The Baby Bump and Malignant Lump: A Case Report of a Pregnant Patient with a Pelvic Sarcoma
Received: 15-May-2020 / Accepted Date: 05-Jun-2020 / Published Date: 15-Jun-2020 DOI: 10.4172/2472-016X.1000135
Abstract
Purpose: The occurrence of a malignancy during the course of pregnancy is uncommon but devastating. Due to the relative rarity of the condition, guidelines for management are largely based from small retrospective studies or case series with limited follow-up. With this case, we aim to discuss the options of management and rationalize the decisions in which the course of treatment of this patient has proceeded.
Methods: We describe the clinical presentation of the patient as well as the radiological findings, diagnostic tests, and management during the course of the disease.
Results: A 26-year old G2P1 (1001) Filipino female presented initially with a limp and gradual enlargement of a mass on the right hip while with a single intrauterine pregnancy of 8-9 weeks age of gestation. As the growth the mass continued, patient sought consult at our institution at 22 weeks gestation and was presented with options for management. Patient opted for conservative treatment with chemotherapy over hemipelvectomy. The neonate was eventually delivered at 35 weeks of gestation and demise of the patient ensued 2 months postpartum.
Conclusion: The treatment of malignancy in the pregnant patient should be individualized and largely dependent on the decision of the mother once full disclosure of all options of management, possible risks, and prognosis have been discussed.
Keywords: Sarcoma; Cancer; Pregnant
Introduction
Cancer in pregnancy is defined as a cancer diagnosed from the first day of childbearing to one year post-partum, estimated to occur 1 in every 1,000 women [1,2]. Due to the relative rarity of the condition, guidelines for management are largely based from small retrospective studies or case series with limited follow-up [2-4].
The general rule in the management of pregnant women with cancer is that treatment should not differ between pregnant and nonpregnant patients [1]. The main concern is that both diagnostics and treatment in the form of surgery, chemotherapy, or radiotherapy all have consequences on the developing fetus, which have to be considered. Eventually, once full disclosure of all options of management with its possible risks and benefits has been provided, the course of treatment is dependent on the decision of the mother.
Case Presentation
Here, we present a rare case of a pelvic soft tissue sarcoma in a mother with a pregnancy of 22 weeks gestation and the process by which her diagnosis and treatment was established.
History and physical examination
A 26-year old G2P1 (1001) Filipino presented initially with a limp while at 8-9 weeks age of gestation (AOG). By 18 weeks AOG, there was note of an enlarging mass on the right hip associated with difficulty ambulating, loss of appetite and weight. This prompted consult where imaging revealed a right hip mass. Patient consequently underwent incisional biopsy which revealed histiocytic sarcoma.
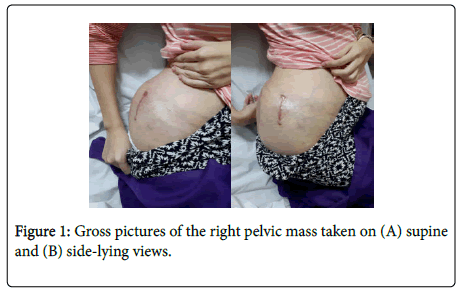
Upon presentation at our institution at 22 weeks AOG, patient was stretcher- borne with a 10 × 15 cm firm and non-tender, round mass on the right pelvic area (Figure 1). Patient was unable to tolerate range of motion of the right hip due to pain. Pulses were full and no palsy was documented.
Imaging
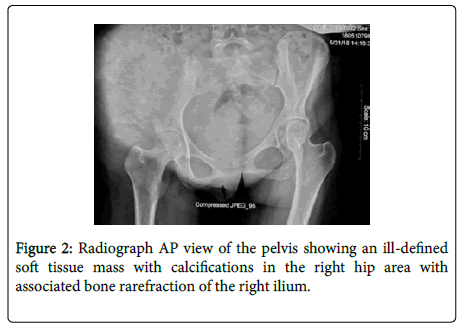
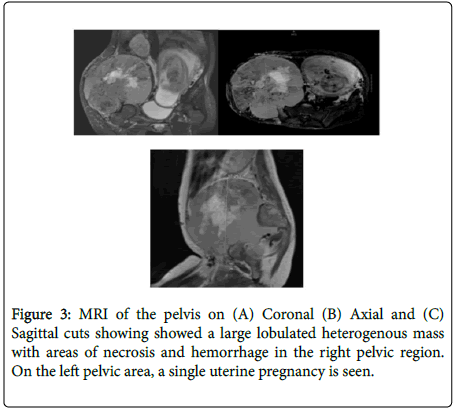
An x-ray of the pelvis initially showed an ill-defined soft tissue mass with calcifications in the right hip area and bone rarefraction of the right ilium (Figure 2). An MRI done showed a large lobulated heterogenous mass with areas of necrosis and hemorrhage and osseous destruction centering on the right iliac bone measuring 18.6 × 18.8 × 17.3 cm (Figure 3).
Course of present illness
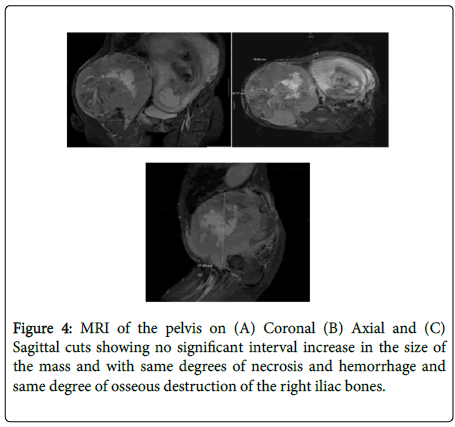
All options for management were discussed with the patient, including hemipelvectomy however, patient opted conservative management with chemotherapy and to continue with the pregnancy until delivery of her baby. Doxorubicin was given on separate admissions (at 22 weeks, 28 weeks, and 32 weeks AOG), and after each cycle, a nonstress test (NST) done showed reactive findings and normal fetal heart tones. At 28 weeks AOG, patient was also given betamethasone. Patient was discharged stable after each cycle of chemotherapy. At 29 weeks AOG, a repeat MRI done revealed no progression of the right pelvic mass (Figure 4).
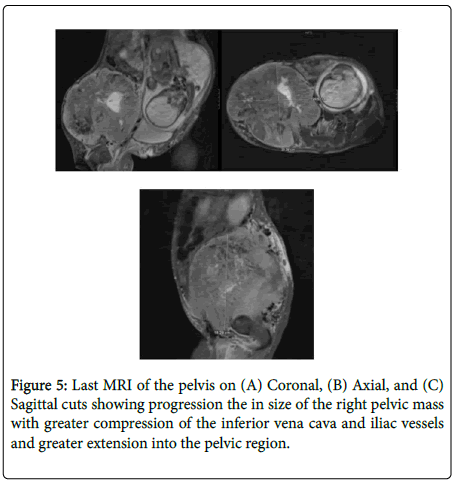
At 34 weeks AOG, patient perceived irregular uterine contractions. Betamethasone was again given. At this time, a repeat MRI of the pelvis showed progression the in size of the right pelvic mass (20.4 × 20.5 × 18.3 cm) (Figure 5). Due to persistence of moderate contractions despite tocolysis with nifedipine, terbutaline was given. After 3 days of admission, patient remained stable and was hence discharged.
At 35 weeks AOG, the patient noted watery vaginal discharge. She was admitted for premature rupture of membranes and underwent emergency cesarean section for cord prolapse. Postoperatively, the patient and infant were stable. Hemipelvectomy was again offered to the patient however was refused. Chest CT done showed several non-calcified pulmonary nodules in the left lung that were likely metastatic in nature. Patient opted to be discharged on the 5th day postpartum and was lost to follow-up.
At 2 months postpartum, patient was readmitted for fever associated with cough, weakness, and drowsiness. Upon admission, patient was febrile at 39.3C, and was stretcher-borne with grade 2 sacral ulcers. Right pelvic mass was measured at 25 × 28 cm. Assessment at this time was sepsis secondary to healthcare-associated pneumonia and sacral ulcers, hence she was started on antibiotics. On the 5th day of admission, patient was unresponsive. Advanced directives for no intubation and resuscitation were signed and patient was discharged against medical advice.
Discussion
Malignancy during pregnancy is known to be rare, affecting 1:1000 pregnancies with a reported incidence of 0.07% to 0.1% of malignancies [1-5], but with outcomes known to be devastating. Because of the rarity of this occurrence, this has only been the subject of very few studies so far. Hence, there has been a scarcity of guidelines regarding the clinical diagnosis and justifying the management of tumors during pregnancy.
In the review of available literature, the most common gestational cancers in terms of its organ of origin are breast and cervical cancer, followed by hematologic malignancies and melanoma [1-3,6-8], while the incidence of musculoskeletal tumors being comparably lower [3]. The most common presenting symptom for these tumors was noted to be pain (60%), followed by swelling or a mass (40%), [5] both of which were noted in our case. A diagnosis is then typically made histologically after a biopsy is obtained. When indicated, pathological examination of lesions should follow standard procedures as in the non-pregnant setting, including molecular analysis and staging of the malignancy [2].
Among the bone and soft tissue tumors, the most common primary bone malignancy was osteosarcoma (20%) [5], followed by Ewing sarcoma and chondrosarcoma [4,5]. It is of note that while the most common locations for these sarcomas are in the lower or upper extremities, chondrosarcoma is the most common subtype to be seen in the pelvis [4]. On the other hand, among the soft tissue sarcomas, leiomyosarcoma was the most common (50%), appearing often in the retroperitoneum, followed by the abdominal viscera [4]. To date, there has been no documented histiocytic sarcoma in the pelvis occurring in the pregnant population.
Upon final histopathologic diagnosis, treatment can now proceed. The American College of Obstetrics and Gynecology (ACOG) recommends that a pregnant woman should never be denied indicated surgery, regardless of trimester, while chemotherapy and radiotherapy require more specialized considerations [6-8]. As in our case, the patient was immediately offered the option of hemipelvectomy, which was refused in favor of a doxorubicin-based chemotherapy and the possibility of carrying her pregnancy to viable age.
A systemic review done by Azim, et al. (2010) found twelve patients with sarcoma treated with chemotherapy, mostly doxorubicin-based, treated during the course of pregnancy with variable outcomes, ranging from no fetal adverse events, to malformations such as cleft palate and trans-esophageal fistula, and to spontaneous abortions or fetal death from multi organ failure a few days after birth. This review concludes that systemic chemotherapy should not be started during the first trimester, but may be safely administered in the second or third trimester, with the exception of methotrexate and cisplatin [8]. Data on doxorubicin is reassuring, however it is important to note that all chemotherapeutic agents cannot be regarded as “safe” even when administered past the first trimester, hence recapitulating the importance of providing proper information regarding the effects of chemotherapy [8,2].
According to the case series of Figueiro-Filho et al. (2018), they reported that 7 out of 10 women diagnosed with malignancy during pregnancy delivered preterm, and among these, 5 infants were admitted at the NICU as a result of prematurity. This reiterates the significance of treating these mothers in hospitals with the facilities to care for preterm infants. While fetal loss was documented to be rare, this should also be discussed with mothers as a possible outcome of the pregnancy [5].
Likewise, maternal demise has also been documented in the same case series [5] and was seen in those with advanced malignancies. A patient, who opted to continue her pregnancy, in the same manner as our patient, succumbed to advanced metastatic disease. It is important to keep in mind that counseling pregnant women in terms of prognosis and survival is challenging, and can depend on the tumor type, stage, grade, location, and operability.
Conclusion
We are reporting a rare case of a soft tissue pelvic sarcoma in a pregnant patient. At any given time during the course of the pregnancy, a diagnosed malignancy can be treated with surgery, chemotherapy, or radiotherapy, but it is generally avoided during the first trimester of pregnancy due to the increased risk of complications or fetal adverse events. Ultimately, the treatment of malignancy in the pregnant patient should always be multi-disciplinary and individualized, depending largely on the decision of the mother once full disclosure of all options of management, possible risks, and prognosis have been discussed.
References
- Zagouri F, Dimitrakakis C, Marinopoulos S, Tsigginou A, Dimopoulos MA (2016) Cancer in pregnancy: Disentangling treatment modalities. ESMO Open. 1:e000016.
- Peccatori FA, Azim HA, Orecchia, R, Hoekstra HJ, Pavlidis N, et al. (2013 ) Cancer, pregnancy and fertility: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 24:vi160-70.
- Postl LK, Gradl G, Rothe RVE, Toepfer A, Pohlig F, et al. (2015) Management of musculoskeletal tumors during pregnancy: A retrospective study. BMC Womens Health15:48.
- Zarkavelis G, Petrakis D, Fotopoulos G, Mitrou S, Pavlidis N (2016) Bone and soft tissue sarcomas during pregnancy: A narrative review of the literature. J Adv Res 7:581-587.
- Figueiro-Filho E, Al-Sum H, Parrish J, Wunder J, Maxwell C (2018) Maternal and fetal outcomes in pregnancies affected by bone and soft tissue tumors. Am J Perinatol Rep 8:e343-e348.
- Rimawi BH, Green V, Lindsay M (2016) Fetal implications of diagnostic radiation exposure during pregnancy: Evidence-based recommendations. Clin Obstat Gynecol 59:412-418.
- Kal HB, Struikmans H (2005) Radiotherapy during pregnancy: Fact and fiction. Lancet Oncol 6:328-333.
- Azim HA, Peccatori FA, Pavlidis N (2010) Treatment of the pregnant mother with cancer: A systemic review on the use of cytotoxic, endocrine, targeted agents and immunotherapy during pregnancy. part I: solid tumors. Cancer Treatment Reviews 36:101-109.
Citation: Carolino DKD, Gonzales MRC, Rotor RS (2020) The Baby Bump and Malignant Lump: A Case Report of a Pregnant Patient with a Pelvic Sarcoma. J Orthop Oncol 6:135. DOI: 10.4172/2472-016X.1000135
Copyright: © 2020 Carolino DKD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4804
- [From(publication date): 0-2020 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 3957
- PDF downloads: 847