Subtotal Colectomy is a Safe and Effective Single Stage Surgery for Acute Left Colonic Malignant Obstruction with Acceptable Functional
Received: 13-Feb-2023 / Manuscript No. JGDS-23-89318 / Editor assigned: 15-Feb-2023 / PreQC No. JGDS-23-89318 (PQ) / Reviewed: 01-Mar-2023 / QC No. JGDS-23-89318 / Revised: 03-May-2023 / Manuscript No. JGDS-23-89318 (R) / Published Date: 10-May-2023
Abstract
Purpose: Primary resection and anastomosis for malignant acute obstruction of left colon offers a single stage surgical option without a stoma. Our aim was to determine the outcome of subtotal colectomy in acutely obstructed left colonic cancer.
Methods: A retrospective review of all patients who underwent subtotal colectomy for acutely obstructed left colon cancer over a 10 years period was performed. All procedures were performed by specialist colorectal surgeons. The primary objective is to analyse the anastomotic leak rate and the functional outcome measured in terms of frequency of bowel movements.
Results: A total of 72 patients underwent sub-total colectomy among which one patient had primary peritoneal carcinomatosis causing obstruction of the sigmoid colon. Male predominance was noted (61.1%). The tumours predominantly involved the distal transverse colon (23/71) and proximal sigmoid colon (22/71), followed by descending colon (16/71) and splenic flexure (11/71). All the patients had locally advanced T3 and T4 tumours leading to colonic obstruction. Eight patients had synchronous adenomatous polyps among which 3 of them had high grade dysplasia. Seven patients had synchronous non-obstructing malignant colonic lesions. The average postoperative stay in hospital was 6.5 days. Only one patient had an anastomotic leak (1.4%). The average frequency of bowel movements per day was 2.83 at 6 months after surgery. There was no mortality during the six month follow up.
Conclusion: Sub-total colectomy is a safe, effective and well tolerated single stage procedure with acceptable functional outcome with added benefits of removing synchronous polyps and cancers.
Keywords
Colon cancer; Acute colonic obstruction; Colectomy; Single stage surgery; Synchronous polyps
Introduction
Seven to twenty nine percent of patients with colorectal cancer present with an acute LBO of which >75% are distal to the splenic flexure [1]. International guidelines offer limited and contrasting recommendations on the management of left colonic obstruction [2]. Proximal stoma, followed by a segmental resection and subsequent stoma reversal or ‘3 stage procedure’ has historically been employed for obstructing cancers to reduce morbidity [3]. Several studies have since shown no benefit of this approach for colonic obstruction [4,5]. Primary resection with end colostomy (Hartmann’s operation) is considered the safest option [6,7]. End colostomy without resection cannot be performed in obstructed patients due to risk of stump dehiscence secondary to closed loop obstruction. Loop colostomies can be associated with prolapse and bypass into the distal limb, especially the loop transverse colostomy [8]. Defunctioning ileostomy has the disadvantage of leaving behind a dilated fecal filled colon, especially in the presence of a competent ileocaecal valve [9]. For distal colonic obstruction, the Hartmann’s procedure which involves a rectosigmoidectomy, closure of the rectal stump and formation of an end stoma, is the most frequently chosen surgical option [10]. Only 30%-40% of patients ultimately undergo a reversal procedure [11].
Colorectal Self Expanding Metal Stent (SEMS) can be a good option for the treatment of acute malignant colonic obstruction as a bridge to surgery, allowing time for a preoperative evaluation and for the patient’s page 3/13 medical condition to improve. One study has reported a higher rate of local recurrence in the SEMS group [12]. The technical failure rate was higher for descending and more proximal colonic stenting than rectosigmoid stenting [13,14]. Failed relief can occur due to malpositioning or lack of expansion of stent. It can also be associated with complications such as perforation, stent migration and stent reobstruction. Some reports had concluded that colonic stent followed by elective surgery is more effective and cost efficient than emergency surgery [15,16]. However, the stenting group was compared with staged surgery in above reports. Stenting prior to surgery can also significantly increase the costs of treatment when compared with single stage surgery, especially in countries where patient has to pay for the treatment.
Resection and primary anastomosis without stoma is increasingly being considered as a preferred single stage procedure in left colonic obstruction. The choice is between a sub-total colectomy and segmental colectomy. While segmental colectomy has the advantage of preserving majority of colon, it has the disadvantage of having to deal with a dilated fecally loaded colon with on table lavage or manual evacuation. While intra operative colonic irrigation has the advantage of performing anastomosis on a relatively clean bowel, it can be associated with increased operative time, risk of spillage and contamination. The edematous and dilated proximal colon is likely to be associated with increased risk of anastomotic leak in segmental colectomy and primary anastomosis.
Diarrhoea has been reported as the main complaint in patients undergoing total/subtotal colectomy leading to poor functional outcome [17,18]. A total colectomy and ileorectal anastomosis for recto sigmoid tumours is more likely to be associated with troubling diarrhoea due to complete absence of colon and part of rectum. Hence our preference for rectosigmoid tumours will be stenting followed by elective surgery. However, subtotal colectomy with ileosigmoid anastomosis for tumours involving splenic flexure, descending colon and proximal sigmoid colon can be associated with a much better functional outcome due to partly preserved sigmoid colon. Ileosigmoid anastomosis after sub-total colectomy has been shown to be associated with good bowel function and quality of life [19]. A subtotal colectomy can also remove synchronous proximal neoplasms and polyps and thereby reduce metachronous tumours in future [20]. We performed a retrospective study to analyse the outcome of patients undergoing sub-total colectomy and primary ileo-colic anastomosis in our institution.
Materials and Methods
A retrospective review of all patients who underwent subtotal colectomy for acutely obstructed left colon cancer over a 10 years period was performed. Tumours involving the distal transverse colon, splenic flexure, descending colon and proximal sigmoid colon were included. Tumours involving rectosigmoid junction and rectum were excluded from this study. All procedures were performed by specialist colorectal surgeons. Discharge summaries, histopathology reports and outpatient review notes were used for data collection. Data collection will include duration of surgery, per-operative complications, postoperative complications and duration of hospital stay. Our primary objective is to analyse the anastomotic leak rate and the functional outcome measured in terms of frequency of bowel movements at 6 months.
Definition
Segmental colectomy is defined as resection in which one main artery is divided, while hemicolectomy involves two main arteries. Subtotal colectomy is performed if three main colic arteries are divided, while total colectomy involves four main arteries. In our series of sub-total colectomy, ileocolic, middle colic and left colic arteries were divided with division of additional sigmoid arteries based on tumour location. Superior rectal artery was preserved in all patients.
Surgical technique
Under general anaesthesia abdomen is examined and based on availability of intraperitoneal space a laparoscope was inserted and examined. If there was adequate space for surgery to proceed laparoscopically, then a laparoscopic assisted surgery was performed. However, if there was no adequate space for laparoscopic mobilisation, it was converted to midline laparotomy.
The tumour location is confirmed during surgery and the status of caecum is examined. Partial decompression was done by a large bowel enterotomy with a protecting purse string suture if there was risk of rupture during mobilisation. Lateral mobilisation is done to release the sigmoid colon and descending colon with preservation of ureter and gonadal vessels. Without ligating the main trunk of IMA, the left colic and sigmoid vessels are ligated as necessary. The superior rectal artery is also preserved in all patients. Splenic flexure mobilisation is performed. The right colon is then mobilised in the lateral to medial fashion protecting the duodenum. The ileocolic, right colic (if present) and right and left branches of middle colic vessels are ligated and divided. The ileum is divided 5 cm proximal to ileocecal junction and the distal division was done based on the location of tumour and vascularity, providing at least 5 cm distal margin. A T-shaped side to side stapled ileo descending or ileo sigmoid anastomosis was performed using linear cutting staplers. In cases where laparoscopic mobilisation was performed, the bowel ends were delivered out through a small midline incision to complete the ileo-colic anastomosis.
Results
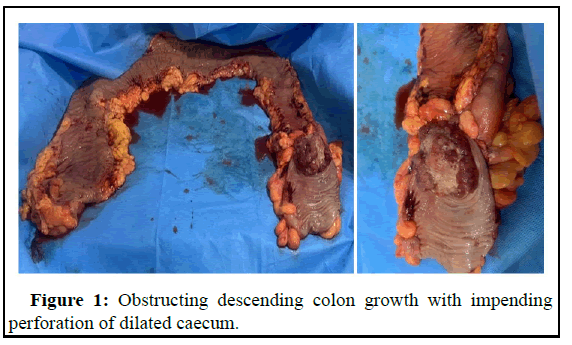
A total of 72 patients who underwent sub-total colectomy for acute left colonic malignant obstruction were examined. While one patient had a primary peritoneal carcinomatosis causing obstruction of the sigmoid colon, all other patients had primary colonic cancer with obstruction. Male predominance was noted (61.1%) similar to the incidence of colorectal cancers in general population. The tumours predominantly involved the distal transverse colon and proximal sigmoid colon, followed by descending colon and splenic flexure. All the patients had locally advanced T3 and T4 tumours leading to colonic obstruction (Figure 1). Positive malignant lymph nodes (56.3%) were more common than finding negative lymph nodes (43.7%). Majority of the tumours were moderately differentiated and non-mucinous tumours. The frequency of perineural invasion (23.9%) in the resected tumours was more common than lympho vascular invasion (12.7%). All the clinicopathological characteristics are summarised in Table 1.
| Variables | Characteristics |
|---|---|
| Total patients | n=72 |
| Mean age | 60 years (range 26-85 years) |
| Gender | Male-44, female-28 |
| Site of tumour | Distal transverse colon-23 Splenic flexure-11 Descending colon-16 sigmoid colon-22 |
| T status (n=71) | T1-0 |
| T2-0 | |
| T3-42 | |
| T4-29 | |
| N status (n=71) | N0-31 |
| N1-23 | |
| N2-17 | |
| M status (n=72) | M0-68 |
| M1-4 | |
| Grade | Well differentiated-1 |
| Moderately differentiated-63 | |
| Poorly differentiated-7 | |
| Mucinous type (n=71) | Mucinous-10 Non-mucinous-61 |
| Lymphovascular invasion (n=71) | Present-9 |
| Absent-62 | |
| Perineural invasion (n=71) | Present-17 |
| Absent-54 |
Table 1: Clinicopathological characteristics.
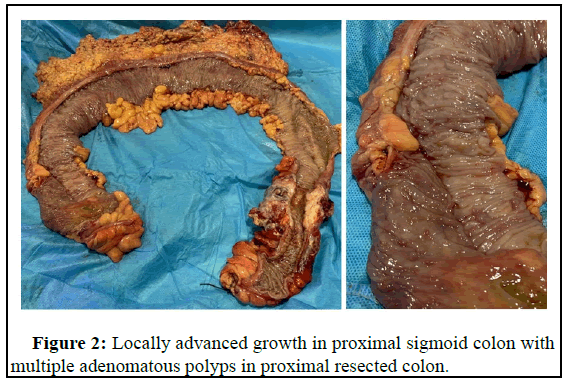
A total of 8 patients had synchronous adenomatous polyps in the resected proximal colon among which 3 of them had adenomatous polyps with high grade dysplasia (Figure 2). Seven patients had synchronous non-obstructing malignant colonic lesions in the proximal resected colon. While large majority of surgeries were performed with open laparotomy (88.9%), we were able to perform laparoscopic assisted surgery in a minority (11.1%) of patients. While the average duration of surgery was 169.4 min, the duration of surgery was much higher when performed laparoscopically (222.9 min) than open surgery (162.8 min). The average post-operative stay in hospital following sub-total colectomy was 6.5 days. 25% of the patients developed a minor wound infection which settled with antibiotics and regular dressings. In our study only one patient had an anastomotic leak (1.4%) which was a patient with localised perforation for which an end ileostomy was performed subsequently. The average frequency of bowel movements per day was 2.83 at 6 months after surgery. There was no mortality during the six month follow up. The outcome variables are summarised in Table 2.
| Variable | Outcome | |
|---|---|---|
| Synchronous polyps identified | n=8 | HGD=3 |
| LGD=5 | ||
| Synchronous cancer identified | n=7 | Caecum-1 |
| Ascending colon-1 | ||
| Caecum and ascending colon-1 | ||
| Hepatic flexure-1 | ||
| Transverse colon-1 | ||
| Descending colon-2 | ||
| Type of surgery | Open-64 | |
| Laparoscopic-8 | ||
| Surgery duration (min) | Mean-169.44 (range 109-268) | |
| Time to discharge after surgery (days) | Mean-6.5 (range 4-11) | |
| Complications | Anastomotic leak -1 | |
| Wound infection-18 | ||
| Bowel frequency at 6 months | Mean-2.83 (range 1-6) | |
Table 2: Operative, immediate post-operative and short term outcomes after sub-total colectomy for acute left colonic malignant obstruction.
Discussion
This is the largest series of single stage sub-total colectomy and ileo-colic anastomosis for acutely obstructing left colonic cancer. While we excluded the patients undergoing total colectomy, some of the previous studies had reported the combined outcome of total and subtotal colectomy. In general the colon is considered dilated if it is over 6 cm in diameter, with the caecum having an upper limit of 9 cm. Hence caecal dilatation of 9 cm or higher on CT were considered to have impending rupture and planned for a sub-total colectomy. Some patients in whom dilatation on CT was less than 9 cm but per operatively found to have impending rupture with significant serosal tears on the caecum were decided to proceed with sub-total colectomy. With this strategy we report a series of sub-total colectomy (n=72) for left colonic malignant obstruction. In patients with partial colonic obstruction we preferred to perform a segmental colectomy. In this study we have not compared segmental colectomy with sub-total colectomy as our criteria for patient selection will not allow comparison of the two groups. Hence, we planned to analyse the outcome of sub-total colectomy alone in this study.
Only one patient in our study ended up having a stoma (ileostomy) due to anastomotic leak. All the remaining patients did not have the need for stoma during the follow up period. A staged surgery for malignant left colonic obstruction has the disadvantage of long duration of treatment with associated increasing costs, particularly in the absence of a national healthcare system. An obstructing cancer is likely to be locally advanced and hence the need for adjuvant therapy. The need for adjuvant therapy may delay the stomal reversal thereby reducing the quality of life of patients. Disease progression in the postoperative period may mean that the patients would be stuck with colostomy for the rest of their lives. The underlying general condition does not permit colostomy reversal in up to 45% of the patients.
Surgical strategies such as intraoperative colonic lavage and preoperative placement of SEMS have been developed to promote primary resection of cancer and anastomosis.
All the patients had sub-total colectomy and primary anastomosis except one patient who along with obstruction had perforation and abdominal sepsis. Only one patient had anastomotic leak (1.4%) among the remaining patients (n=71) who had ileo-colic anastomosis. The SCOTIA trial (segmental 5%, sub-total colectomy 9%) did not report any significant difference in anastomotic leak rates. However, we consider the leak rates to be high in both the groups. However, other reports have shown significantly less leak rate in sub-total colectomy. Kaser, et al., had reported an anastomotic leak rate of 20% in patients with segmental colectomy and primary anastomosis for malignant acute left colonic obstruction. The low anastomotic leak rate in sub-total colectomy with ileosigmoid anastomosis could have been due to the fact that a relatively healthy and non-dilated ileum is anastomosed to the healthy colon distal to obstruction. Further, the column of faeces is completely removed along with the colon which reduces the risk further. Considering that in sub-total colectomy we leave at least the last 5 cm-10 cm of sigmoid colon, we do not perform ligation of IMA. Rather we do ligation of the left colic and selected sigmoid arterial branches similar to segmental colectomy without compromising the oncological clearance. Our technique of preserving blood supply to the distal colon and rectum has also contributed to the low anastomotic leak rates.
As the entire segment of dilated, edematous and potentially ischemic segment of colon is removed, the risk of wound and peritoneal contamination is less compared to on table lavage. Whenever there was a risk of rupture of the dilated bowel, a partial decompression was done by a large bowel enterotomy with a protecting purse string suture in order to avoid peritoneal contamination. The operating time can be comparable to segmental colectomy with on table lavage without the need for additional equipment. The avoidance of peritoneal contamination during surgery could also have contributed to our very low anastomotic leak rate.
Eight patients were found to have synchronous adenomatous polyps in the resected colon, which included polyps with high grade dysplasia in three patients. Seven patients (9.9%) in the study group were found to have synchronous proximal bowel cancer. Various studies have reported the incidence of synchronous colonic cancer as 2%-11% with an even higher incidence in the presence of malignant colonic obstruction. In patients presenting with acute colonic obstruction, detection of synchronous cancer and polyps is impossible as a colonoscope could not be passed beyond the site of obstruction. A multidetector CT scan also cannot reliably diagnose a synchronous early cancer due to the faecal loading.
In our study the average bowel frequency at 6 months has been shown to be 2.83 (range 1-6) which we consider to be an acceptable outcome. Diarhhoea has been reported to be one of the main reasons against performing total/subtotal colectomy in acute left colonic malignant obstruction. This can be true in total colectomy with ileorectal anastomosis due to which we prefer to do stenting followed by elective surgery. Bowel frequency and diarrhoea have been reported to be less when about 10 cm of the colon is left in situ.
While the average bowel frequency following sub-total colectomy tends to be higher than that of segmental colectomy, we have shown that bowel frequency is within acceptable limits. In order to put things in perspective, we have to consider the benefits of single stage surgery, avoidance of stoma, very low anastomotic leak rates and simultaneous resection of undetectable synchronous polyps and cancers.
Conclusion
Sub-total colectomy is a safe procedure with very low anastomotic leak rate. It is an effective procedure with early return of bowel function. It is a well-tolerated single stage procedure without the need for a stoma which drastically improves the quality of life of patients. We have shown that it has an acceptable functional outcome in terms of bowel frequency when performed in selected patients with 5 cm-10 cm of residual sigmoid colon. It is associated with reduced costs for the patient as it is a single stage procedure with minimal complications. It has the added benefits of removing synchronous polyps and cancers at the same stage.
Declarations
• The authors did not receive support from any organization for the submitted work.
• The authors have no competing interests to declare that are relevant to the content of this article.
• The study was approved by the institutional review board-GEM research ethics committee.
Acknowledgements
Greeshma for help with data collection.
Author’s Contributions
Concept and design: Senthil Kumar Ganapathi, Rajapandian Subbiah, Praveenraj Palanivelu.
Tables and figures: Harish Kakkilaya, Sathiyamoorthy Rudramurthy.
Data collection and analysis: Senthil Kumar Ganapathi, Aravinth Subramanium.
First draft of manuscript: Senthil Kumar Ganapathi, Palanivelu Chinnusamy.
All authors read and approved the final manuscript.
References
- Dauphine CE (2002) Placement of self-expanding metal stents for acute malignant large-bowel obstruction: a collective review. Ann Surg Oncol 9: 574-579.
[Crossref] [Google Scholar] [PubMed]
- Webster PJ, Aldoori J, Burke DA (2019) Optimal management of malignant left sided large bowel obstruction: Do international guidelines agree?. World J Emerg Surg 14: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Ansaloni L (2010) Guidelines in the management of obstructing cancer of the left colon: Consensus conference of the World Society of Emergency Surgery (WSES) and Peritoneum and Surgery (PnS) society. World J Emerg Surg 5: 29.
[Crossref] [Google Scholar] [PubMed]
- Kronborg O (1995) Acute obstruction from tumour in the left colon without spread. A randomized trial of emergency colostomy versus resection. Int J Colorectal Dis 10: 1-5.
[Crossref] [Google Scholar] [PubMed]
- de Salvo GL (2004) Curative surgery for obstruction from primary left colorectal carcinoma: Primary or staged resection?. Cochrane Database Syst Rev 2004.
[Crossref] [Google Scholar] [PubMed]
- Meyer F (2004) Emergency operation in carcinomas of the left colon: Value of Hartmann's procedure. Tech Coloproctol 8: 226-229.
[Crossref] [Google Scholar] [PubMed]
- Desai DC (1998) The utility of the Hartmann procedure. Am J Surg 175: 152-154.
[Crossref] [Google Scholar] [PubMed]
- Du R (2021) Postoperative morbidity and mortality after anterior resection with preventive diverting loop ileostomy versus loop colostomy for rectal cancer: A updated systematic review and meta-analysis. Eur J Surg Oncol 47: 1514-1525.
[Crossref] [Google Scholar] [PubMed]
- Malik TA, Lee MJ, Harikrishnan AB (2018) The incidence of stoma related morbidity-a systematic review of randomised controlled trials. Ann Coll Surg Engl 100: 501-508.
[Crossref] [Google Scholar] [PubMed]
- Sartelli M (2020) Update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg 15: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Frago R (2014) Current management of acute malignant large bowel obstruction: A systematic review. Am J Surg 207: 127-138.
[Crossref] [Google Scholar] [PubMed]
- Gorissen KJ (2013) Local recurrence after stenting for obstructing left-sided colonic cancer. Br J Surg 100: 1805-1809.
[Crossref] [Google Scholar] [PubMed]
- Khot UP (2002) Systematic review of the efficacy and safety of colorectal stents. Br J Surg 89: 1096-1102.
[Crossref] [Google Scholar] [PubMed]
- Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M (2004) Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 99: 2051-2057.
[Crossref] [Google Scholar] [PubMed]
- Targownik LE (2004) Colonic stent vs. emergency surgery for management of acute left sided malignant colonic obstruction: A decision analysis. Gastrointest Endosc 60: 865-874.
[Crossref] [Google Scholar] [PubMed]
- Singh H (2006) The cost effectiveness of colonic stenting as a bridge to curative surgery in patients with acute left sided malignant colonic obstruction: A Canadian perspective. Can J Gastroenterol 20: 779-785.
[Crossref] [Google Scholar] [PubMed]
- Hennekinne-Mucci S (2006) Emergency subtotal/total colectomy in the management of obstructed left colon carcinoma. Int J Colorectal Dis 21: 538-541.
[Crossref] [Google Scholar] [PubMed]
- Manceau G (2013) Elective subtotal colectomy with ileosigmoid anastomosis for colon cancer preserves bowel function and quality of life. Colorectal Dis 15: 1078-1085.
[Crossref] [Google Scholar] [PubMed]
- Ghazal AH (2013) Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg 17: 1123-1129.
[Crossref] [Google Scholar] [PubMed]
- Pearce NW, Scott SD, Karran SJ (1992) Timing and method of reversal of Hartmann's procedure. Br J Surg 79: 839-841.
[Crossref] [Google Scholar] [PubMed]
Citation: Ganapathi SK, Kakkilaya H, Rudramurthy S, Subbiah R, Subramanium A, et al. (2023) Subtotal Colectomy is a Safe and Effective Single Stage Surgery for Acute Left Colonic Malignant Obstruction with Acceptable Functional Outcome. J Gastrointest Dig Syst 13: 737.
Copyright: © 2023 Ganapathi SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2384
- [From(publication date): 0-2023 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 2017
- PDF downloads: 367