Regional Anesthetic Techniques Ability to Control Pain Effectively
Received: 26-May-2023 / Manuscript No. JPAR-23-103645 / Editor assigned: 29-May-2023 / PreQC No. JPAR-23-103645 / Reviewed: 12-Jun-2023 / QC No. JPAR-23-103645 / Revised: 17-Jun-2023 / Manuscript No. JPAR-23-103645 / Published Date: 24-Jun-2023 DOI: 10.4172/2167-0846.1000514 QI No. / JPAR-23-103645
Abstract
Adhesive capsulitis of the shoulder is characterized by a progressive painful loss of passive and active shoulder range of motion. The condition, which affects 2% to 5% of the general population, is due to chronic inflammation of the capsular sub-synovial layer leading to thickening, fibrosis, contracture, and loss of the normal axillary recess.
Keywords: Surgical intervention; Medical comorbidities; Treatment modalities; Orthopaedic surgeons; Logistic regression
Keywords
Surgical intervention; Medical comorbidities; Treatment modalities; Orthopaedic surgeons; Logistic regression
Introduction
Although commonly referred to as frozen shoulder, which encompasses the end result of a number of etiologies, adhesive capsulitis is its own distinct pathologic entity. Most patients are successfully managed with physical therapy and gentle range of motion exercises. However, surgical intervention is indicated in patients when conservative treatment fails, including physical therapy, home exercises, intra-articular injections, and oral anti-inflammatory medications, with continued pain and limitation in activities of daily living. Adhesive capsulitis most commonly affects women between the ages of 40 and 60. Systemic conditions, such as obesity, thyroid dysfunction, cardiac disease, Dupuytren contracture, breast cancer treatment, and neurologic disorders, are thought to increase the risk for developing adhesive capsulitis [1]. Furthermore, several studies have shown that the diagnosis is 2 to 4 times more common in diabetic patients than in the general population. Few studies have examined the epidemiology of adhesive capsulitis in a large urban population compared with a matched control group or determined patient factors associated with requiring surgical intervention. The purpose of this study was to evaluate patient variables significantly associated with developing adhesive capsulitis compared with a sex-matched control group without adhesive capsulitis [2]. We also sought to determine those factors associated with adhesive capsulitis patients requiring surgical intervention. Demographic information, including sex, age, body mass index, race, and ethnicity were collected for all patients. The presence of concurrent medical comorbidities was also documented and verified by review of primary care physician notes, which included diabetes mellitus, hypothyroidism, hypertension, lupus, Sjögren syndrome, dermatomyositis, polymyositis, connective tissue disorder, and rheumatoid arthritis.
Methodology
Shoulder pain status, medications, appointment history, and insurance information were collected. Patients diagnosed with adhesive capsulitis have high rates of comorbid conditions, most notably diabetes. As a result of a lack of clear pathophysiology and significantly high rates of comorbid pre-diabetes and diabetes, many authors has hypothesized that diabetes may play a central role in the pathogenesis of adhesive capsulitis [3]. Prior research points to high serum glucose increasing the rates of collagen glycosylation and crossing linking in the shoulder capsule tissue leading to inflammation, fibrosis, contracture, and significant limitations in range of motion. Controversy exists over the best treatment modalities for adhesive capsulitis, but the general agreement is that conservative methods, such as corticosteroid injections and physical therapy, are exhausted before surgery or manipulation under anaesthesia [4]. Our data indicate that age is significantly associated with whether patients were treated with surgery, with younger patients more likely to undergo surgery. This is likely attributed to younger patients having a lower perioperative risk profile, and they are less likely to adhere to the prolonged nonoperative course required due to activity demands. In contrast, patients in our group aged 70 to 79 and 80 to 89 were significantly less likely to receive surgery. Limitations of the study include those inherent to any retrospective comparative study [5]. The study relied on providers documenting correctly in the medical record. In addition, although we were able to compare patients with adhesive capsulitis to controls at our own institution, the study population may not be representative of other institutions or nationally, limiting the generalizability of this study. The mean age of adhesive capsulitis in our population falls within the previously accepted age range [6]. Obesity and diabetes were significantly associated with developing adhesive capsulitis and should be considered as modifiable patient factors. Younger, white, and workers’ compensation patients were patient variables significantly associated with receiving surgical treatment [7]. Governmentsponsored insurance status was also significantly associated with nonoperative treatment. Reasons for greater surgical intervention in these particular subgroups should be evaluated with prospective studies. Lastly, patients with workers’ compensation were 8 times as likely to receive surgery as part of their course of treatment than patients with private or commercial insurance. The disparity in reimbursement may create treatment bias for orthopaedic surgeons. In addition, patients with workers’ compensation may need to return to work sooner, thereby needing a quick fix. These patients may be unwilling to exhaust conservative treatment before progressing to more invasive treatment options [8].
Results
Adhesive capsulitis is characterized by a gradual, painful loss of shoulder motion. This study evaluated patient variables significantly associated with developing adhesive capsulitis compared with a sex-matched control group without adhesive capsulitis [9]. We also sought to determine those factors associated with adhesive capsulitis patients requiring surgical intervention. All patients presenting to our hospital with adhesive capsulitis between 2004 and 2014 were identified. Demographic characteristics were collected, and a sexmatched control group was randomly generated from the electronic medical record and used for comparison [10]. Patients who underwent surgical intervention for adhesive capsulitis were also identified, and factors associated with surgical intervention were identified with logistic regression analysis. There is a wide variety of patients who present for shoulder surgery, ranging from the fit, robust patient with a sports injury requiring a stabilization procedure, to the frail, elderly rheumatoid patient requiring joint decompression or arthroplasty [11]. Recent surgical advances have resulted in the development of minimal access arthroscopic procedures with resulting improvements in speed of convalescence. However, the management of severe postoperative pain remains a major challenge for many anaesthetists. Regional anaesthetic techniques have the ability to control pain effectively both at rest and on movement, reduce muscle spasm, and allow earlier mobilization and co-operation with physiotherapy [12]. Therefore, these techniques have the potential to improve both patient recovery and outcome after both open and arthroscopic surgeries. Management of these patients requires thorough preoperative assessment, careful intraoperative management, and appropriate use of regional anaesthetic techniques to provide adequate dynamic pain relief in the initial postoperative period. The most commonly performed open surgical procedures include repairs for instability, acromioplasty, subacromial decompression, fracture fixation, and hemi- and total shoulder arthroplasty [13].
Discussion
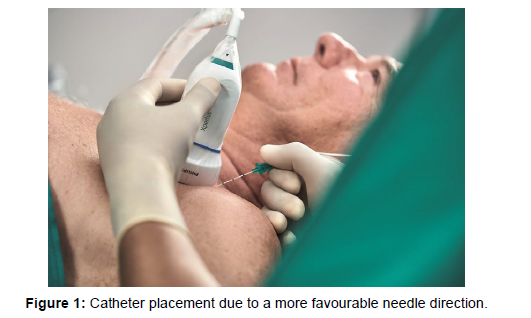
The main surgical approach is through an anterior incision starting just lateral to the tip of the coracoid, running down into the axillary crease. A more extended approach is used for shoulder arthroplasty, when the incision is continued past the axilla to the deltoid insertion [14]. A posterior approach is rarely used. In recent years, shoulder arthroscopy has been increasingly popular both as a diagnostic tool and for surgical procedures, including acromioplasty, stabilization of the gleno-humeral joint, arthroplasty of the acromioclavicular joint, rotator cuff repairs, and chondroplasties. The patient is either in the deck chair or lateral position, depending on surgical preference [15]. A full preoperative anaesthetic assessment is essential before choosing the most appropriate anaesthetic technique. Although many of the patients are fit and healthy, another group exists in whom coexisting medical problems have not only contributed to the development of shoulder ailments but also make anaesthetizing the patient for surgery challenging. Besides patient factors influencing anaesthetic technique, surgical factors also need to be considered [16]. Minor surgical procedures can usually be carried out with regional anaesthesia alone, whereas, with more major surgery of longer duration, a combination of regional and general anaesthesia may be more appropriate. Patient selection and psychological preparation are essential for awake shoulder surgery, as aspects of the procedure are often less well tolerated even with excellent anaesthesia due to the proximity of surgical instruments to the face and head. Other approaches such as the Meier modification may facilitate catheter placement due to a more favourable needle direction as shown in (Figure 1). The needle insertion site is a further 2 cm cranially, with the needle directed along the inter-scalene groove towards the junction of the middle and lateral third of the ipsilateral clavicle, caudad and slightly dorsal to the horizontal [17]. Initial block assessment should be made 10 min after insertion; earlier evaluation when the block is unlikely to be working will only endanger patient confidence, which is an essential part of any regional technique. The three components of the block should be tested, motor by asking the patient to abduct and flex the arm from the shoulder, cutaneous sensation to cold over the relevant dermatomes, and, joint sensation by demonstrating the loss of pain during passive movement. Cutaneous anaesthesia alone is not a reliable indicator of block success. After the insertion of the block and the demonstration of its efficacy, general anaesthesia is induced if required as shown in (Figure 2). Alternatively, the patient is sedated, usually with midazolam or a target-controlled propofol infusion as appropriate [18]. The judicious use of an opioid may be useful to help with generalized discomfort during the more prolonged cases. We believe that the inter-scalene block should only be performed before the induction of general anaesthesia, as it is associated with potentially serious complications. Accidental injection of local anaesthetic can be more easily diagnosed in an awake patient and we advise, following aspiration, injecting only 1 –2 ml of local anaesthetic to allow detection of inadvertent injection into the vertebral artery, before continuing with the slow injection of 5 ml increments to a total volume of 25–30 ml. Other major complications include subarachnoid/epidural injection, stellate ganglion block, and pneumothorax. Benumof described four cases in which inter-scalene block performed after induction of anaesthesia led to total spinal anaesthesia and subsequently to extensive permanent cervical spinal cord damage. Magnetic resonance scans showed syrinx or cavity formation in the cervical spinal cord as a result of direct injection of local anaesthetic solution into the spinal cord. The phrenic nerve, with associated ipsilateral hemi-diaphragmatic paresis, is nearly always blocked; therefore, bilateral inter-scalene blocks should never be performed. It is also important to be cautious when performing this block on patients with co-existing respiratory disease as it may cause respiratory embarrassment or failure, particularly in the supine patient. A combination of COPD with a high BMI is particularly problematic, although most patients will tolerate a unilateral block if maintained in the deck chair or seated positions. Each case should be assessed on an individual basis and an alternative analgesic strategy sought if there is significant concern. Choice of local anaesthetic agent is usually determined by the duration and magnitude of surgery. Lidocaine is appropriate for short procedures and for those patients with pre-existing respiratory compromise in whom shorter block duration is desirable. However, for most surgery, a long-acting agent such as levobupivacaine or ropivacaine is more appropriate given the significant postoperative discomfort involved. A perineural catheter may be inserted while performing the interscalene block, allowing analgesia to be extended longer into the postoperative period. If a catheter is to be inserted, the initial block should be performed using one of the available proprietary catheter kits, and the catheter inserted to a depth of approximately 2–3 cm. Once the catheter is secured to the skin with an occlusive dressing, this should be covered with gauze to prevent the surgical drapes from sticking to the dressing, with the catheter then being inadvertently dislodged or cut at the end of the procedure. Alternatively, the catheter can be tunnelled medially. This has three advantages: it improves catheter security in the perioperative period; it lessens the likelihood of infection; and the more medial placement removes the catheter further from the surgical field. The brachial plexus is a relatively superficial structure in the inter-scalene region, and other techniques can be used to aid location of the plexus. These include ultrasound guided techniques and percutaneous electrode guidance of the block needle. Ultrasound guided block placement allows the plexus to be visualized at different levels in the neck. The path of the needle as it approaches the plexus can be visualized, allowing vital structures to be avoided, potentially reducing the incidence of complications. Using ultrasound as an aid to block placement is an exciting development; the technique was described in a recent review article. Percutaneous electrode guidance6 uses a transcutaneous stimulating probe with the nerve first located by eliciting the desired motor response at a current of 5 mA at an increased pulse width of 1 ms. The needle insertion point can then be mapped on the skin and the block needle introduced. Intraoperative management Adequate access should be obtained as blood loss can be significant, especially during arthroplasty. The deck chair position is used for most anterior approaches to the shoulder joint. The trunk and head are raised to an angle of approximately 20– 308 to the horizontal to reduce venous pressure at the shoulder level; raising the legs will help maintain venous return and cardiac output. The legs should be flexed at the knees with a pillow to avoid discomfort from over-stretching of the hamstrings. Pressure points, especially the heels, must be carefully padded, as must the ulnar nerve at the elbow. The head and neck should be secure while care should be taken throughout the procedure to ensure that excessive stretching of the brachial plexus does not occur as a result of the excessive surgical traction. The eyes should be taped and padded in the anaesthetized patient as they are in close proximity to the surgical site and instruments. Performing surgery under peripheral nerve block alone allows the patient to assist with comfortable positioning on the operating table.
Conclusion
However, shoulder surgery is often prolonged and patients may find parts of the procedure unpleasant, even with sedation. A warm-air blanket system should be used to maintain patient temperature.
Acknowledgement
None
Conflict of Interest
None
References
- Świeboda P, Filip R, Prystupa A, Drozd M (2013) Assessment of pain: types, mechanism and treatment. Ann Agric Environ Med EU 1:2-7.
- Nadler SF, Weingand K, Kruse RJ (2004) The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain Physician US 7:395-399.
- Trout KK (2004) The neuromatrix theory of pain: implications for selected non-pharmacologic methods of pain relief for labor. J Midwifery Wom Heal US 49:482-488.
- Cohen SP, Mao J (2014) Neuropathic pain: mechanisms and their clinical implications. BMJ UK 348:1-6.
- Mello RD, Dickenson AH (2008) Spinal cord mechanisms of pain. BJA US 101:8-16.
- Kahn LH (2006) Confronting zoonoses, linking human and veterinary medicine. Emerg Infect Dis US 12:556-561.
- Bidaisee S, Macpherson CNL (2014) Zoonoses and one health: a review of the literature. J Parasitol 2014:1-8.
- Cooper GS, Parks CG (2004) Occupational and environmental exposures as risk factors for systemic lupus erythematosus. Curr Rheumatol Rep EU 6:367-374.
- Parks CG, Santos ASE, Barbhaiya M, Costenbader KH (2017) Understanding the role of environmental factors in the development of systemic lupus erythematosus. Best Pract Res Clin Rheumatol EU 31:306-320.
- M Barbhaiya, KH Costenbader (2016) Environmental exposures and the development of systemic lupus erythematosus. Curr Opin Rheumatol US 28:497-505.
- Gergianaki I, Bortoluzzi A, Bertsias G (2018) Update on the epidemiology, risk factors, and disease outcomes of systemic lupus erythematosus. Best Pract Res Clin Rheumatol EU 32:188-205.
- Cunningham AA, Daszak P, Wood JLN (2017) One Health, emerging infectious diseases and wildlife: two decades of progress? Phil Trans UK 372:1-8.
- Sue LJ (2004) Zoonotic poxvirus infections in humans. Curr Opin Infect Dis MN 17:81-90.
- Pisarski K (2019) The global burden of disease of zoonotic parasitic diseases: top 5 contenders for priority consideration. Trop Med Infect Dis EU 4:1-44.
- Birnesser H, Oberbaum M, Klein P, Weiser M (2004) The Homeopathic Preparation Traumeel® S Compared With NSAIDs For Symptomatic Treatment Of Epicondylitis. J Musculoskelet Res EU 8:119-128.
- Ozgoli G, Goli M, Moattar F (2009) Comparison of effects of ginger, mefenamic acid, and ibuprofen on pain in women with primary dysmenorrhea. J Altern Complement Med US 15:129-132.
- Świeboda P, Filip R, Prystupa A, Drozd M (2013) Assessment of pain: types, mechanism and treatment. Ann Agric Environ Med EU 1:2-7.
- Nadler SF, Weingand K, Kruse RJ (2004) The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain Physician US 7:395-399.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed At , Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Ahasan R (2023) Regional Anaesthetic Techniques Ability to ControlPain Effectively. J Pain Relief 12: 514. DOI: 10.4172/2167-0846.1000514
Copyright: © 2023 Ahasan R. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1556
- [From(publication date): 0-2023 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 1221
- PDF downloads: 335