointment days of the month and occult use may have led to dropout [17].
Other reasons for early dropout from BUP might include the high out-of-pocket costs or the lack of psychosocial support except on the day of visit [18-20]. Review studies by Amato et al. [19] and Joe et al. [20] expressed the opinion that the outcome may be improved by contact with providers and suggested that adding any psychosocial support to maintenance treatments improves the number of participants abstinent at follow-up and thus can positively influence retention. However, most of those studies were done with methadone and not with buprenorphine. In our study, at least one LVN dispensed, observed, and communicated daily with all of the OTP patients. BUP clients, on the other hand, were not observed or contacted except on the day of visit to the clinic.
The type of opiate used, and the route of administration could also be a factor influencing the retention. Seventy seven percent (76.6%) of the patients who stayed in the BUP program for more than six months were prescription drug abusers (Table 2), suggesting a need to further evaluate that effectiveness of buprenorphine for treating IV heroin dependence.
Literature shows that living farther away from the treatment site was an environmental barrier that negatively affected treatment retention [21,22]. A separate survey at the clinic reported that many of the BUP clients lived outside the central city where the clinic was located, as opposed to the OTP clients who lived closer to the central city location. But this factor was not analyzed in this study.
Edlund et al. [23] examined dropping out of mental health treatment and found it worse in uninsured, low-income persons with negative attitudes toward substance abuse treatment. In our study, higher education and employment rates in the BUP group did not translate into better retention. Even if patients had insurance, there is evidence from Massachusetts’s experience that extending health care to many with untreated substance use disorders (as in the Affordable Care Act of 2010) might not translate to better care, since requirements for co-payments can still deter participation [24]. The high cost of treatment (including multiple physician visits, co-payments for pharmacy, and cost of non-generic medication) during the induction phase may have contributed to the high dropout rate in the initial months of the BUP program.
Mattick et al. [11] found buprenorphine, given in similar flexible doses as in this study, was less effective in retaining patients in treatment than flexible dose methadone at medium level doses equivalent to our dose levels. However, in our study, the same dose ranges of methadone and buphrenorphine had much lower retention. Other studies that compared methadone to buprenorphine, such as Kosten et al. [15], Kakko et al. [25] and Simoens et al. [26] also found retention much greater than our percentages. This may be in part because medications and no fee services may have been provided as incentives rather than patients paying out-of-pocket fee-for service. As such, these excellent research efforts may not reflect the “real world” economic issues that private treatment programs must overcome to provide substance abuse care.
The studies by Finch et al. [27] and Alford et al. [28], which were done in an office based setting with buprenorphine reported higher treatment retentions in the program compared to our study, but differed in that the study population was predominantly white and employed. Interestingly, Alford et al. [28] reported that participants of Hispanic ethnicity had significantly lower odds of treatment success.
The major strengths of this study were the large sample size, the fact that both OTP and BUP operated at the same site and employed shared professional staff, and that it had a large population of lower income non-Caucasian study participants. Although to some degree our study was a “natural control” setting in being conducted at same site and by same staff, we are unable to compare directly the two programs, since the selection of patients was not randomized, and the patients were different in ethnicity, employment, education and route of administration.
In summary, this observational study did attempt to address some of the factors contributing to the high dropout rates in opioid treatment programs. Of these, UDS positivity for illicit substances was one of the significant indicators of likelihood of dropout in both OTP and BUP. Based on these results we recommend that private practitioners treating opiate dependency in office-based settings should frequently check both regular and random UDS in an effort to try to prevent early relapse in the course of therapy.
Stark [29] have extensive reviews of methods used to enhance retention but these were not operationalized due to unavailability of finances and staff. In both BUP and OTP, the economic situation may create an environment in which financing of outpatient opiate treatment becomes financially difficult to sustain, in which case increasing support from state and local sources will be required. Practitioners treating opiate dependence must be very involved in the implementation of the Affordable Care Act of 2010, which has the potential to make positive changes for those with opiate dependence.
Conclusion
This observational study showed low retention for opiate dependence treatment at 3 and six months with both methadone (36%) and buprenorphine (15.8%) in a large Metropolitan area in South Texas with a predominant Hispanic population. Despite the clinic’s central location, flexible hours, 24/7 h availability of physicians, two dispensing nurses for shorter waiting times, 4 counseling stations, individualization of treatment, allowing balances on account in selected patients, retention was still very low.
UDS positivity for illicit substances was found to be the most important predictor for low BUP and OTP retention. Financial hardship was a factor in both groups. Operating a private office based opiate treatment program under the federal and state guidelines that includes physicians, LCDC’s, nurses, facilities for UDS may not be feasible unless significant governmental support is available.
Our study identified the need for enhanced efforts to find the factors that can improve participant retention in our current economic setting. Most of the previous research studies done to evaluate retention in treatment with methadone and buprenorphine provided medication and services for study patients free of cost in a socialized medicine environment or in an academia, so comparison with results in our setting is difficult. Further studies are required to elucidate the factors and strategies that can improve opiate treatment retention for those with limited resources.
References
- Dole VP, Nyswander M (1965) A medical treatment for diacetylmorphine (heroin) addiction: A clinical trial with methadone hydrochloride. JAMA 193: 646-650.
- Brady KT (2007) Medical treatment of opiate dependence: Expanding treatment options. Am J Psychiatry 164: 702-704.
- Fiellin DA, Rosenheck RA, Kosten TR (2001) Office-based treatment for opioid dependence: Reaching new patient populations. Am J Psychiatry 158: 1200-1204.
- Minimum Standards for Narcotic Treatment Programs. 25 Texas administrative code.
- Medication-Assisted Treatment (2018) Department of Health and Human Services. Substance Abuse and mental health services administration. 42 CFR part 8.
- American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders.
- Spruance SL, Reid JE, Grace M, Samore M (2004) Hazard ratio in clinical trials. Antimicrob Agents Chemother 48: 2787-2792.
- Simpson D, Joe G, Rowan-Szal G (1997) Drug abuse treatment retention and process effects on follow-up outcomes. Drug Alcohol Depend 47: 227-35.
- Mattick RP, Kimber J, Breen C, Davoli M (2008) Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2: CD002207.
- Ball JC, Ross A (1991) The effectiveness of methadone maintenance treatment: Patients, programs, services and outcome. Springer-Verlag, New York.
- Brown ER, Ojeda V, Wyn R, Levan R (2000) Racial and ethnic disparities in access to health insurance and health care, UCLA Center for health policy research and Henry J. Kaiser foundation.
- Fry R, Taylor P (2012) The rise of residential segregation by income. Pew research center-Social and demographic trends.
- Kosten TR, Schottenfeld R, Ziedonis D, Falcioni J (1993) Buprenorphine versus methadone maintenance for opioid dependence. J Nerv Ment Dis 181: 358-364
- Schottenfeld RS, Chawarski MC, Pakes JR, Pantalon MV, Carroll KM, et al. (2005) Methadone versus buprenorphine with contingency management or performance feedback for cocaine and opioid dependence. Am J Psychiatry 162: 340-349.
- Goldstein A, Brown BW (2003) Urine testing in methadone maintenance treatment: Applications and limitations. J Subst Abuse Treat 25: 61-63.
- Cartwright WS, Solano PL (2003) The economics of public health: Financing drug abuse treatment services. Health Policy 66: 247-260.
- Amato L, Minozzi S, Davoli M, Vecchi S (2011) Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database Syst Rev 5: CD004147.
- Joe GW, Simpson DD, Dansereau DF, Rowan-Szal GA (2001) Relationships between counselling rapport and drug abuse treatment outcomes. Psychiatr Serv 52: 1223-1229.
- Schmitt S, Phibbs C, Piette J (2003) The influence of distance on utilization of outpatient mental health aftercare following inpatient substance abuse treatment. Addict Behav 28: 1183-1192.
- Havens JR, Latkin CA, Pu M (2009) Predictors of opiate agonist treatment retention among injection drug users referred from a needle exchange program. J Subst Abuse Treat 36: 306-312.
- Edlund M, Wang P, Berglund P, Katz S, Lin E, et al. (2002) Dropping out of mental health treatment: Patterns and predictors among epidemiological survey respondents in the United States and Ontario. Am J Psychiatry 159: 845-851.
- Capoccia V, Grazier K, Toal C, Ford JII, Gustafson D (2012) Massachusetts’s experience suggests coverage alone is insufficient to increase addiction disorder treatment. Health Aff 31: 1000-1008.
- Kakko J, Grönbladh L, Svanborg, KD (2007) A stepped care strategy using buprenorphine and methadone versus conventional methadone maintenance in heroin dependence: A randomized controlled trial. Am J Psychiatry 164: 797-803.
- Simoens S, Matheson C, Bond C, Inkster K, Ludbrook A (2005) The effectiveness of community maintenance with methadone or buprenorphine for treating opiate dependence. Br J Gen Pract 55: 139-146.
- Finch JW, Kamien JB, Amass L (2007) Two-year experience with buprenorphine-naloxone (Suboxone) for maintenance treatment of opioid dependence within a private practice setting. J Addict Med 1:104-110.
- Alford, DP, LaBelle CT, Kretsch N (2011) Collaborative care of opioid-addicted patients in primary care using buprenorphine: Five-year experience. Arch Intern Med 171: 425-431.
- Stark MJ (1992) Dropping out of substance abuse treatment: A clinically oriented review. Clin Psychol Rev 12: 93-116.
Citation: Roberts BW, Perches L, Sagiraju HKR, Cech I, Herbold J (2018) “Real World” Factors Influencing Dropout from Opiate Treatment with Methadone and Buprenorphine. J Addict Res Ther 9: 360. DOI: 10.4172/2155-6105.1000360
Copyright: ©2018 Roberts BW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6687
- [From(publication date): 0-2018 - Dec 22, 2025]
- Breakdown by view type
- HTML page views: 5668
- PDF downloads: 1019