The Effects of Acupuncture on Mild Cognitive Impairment: A Pilot Study
Received: 31-Oct-2019 / Accepted Date: 19-Nov-2019 / Published Date: 26-Nov-2019 DOI: 10.4172/2161-0460.1000479
Abstract
Objective: To evaluate the effects of acupuncture on cognition, mood, quality of life and physical performance in individuals with mild cognitive impairment due to Alzheimer’s disease (MCI-AD).
Methods: A quasi-experimental 8-week study was conducted with MCI-AD individuals (mean age: 74.3+5.3 y; 50% Female) using an Intent-To-Treat (ITT) and a Last Observation Carried Forward (LOCF) approach. Acupuncture was perform twice weekly for 8 weeks. Outcomes measures were collected at baseline, 4 weeks and 8 weeks. Cognition was assessed by the Montreal Cognitive Assessment, mood was assessed with the Hospital Anxiety and Depression Scale, mindfulness was assessed with the Applied Mindfulness Process Scale and physical performance was assessed by computerized gait and balance measurements, Mini-Physical Performance Test, Berg Balance Scale, Timed-Up-and-Go (TUG), Dynamic Gait Index (DGI) and Five Times Sit-to-Stand (STS-5) tests.
Results: Twelve individuals were enrolled and 11 competed all 16 sessions. There was a trend towards improvement in cognition (p=0.09) on ITT analyses that met significance in the LOCF analyses (p=0.02). Significant improvements with ITT analyses were found in depressive symptoms (p=0.04), mindfulness (p=0.04), the miniphysical performance test (p=0.04), Berg balance test (p=0.005), TUG (p=0.001), DGI (p=0.04) and STS-5 (p=0.02).
Conclusion: Acupuncture in MCI-AD may provide improvements in cognition, mood, mindfulness and physical performance. A larger double-blind study is warranted.
Keywords: Acupuncture; Mild cognitive impairment; Alzheimer’s disease; Dementia; Non-pharmacological approaches; Cognitive outcomes; Physical performance outcomes
Introduction
Mild Cognitive Impairment (MCI) represents a transitional stage between normal brain aging and dementia, with cognitive decline in the absence of significant impairment in everyday functioning. MCI can be due to many causes and may not always progress to dementia such as Alzheimer’s disease (AD). More recently, the term mild cognitive impairment due to Alzheimer’s disease (MCI-AD) has been used to refer specifically to the symptomatic prodromal phase of AD. Advances in the understanding of the pathoetiology of MCI and AD have improved the ability of the clinician to rigorously apply core clinical criteria to establish MCI-AD [1]. The MCI-AD diagnosis corresponds well to underlying brain pathology [2].
According to the 2019 Alzheimer’s Association Alzheimer’s Disease Facts and Figures Report approximately 15-20% of people age 65 or older have MCI [3]. A meta-analysis of 41 studies that found that among individuals with MCI who were tracked for 5 years or longer, 38 percent progressed to dementia [4]. Individuals with MCI due to AD (MCI-AD) are more likely to develop AD than people without MCI [1-3]. Risk factors (e.g., age, diabetes, Apo lipoprotein E) and biomarkers may aid in predicting conversion to AD [1-7]. Once diagnosed with MCI-AD, there is no known way to reverse the effects and there are no approved medications to treat MCI-AD. Therefore, at the present time, a focus is on how best to delay the progression of MCI-AD using preventative approaches that includes non-pharmacological methods, diet and lifestyle changes [8,9].
Acupuncture may offer a novel approach to treat MCI and AD, taking advantage of increasing interest in integrative medicine approaches to healthcare [10,11]. Acupuncture is an integral part of Traditional Chinese Medicine (TCM) and may play a role in the treatment of a wide range of neurodegenerative disease [12,13]. In TCM, aging and cognitive decline can impair “Qi”, the vital energy that circulates through the body and that impairment in Qi function may decrease flow of body fluids required for optimal brain function [13,14]. Organs in TCM are not anatomical structures but rather functional circuits that interact with each other as well as essential substances such as Qi [12]. TCM postulates that imbalances in Qi may be addressed through acupuncture manipulations of meridians, channels by which the human body’s “Qi” are circulated and maintain balance [12,15].
Finding an effective alternative treatment to prevent or delay the impact and progression of MCI-AD is an ongoing research effort. With its ease of application, limited side effect profile and potential for health related benefits, acupuncture may provide clinical benefits while other treatments are being developed. Little is known about the clinical effect and safety of acupuncture in patients diagnosed with MCI-AD [16-18]. There are few studies to date that have explored the effects of acupuncture on cognitive disorders and most of these have been limited to vascular cognitive impairment and nearly all conducted in China [18- 23].
The biological mechanisms of acupuncture effects on memory are not yet fully elucidated. A study of 22 individuals with and without MCI performed resting state Functional Magnetic Resonance Imaging (fMRI) [16]. Acupuncture, but not the sham condition, induced amplitude of low frequency fluctuations in the medial frontal gyrus, inferior temporal gyrus and posterior cingulate gyrus all regions affected by AD pathology [2,16]. In another acupuncture study of 8 MCI, 14 AD and 14 controls, fMRI also demonstrated changes in temporal and frontal lobe regions [18]. Several animal studies have suggested that acupuncture may improve learning and cerebral blood flow following experiments ischemic models [24,25]. These studies supported the scientific rationale for why acupuncture could offer potential benefits in cognitive disorders. To test the effect of acupuncture on MCI-AD, we conducted a pilot single arm clinical trial.
Material and Methods
Intervention
The study was an 8 week open label, quasi-experimental design. Needle retention was for 30 min, twice a week for 8 weeks and 16 times in total. Outcome measures and physical function testing were performed before starting acupuncture intervention to establish a baseline. A midpoint assessment at week 4 and a post-intervention assessment after week 8 were collected. Any potential Adverse Events (AE) were collected and rated as definitely related, probably related, possibly related or not related to the intervention.
Participants
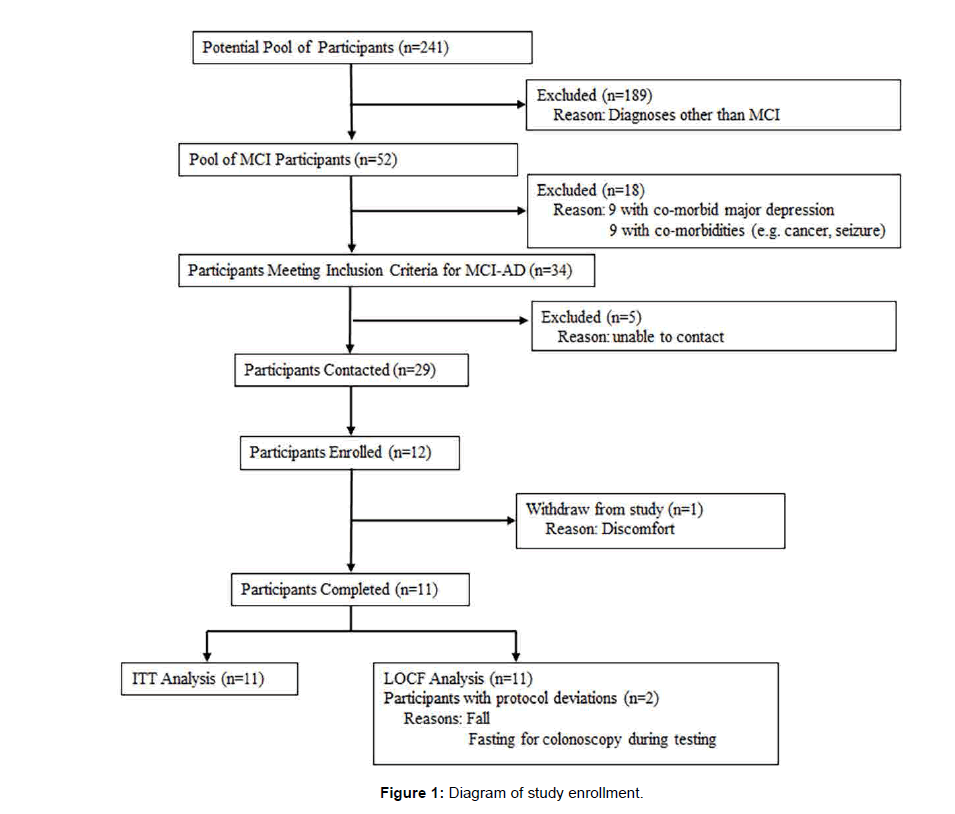
Participants were recruited from a pool of well-characterized patients (N=241) seen at the Comprehensive Center for Brain Health at Florida Atlantic University. All participants were evaluated by an interdisciplinary team led by an experienced cognitive-behavioral neurologist (JEG) who provided diagnoses for all participants [26]. The clinical assessment included a comprehensive neurological examination and neuropsychological test battery, the Clinical Dementia Rating (CDR) and its sum of boxes (CDR-SB), magnetic resonance imaging and laboratory tests to establish diagnoses [27,28]. Inclusion criteria for the study included age 60-85 y inclusive, diagnosis of MCI due to AD, CDRSB> 0.5, ability to provide informed consent and intention to participate in the entire study from September-December 2018. Exclusion criteria included MCI due to other disorders (e.g., cerebrovascular disease, Lewy bodies), a diagnosis of dementia, Primary Axis I diagnoses (i.e., major depressive disorder), active skin infections, cancer within the last 5 years or concomitant medications or medical conditions that would potentially interfere with acupuncture or the conduct of the study. The overall recruitment plan was designed to capture the wide range of cognitive abilities and functional impairments in MCIAD to study the potential efficacy of acupuncture, while also limiting potential confounders by excluding individuals who had MCI likely due to other disorders. The lower age limit was selected to eliminate individuals who are likely too young to have AD as the cause of their MCI, while the upper limit was selected to eliminate individuals whose physical frailty and co-morbidities might preclude completion of all the study requirements. Fifty two patients were identified as having MCI. Of these 34 individuals had amnestic deficits +/- other domains, relative preservation of activities of daily living, a global CDR of 0.5, no laboratory abnormalities suggesting reversible causes for their impairments, MRI findings of hippocampal atrophy without other significant brain pathology and no co-morbidity (depression, stroke, sleep apnea) that were thought to have AD as the most likely underlying cause of their MCI (i.e. MCI-AD) [1,2]. Although some participants reported depressive or anxiety symptoms, none met criteria for major depressive disorder or generalized anxiety disorder. Twenty-nine patients were contacted and 12 individuals consented to participate in the study. This study was approved by the Institutional Review Board of Florida Atlantic University and each participant provided written informed consent in person (Figure 1).
Procedures
The participant was placed in either the supine or prone position depending on the patient’s choice of comfort for the remainder of the study. The skin at the acupoint regions was routinely disinfected with 70% isopropyl alcohol with a sterile cotton ball. The choice for acupuncture needles with guide tubes was (JOCU, EZ Medical, Germany). The disposable, sterile acupuncture needle size was 32 gauges, 0.25 mm × 30 mm long. Needle manipulation was by lifting, thrusting, twirling and rotating in order to elicit the De-qi phenomenon, regarded in TCM as the key to successful treatment [29]. This sensation has been reported as a dull ache, distension, a warm sensation, heaviness or a slight throbbing. Different De-qi sensations represent activation of different nerve fibers with numbness sensed by Aβ/γ fibers, distention and heaviness by Aδ fibers and soreness and achiness by C fibers [30]. De-qi sensation is frequently used as a sign by acupuncturists that the therapeutic effects have been initiated [29]. Needle retention was for 30 min, twice a week for 8 weeks and 16 times in total. During the acupuncture intervention patients were closely observed and monitored to address any concerns or discomfort. All patients in this study received acupuncture intervention. Location of all acupoints are in accordance with the National Standard Name and Location of Acupoints (GB/T12346-2006) [31,32]. The acupoints were selected based on a search of the literature for prior use in cognitive disorders and compensate for theoretical Qi deficiencies associated with MCI based on the clinical acupuncture practices of the author (TW) and his mentors [15,16]. All acupuncture procedures were performed by the same experienced acupuncture provider (TW) for the duration of the study (Table 1).
| Acupoint | Name | Insertion Angle | Depth (cun) | Meridian | TCM Organ | Location |
|---|---|---|---|---|---|---|
| GV 20 (Unilateral) |
Baihui | Transverse | 0.5-1.0 | Yang | Governing Vessel | At the vertex on the midline, in the depression 5 cun posterior to the anterior hairline and 7 cun superior to the posterior hairline. |
| GV 24 (Unilateral) |
Shenting | Transverse | 0.5-1.0 | Yang | Governing Vessel | At the top of the head on the midline, 0.5 cun posterior to the anterior hairline and 0.5 cun anterior to Shangxing DU 23 |
| GB 20 (Bilateral) |
Fengchi | Slightly oblique inferior, directed toward the tip of the nose | 1.0-1.5 | Yang | Gall Bladder | Below the occiput, approximately midway between Fengfu DU 16 and Wangu GB 12, in the hollow between the origins of the sternocleidomastoid and trapezius muscles. |
| KI 3 (Bilateral) |
Taixi | Perpendicular | 0.5-1.0 | Yin | Kidney | In the depression between the medial malleolus and the Achilles tendon, level with the prominence of the medial malleolus |
| EX-HN 1 (Extra Point) |
Sishencong | Transverse | 0.5-1.5 | Not applicable | Not applicable | Cluster of four points at the vertex of the scalp, grouped around Baihui DU 20 or otherwise named GV 20 and located 1 cun anterior, posterior and lateral to GV 20 |
| GV 26 (Unilateral) |
Renzhong (Shuigou) | Oblique, directed superiorly | 0.3-0.5 | Yang | Governing Vessel | Above the upper lip on the midline, at the junction of the upper third and lower two thirds of the philtrum |
| GV 14 (Unilateral) |
Dazhui | Perpendicular-oblique superior | 0.5-1.0 | Yang | Governing Vessel | On the midline, below the spinous process of the 7th cervical vertebra (C7) |
| CV 4 (Unilateral) |
Guanyuan | Perpendicular | 0.5-1.0 | Yin | Conception Vessel | On the midline of the lower abdomen, 3 cun inferior to the umbilicus and 2 cun superior to the pubic symphysis |
| HT 7 (Bilateral) |
Shenmen | Oblique, medially | 0.3-0.8 | Yin | Heart | At the wrist joint, on the radial side of flexor carpi ulnaris, in the depression at the proximal border of the pisiform bone |
| BL15 (Bilateral) |
Xinshu | Transverse- oblique | 1.0-1.5 | Yang | Bladder | 1.5 cun lateral to the lower border of the spinous process of the 5th thoracic vertebra (T5) |
| BL 23 (Bilateral) |
Shenshu | Perpendicular-oblique, towards spine | 1.0-1.5 | Yang | Bladder | 1.5 cun lateral to the lower border of the spinous process of the 2nd lumbar vertebra (L2) |
| ST 36 (Bilateral) |
Zusanli | Perpendicular | 1.0-1.5 | Yang | Stomach | Below the knee, 3 cun inferior to Dubi ST 35, one fingerbreadth lateral to the anterior crest of the tibia |
| SP 6 (Bilateral) |
Sanyinjiao | Oblique proximal | 1.0-1.5 | Yin | Spleen | On the medial side of the lower leg, 3 cun superior to the prominence of the medial malleolus, in a depression close to the medial crest of the tibia |
| KI 1 (Bilateral) |
Yongquan | Perpendicular | 0.5-1.0 | Yin | Kidney | On the sole of the foot, between the 2nd and 3rd metatarsal bones, approximately one third of the distance between the base of the second toe and the heel, in a depression formed when the foot is plantarflexed |
| *Cun is a measurement used to find acupoints. One ‘cun’ is equal to the space between the distal interphalangeal joint and the proximal interphalangeal joint on the middle finger | ||||||
Table 1: Selected acupoints and associated meridians and Traditional Chinese Medicine (TCM) organs.
Outcome measures
Information on demographics, medical and injury history, medications, co-morbidities and alcohol, tobacco and substance use history was collected as part of their diagnostic evaluation. Outcome measures were selected to provide assessment of cognition, mood, health-related quality of life and physical performance. The Montreal Cognitive Assessment Scale (MoCA, Forms a, b, c) was used as a global measure of cognitive performance [33]. Alternate forms were used to eliminate practice effect. The Hospital Anxiety and Depression Scale (HADS) is a 14-point scale with orthogonal scores for distinct ratings of depression (HADS-D) and anxiety (HADS-A) [34]. The Quality of Life in Alzheimer’s Disease (QoL-AD) was used to capture the patients perceptions of their quality of life, validated in MCI [35,36]. The Applied Mindfulness Scale was used to capture domains of mindfulness, including decentering, positive emotional regulation and negative emotional regulation [37]. Physical assessments include (a) computerized gait analysis with the ZenoMat electronic walkway (ProtoKinetics, Havertown PA) measuring velocity, cadence and gait cycle metrics, (b) body sway analysis was measured using Falltrak II System (MedTrak VNG Inc, Henderson NV), (c) Berg Balance Scale measures balance, stable and anticipatory postural control, (d) the 5-times Sit to Stand Scale (STS-5) measuring the time for a person to arise from a seated position with arm folded and sit back down 5 times, (e) the Timed Up and Go (TUG) measuring the time required for an individual to arise from a chair, walk 3 m, turn around, walk back to the chair and sit down, (f) the Dynamic Gait Index (DGI) measuring 8 tasks of gait and dynamic posture in different sensory contexts and (g) Grip Strength using a dynamometer [38-45]. A global measure of physical functionality was measured with the mini Physical Performance Test (mPPT), a 16-point scale to determine functionality. Body composition was determined using the in Body 770 Bioimpedance (InBody Co, LTD, Cerritos, CA) method for lean muscle mass, body water and body fat [46]. All outcome measures were completed by the same physical therapist (AR) for the duration of the study.
Statistical analyses
Descriptive statistics including means and frequency distributions for sociodemographic characteristics and study outcomes were used to characterize the sample. Pre-post differences between all time-points (Time 1 vs. Time 2, Time 2 vs. Time 3, Time 1 vs. Time 3) were assessed with paired t tests. Data were analyzed with two analytic approaches [47]. An Intent-to-treat (ITT) analysis, widely used in clinical trials, is a strategy for reducing potential biases in observed treatment effects by including all participants who started the trial, regardless of adherence to protocol (e.g. deviations, dropout, withdrawal) [48,49]. The strength of ITT analyses include preserving integrity of group assignment and providing a more realistic estimate of true treatment effects in the “real-world” where patients may not always follow treatment regimens [48]. However, missing data and protocol deviations may occur during most clinical research projects, therefore modified ITT analyses are often used in order to preserve study power and control for potential confounding factors [49,50]. One such modified ITT strategy is the Last-Observation-Carried-Forward (LOCF) approach, which substitutes missing outcome data with the last measurement taken before issues with protocol adherence [50]. In this pilot study, two such instances occurred at time 3 in two subjects (i.e. fasting extended time to assessment due to previous fall). All analyses were performed with SAS V9.4 (IBM, Armonk, NY). A p value of <0.05 was considered indicative of statistical significant change, while a p-value <0.1 was considered indicative of a clinically meaningful trend. Given the pilot nature of the study, no correction for multiple comparisons was performed.
Results
Sample characteristics
A total of 52 individuals meeting criteria for MCI were evaluated at CCBH over the past 2 years, of this total, 29 individuals met inclusion criteria for MCI-AD and were contacted to participate in the study [1,2]. A total of 12 individuals were consented and enrolled in the study. The mean age of the sample at baseline was 74.3 ± 5.3 y (range 67-84), 50% were women and 73% were married. The mean years of education was 15.6 ± 2.9 y (range 12-20). The mean CDR-SB was 1.4 ± 0.8 (range 0.5-3) consistent with mild cognitive impairment. The mean baseline MoCA score was 25.0 ± 2.5 (range 19-28) consistent with mild global impairments. The mean baseline HADS-A score was 4.9 ± 4.1 (range 0-14) and mean baseline HADS-D score was 3.3 ± 3.4 (range 0-12) consistent with a range of symptomatology from no complaints to mild symptoms. One individual dropped out after the first 3 sessions due to discomfort from the acupuncture needle, thus 11 individuals were followed for the duration of the study, completing all three outcome measurement periods (baseline, 4 weeks and 8 weeks). All 11 participants completed the study, however 2 individuals deviated from the pre-specified study protocol. One participant (female) missed their final assessment due to a fall and was not evaluated with outcome measures until 1 month after the last acupuncture treatment. One participant (male) was fasting for a colonoscopy and reported not feeling well during the cognitive and physical testing. He did not inform the study team until several days later. To account for protocol deviations, outcomes were evaluated with both ITT and LOCF approaches for the 11 individuals [48-50]. A total of three adverse events were reported. One AE (discomfort from needle) was related to the intervention. Two other AEs (fall and fatigue) were not related to the intervention. No serious adverse events were reported (Figure 1).
Intent to treat analyses
Cognitive outcomes: Cognitive outcomes included measures of global cognition (MoCA), mood (HADS-A and HADS-D subscales), mindfulness (AMPS) and quality of life ratings (QoL-AD) (Table 2).
| Time 1 Baseline | Time 2 4 Weeks | Time 3 8 Weeks | p value Time 2-Time 1 | p value Time 3-Time 1 | p value Time 3-Time 2 | ||
|---|---|---|---|---|---|---|---|
| Cognitive outcomes | MoCA | 25.1 ± 2.6 | 26.1 ± 2.6 | 26.3 ± 2.8 | 0.199 | 0.090 | 0.889 |
| HADS-Anxiety | 4.1 ± 3.2 | 3.8 ± 3.1 | 2.8 ± 2.0 | 0.787 | 0.203 | 0.314 | |
| HADS-Depression | 2.5 ± 2.2 | 2.2 ± 1.8 | 1.3 ± 1.3 | 0.572 | 0.040 | 0.016 | |
| AMPS-Mindfulness | 36.9 ± 15.9 | 45.5 ± 7.9 | 44.5 ± 11.7 | 0.029 | 0.036 | 0.654 | |
| QoL-AD | 42.9 ± 5.2 | 46.3 ± 4.2 | 45.4 ± 4.5 | 0.004 | 0.080 | 0.356 | |
| Physical function outcomes | mPPT | 13.6 ± 1.7 | 14.0 ± 1.5 | 14.5 ± 0.8 | 0.492 | 0.043 | 0.052 |
| Berg | 54.1 ± 1.8 | 54.7 ± 1.8 | 55.0 ± 1.3 | 0.011 | 0.005 | 0.277 | |
| DGI | 21.7 ± 2.8 | 23.0 ± 1.5 | 23.7 ± 0.5 | 0.046 | 0.045 | 0.120 | |
| TUG | 7.3 ± 1.2 | 6.6 ± 0.8 | 6.2 ± 0.8 | 0.022 | 0.001 | 0.084 | |
| STS 5 | 11.4 ± 2.7 | 10.0 ± 1.8 | 9.6 ± 1.7 | 0.018 | 0.021 | 0.081 | |
| Grip strength | 25.4 ± 8.5 | 25.8 ± 10.2 | 26.5 ± 9.6 | 0.645 | 0.162 | 0.139 | |
| *Mean ± Standard Deviation; Significant p-values are in BOLD MoCA: Montreal Cognitive Assessment; HADS: Hospital Anxiety and Depression Scale; AMPS: Applied Mindfulness Process Scale; QoL-AD: Quality of Life in Alzheimer’s Disease; mPPT: Mini Physical Performance Test; DGI: Dynamic Gait Index; TUG: Timed Up and Go; STS5: Five Times Sit to Stand | |||||||
Table 2: Results from Intent to Treat (ITT) Analyses (n=11).
Global cognition showed trends towards improvement from baseline to 8 weeks (25.1 vs. 26.3, p=0.090). There was no change in measures of anxiety however there was a significant improvement in depressive symptoms (2.5 vs. 1.3, p=0.040) and mindfulness (36.9 vs. 44.5, p=0.036). Improvement in mood was seen at week 8 while improvements in mindfulness was seen at week 4. There was a trend towards improved quality of life ratings (42.9 vs. 45.4, p=0.08) that peaked by week 4 (p=0.004).
Physical performance outcomes: Physical performance measures included measures of global functionality (mPPT), gait speed (ZenoMat), postural sway (FallTrak II), overall balance (Berg), ability to arise from a chair (STS-5 and TUG), dynamic gait and posture (DGI) and grip strength (dynamometer).
There was a significant improvement in overall physical functionality measured with the mPPT (13.6 vs. 14.5, p=0.043) as well as gait and balance measured by Berg (54.1 vs. 55.0, p=0.005), DGI (21.7 vs. 23.7, p=0.045), TUG (7.3 vs. 6.2, p=0.001) and STS-5 (11.4 vs. 9.6, p=0.021). Gait and balance benefits were detected by week 4 and persisted through the end of the study. There was a trend towards improved grip strength (25.4 vs. 26.8, p=0.056). No changes were found in computerized measurements of gait speed or postural sway (data not shown). There were no changes in anthropometric measurements (data not shown).
Locf analyses
Cognitive outcomes: Using LOCF approaches, global cognition showed significant improvements beginning at week 4 that was maintained at week 8 (25.1 vs. 27.1, p=0.019). There were strong trends towards improvement in depressive symptoms (2.5 vs. 1.4, p=0.07), mindfulness (36.9 vs. 43.9, p=0.058), self-reported quality of life (42.9 vs. 45.2, 0.045) with the lowest scores seen at week 8. There was no change in anxiety symptoms (Table 3).
| Time 1 Baseline |
Time 2 4 Weeks |
Time 3 8 Weeks |
P value Time 2-Time 1 |
P value Time 3-Time 1 |
P value Time 3-Time 2 |
||
|---|---|---|---|---|---|---|---|
| Cognitive outcomes | MoCA | 25.1 ± 2.6 | 26.1 ± 2.6 | 27.1 ± 2.4 | 0.199 | 0.019 | 0.019 |
| HADS-Anxiety | 4.1 ± 3.2 | 3.8 ± 3.1 | 3.5 ± 3.3 | 0.787 | 0.566 | 0.441 | |
| HADS-Depression | 2.5 ± 2.2 | 2.2 ± 1.8 | 1.4 ± 1.4 | 0.572 | 0.071 | 0.031 | |
| AMPS-Mindfulness | 36.9 ± 15.9 | 45.5 ± 7.9 | 43.9 ± 11.4 | 0.029 | 0.058 | 0.478 | |
| QoL-AD | 42.9 ± 5.2 | 46.3 ± 4.2 | 45.2 ± 3.7 | 0.004 | 0.045 | 0.025 | |
| Physical function outcomes | mPPT | 13.6 ± 1.7 | 14.0 ± 1.5 | 14.4 ± 1.3 | 0.492 | 0.087 | 0.104 |
| Berg | 54.1 ± 1.8 | 54.7 ± 1.8 | 54.8 ± 1.7 | 0.011 | 0.012 | 0.588 | |
| DGI | 21.7 ± 2.8 | 23.0 ± 1.5 | 23.4 ± 1.2 | 0.046 | 0.015 | 0.221 | |
| TUG | 7.3 ± 1.2 | 6.6 ± 0.8 | 6.2 ± 0.7 | 0.022 | 0.001 | 0.077 | |
| STS 5 | 11.4 ± 2.7 | 10.0 ± 1.8 | 9.7 ± 2.0 | 0.018 | 0.014 | 0.095 | |
| Grip strength | 25.4 ± 8.5 | 25.8 ± 10.2 | 26.8 ± 9.7 | 0.645 | 0.056 | 0.013 | |
| *Mean ± Standard Deviation; significant p-values are in BOLD MoCA: Montreal Cognitive Assessment; HADS: Hospital Anxiety and Depression Scale; AMPS: Applied Mindfulness Process Scale; QoL-AD: Quality of Life in Alzheimer’s disease; mPPT: Mini Physical Performance Test; DGI: Dynamic Gait Index; TUG: Timed Up and Go; STS5: Five Times Sit to Stand |
|||||||
Table 3: Results from Last Observation Carried Forward (LOCF) Analyses (n=11).
Physical performance outcomes: Using LOCF approaches, there was a significant improvement in gait and balance measured by Berg (54.1 vs. 54.8, p=0.012), DGI (21.7 vs. 23.4, p=0.015), TUG (7.3 vs. 6.2, p=0.001) and STS-5 (11.4 vs. 9.7, p=0.014). These effects were seen by week 4 and persisted through the end of the study. There was a trend towards improvement in overall physical functionality measured with the mPPT (13.6 vs. 14.4, p=0.088) and grip strength (25.4 vs. 26.8, p=0.056). No changes were found in computerized measurements of gait speed or postural sway (data not shown). There were no changes in anthropometric measurements (data not shown).
Discussion
In our pilot study of MCI-AD individuals, acupuncture demonstrated benefits in cognition, mood, mindfulness and physical performance. Global measures of cognition (MoCA) and mood (HADS-D) were both improved and may have overlapping benefits, i.e. improvements in mood may lead to improvements in cognitive performance. Acupuncture in the MCI-AD individuals also demonstrated significant improvements across measurements of global physical functionality. This may be particularly relevant as there is a strong bidirectional relationship between cognitive and physical performance and changes in physical functionality may herald progression of MCI to dementia [51-53].
There is a limited body of literature on the use of acupuncture in patients with cognitive impairment, with most studies involving vascular cognitive impairment. A recent study explored the role of acupuncture in reducing risk of dementia following traumatic brain injury suggesting that at least 5 sessions of acupuncture may be required to receive benefits [54]. In a study of 216 patients with vascular cognitive impairment, acupuncture had a favorable effect on ADAS-Cog scores compared with citocoline treatment [22]. However, a Cochrane systematic review of acupuncture for vascular dementia found that the absence of randomized clinical trials makes it difficult to evaluate efficacy [23]. In a randomized controlled trial of 87 patients with mild to moderate AD, acupuncture was compared with a group of individuals treated with the cholinesterase inhibitor, donepezil [21]. The acupuncture group had smaller decreases in ADAS-Cog and CIBIC-Plus scores compared with donepezil and had fewer adverse events [21]. A meta-analysis of acupuncture trials for amnestic mild cognitive impairment reviewed 5 trials with 568 participants compared acupuncture to nimodipine therapy and demonstrated better clinical efficacy with mini mental state examination scores [15]. However, there was concern about the low methodological quality of the included trials. Prior studies in individuals with and without MCI demonstrated changes in fMRI and animal studies of acupuncture demonstrated improve learning and cerebral blood flow [16,18,24,25].
This study and future controlled trials can accelerate the development of acupuncture as a therapeutic modality to be included in adjunctive complimentary medicine treatment models that may play a role in changing the mindset of current treatment protocols in Western medicine [12]. For example, a recent study explored the effects of Shiatsu for depression in AD and showed improvements in depression scores [55].
Study Limitations
This was a pilot study and the absence of a control (placebo) group limits the full understanding of the possible benefits of acupuncture in MCI-AD. The rigorous quasi-experimental design and the use of ITT and LOCF analyses overcome some of these limitations. There have been concerns that if LOCF analyses are the only analyses presented that bias may be introduced. However, if similar results are present in both ITT analyses (which include all data points) and LOCF (which includes all adherence data points), then the results are less likely to be biased [48-50]. In a review of 72 studies analyzing data from 23,842 patients, no significant differences in treatment effects were found between ITT and modified ITT analyses [56]. However, a true randomized, placebo-controlled trial will be necessary to demonstrate full effect of acupuncture on cognition, mood and function in individuals with MCIAD. No amyloid or tau biomarkers were included in this pilot study and diagnoses were established on clinical grounds using rigorously applied diagnostic criteria and MRI [1]. Future studies may include biomarkers to better explain biological mechanisms of acupuncture benefits [2].
Conclusion
Even with the limitations of a small sample size, acupuncture improved cognition, mood, mindfulness and physical performance, with many effects seen as soon as 4 weeks, with similar findings in both the ITT and LOCF analyses. This pilot study suggests that acupuncture had a therapeutic effect on MCI-AD patients and there is compelling evidence to investigate this further in a placebo-controlled study with a larger sample size and longer duration of follow-up. From the results of this study, acupuncture appears to be a potentially an effective and safe intervention for MCI-AD patients. This study provides a foundation for future research to further explore the effect of acupuncture on patients diagnosed with MCI-AD.
Declarations
Ethics approval and consent to participate: This study was approved by the Institutional Review Board of Florida Atlantic University.
Consent for publication: All participants signed informed consent prior to enrollment in the study.
Availability of data and material: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests: The authors report no conflicts of interest in this work.
Funding: This project was supported by grants from the National Institute on Aging (R01 AG040211), the Harry T. Mangurian Foundation and Anne and Leo Albert Charitable Trust.
Authors’ contributions: TW conceived the idea, helped design the study, performed the acupuncture intervention and helped write the manuscript. AR helped design the study, performed all the outcome measures and helped write the manuscript. MT helped design the study, performed statistical analyses and helped write the manuscript. JEG helped design the study, performed statistical analyses, provided funding and helped write the manuscript.
Acknowledgement
The authors would like to thank Professor Yang Jun, MD, PhD from the Anhui University of Chinese Medicine for encouragement and assistance with translation of Chinese literature.
References
- Albert MS, De Kosky ST, Dickson D, Dubois B, Feldman HH, et al. (2011) The diagnosis of mild cognitive impairment due to Alzheimer's disease: Recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 7: 270-279.
- Jack CR, Bennett DA, Blennow K, Carillo MC, Dunn B, et al. (2018) NIA-AA research framework: Toward a biological definition of Alzheimer's disease. Alzheimers Dement 14: 535-562.
- Mitchell AJ, Shiri-Feshki M (2009) Rate of progression of mild cognitive impairment to dementia--meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand 119: 252-265.
- Li JQ, Tan L, Wang HF, Tan MS, Tan L, et al. (2016) Risk factors for predicting progression from mild cognitive impairment to Alzheimer's disease: A systematic review and meta-analysis of cohort studies. J Neurol Neurosurg Psychiatry 87: 476-484.
- Ferreira D, Rivero-Santana A, Perestelo-Pérez L, Westman E, Wahlund LO, et al. (2014) Improving CSF biomarkers' performance for predicting progression from mild cognitive impairment to Alzheimer’s disease by considering different confounding factors: A meta-analysis. Front Aging Neurosci 6: 287.
- Hu C, Yu D, Sun X, Zhange M, Wasng L, et al. (2017) The prevalence and progression of mild cognitive impairment among clinic and community populations: A systematic review and meta-analysis. Int Psychogeriatr 29: 1595-1608.
- Hodes JF, Oakley CI, O'Keefe JH, Lu P, Galvin JE, et al. (2019) Alzheimer's "prevention" vs. "risk reduction": Transcending semantics for clinical practice. Front Neurol 9: 1179.
- Galvin JE (2017) Prevention of Alzheimer’s disease: Lessons learned and applied. J Am Geriatr Soc 65: 2128-2133.
- Zhang H, Zhao L, Yang S, Chen Z, Li Y, et al. (2013) Clinical observation on effect of scalp electro acupuncture for mild cognitive impairment. J Tradit Chin Med 33: 46-50.
- Zhou J, Peng W, Xu M, Li W, Liu Z (2105) The effectiveness and safety of acupuncture for patients with Alzheimer disease: A systematic review and meta-analysis of randomized controlled trials. Medicine 94: e933.
- Efferth T, Xu AL, Lee DYW (2019) Combining the wisdoms of traditional medicine with cutting-edge science and technology at the forefront of medical sciences. Phytomedicine 64: 153078.
- Guo X, Ma T (2019) Effects of acupuncture on neurological disease in clinical and animal-based research. Front Integr Neurosci 13: 47.
- Lyu R, Gao M, Yang H, Wen Z, Tang W (2019) Stimulation parameters of manual acupuncture and their measurement. Evid Based Complement Alternat Med 2019: 1725936.
- Deng M, Wang XF (2016) Acupuncture for amnestic mild cognitive impairment: A meta-analysis of randomised controlled trials. Acupunct Med 34: 342-348.
- Jia B, Liu Z, Min B, Wang Z, Zhou A, et al. (2015) The effects of acupuncture at real or sham acupoints on the intrinsic brain activity in mild cognitive impairment patients. Evid Based Complement Alternat Med 2015: 529675.
- Kim MW, Yoo JH, Go HJ. Kim SW, Jang SW, et al. (2019) Systematic review of acupuncture treatment for mild cognitive impairment. J Acupunct Res 36: 72-79.
- Wang Z, Nie B, Li D, Zhao Z, Han Y, et al. (2012) Effect of acupuncture in mild cognitive impairment and Alzheimer disease: A functional MRI study. PLoS One 7: e42730.
- Liu F, Shen C, Yao L, Li Z (2018) Acupoint massage for managing cognitive alterations in older adults: A systematic review and meta-analysis. J Altern Complement Med 24: 532-540.
- Tu CH, MacDonald I, Chen YH (2019) The effects of acupuncture on glutamatergic neurotransmission in depression, anxiety, schizophrenia and Alzheimer’s disease: A review of the literature. Front Psychiatry 10: 14.
- Jia Y, Zhang X, Yu J, Han J, Yu T, et al. (2017) Acupuncture for patients with mild to moderate Alzheimer's disease: A randomized controlled trial. BMC Complement Altern Med 17: 556.
- Yang JW, Shi GX, Zhang S, Tu JF, Wang LQ, et al. (2019) Effectiveness of acupuncture for vascular cognitive impairment no dementia: A randomized controlled trial. Clin Rehabil 33: 642-652.
- Peng WN1, Zhao H, Liu ZS, Wang S (2007) Acupuncture for vascular dementia. Cochrane Database Syst Rev 2: CD004987.
- Lin R, Yu K, Li X, Tai J, Lin Y, et al. (2016) Electroacupuncture ameliorates post-stroke learning and memory through minimizing ultrastructural brain damage and inhibiting the expression of MMP-2 and MMP-9 in cerebral ischemia-reperfusion injured rats. Mol Med Rep 14: 225-233.
- Kim JH, Choi KH, Jang YJ, Bae SS, Shin BC, et al. (2013) Electroacupuncture acutely improves cerebral blood flow and attenuates moderate ischemic injury via an endothelial mechanism in mice. PLoS One 8: e56736.
- Galvin JE, Valois L, Zweig Y (2014) Collaborative transdisciplinary team approach for dementia care Neurodegener Dis Manag 4: 455-469.
- Morris JC (1993) The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurol 43: 2412-2414.
- Williams MM, Storandt M, Roe CM, Morris JC (2013) Progression of Alzheimer's disease as measured by clinical dementia rating sum of boxes scores. Alzheimers Dement 9: S39-44.
- Zhu SP, Luo L, Zhang L, Shen SX, Ren XX, et al. (2013) Acupuncture De-qi: From characterization to underlying mechanism. Evid Based Complement Alternat Med 2013: 518784.
- Wang KM, Yao SM, Xian YL, Hou ZL (1985) A study on the receptive field of acupoints and the relationship between characteristics of needling sensation and groups of afferent fibres. Sci Sin B 28: 963-971.
- Deadman P (2007) A manual of acupuncture. 2nd Edition. Journal of Chinese Medicine, UK, p 675.
- Ahn AC, Martinsen OG (2007) Electrical characterization of acupuncture points: Technical issues and challenges. J Altern Complement Med 13: 817-824.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, et al. (2005) The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 53:695-699.
- Snaith RP (2003) The hospital anxiety and depression scale. Health Qual Life Outcomes 1: 29.
- Logsdon RG, Gibbons LE, McCurry SM, Teri L (2002) Assessing quality of life in older adults with cognitive impairment. Psychosom Med 64: 510-519.
- Bárrios H, Narciso S, Guerreiro M, Maroco J, Logsdon R, et al. (2013) Quality of life in patients with mild cognitive impairment. Aging Ment Health 17: 287-292.
- Li MJ, Black DS, Garland EL (2016) The Applied Mindfulness Process Scale (AMPS): A process measure for evaluating mindfulness-based interventions. Pers Individ Dif 93: 6-15.
- Berg KO, Wood-Dauphinee SL, Williams JI, Maki B (1992) Measuring balance in the elderly: Validation of an instrument. Can J Pub Health 83: S7-11
- Romero S, Bishop MD, Velozo CA, Light K (2011) Minimum detectable change of the berg balance scale and dynamic gait index in older persons at risk for falling. J Geriatr Phys Ther 34: 131-137.
- Buatois S, Miljkovic D, Manckoundia P,Gueguen R, Miget P, et al. (2008) Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J Am Geriatr Soc 56: 1575-1577.
- Mong Y, Teo TW, Ng SS (2010) 5-repetition sit-to-stand test in subjects with chronic stroke: Reliability and validity. Arch Phys Med Rehabil 91: 407-413.
- Nordin E, Rosendahl E, Lundin-Olsson L (2006) Timed "Up & Go" test: Reliability in older people dependent in activities of daily living--focus on cognitive state. Phys Ther 86: 646-655.
- Podsiadlo D, Richardson S (1991) The timed "Up & Go": A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39: 142-148.
- Dye DC, Eakman AM, Bolton KM (2013) Assessing the validity of the dynamic gait index in a balance disorders clinic: An application of Rasch analysis. Phys Ther 93: 809-818.
- Pardasaney PK, Latham NK, Jette AM, Wagenaar RC, Ni P, et al. (2012) Sensitivity to change and responsiveness of four balance measures for community-dwelling older adults. Phys Ther 92: 388-397.
- Wilkins CH, Roe CM, Morris JC (2010) A brief clinical tool to assess physical function: The mini-physical performance test. Arch Gerontol Geriatr 50: 96-100.
- Jorgensen AW, Lundstrom LH, Wetterslev J, Astrup A, Gotzsche PC (2014) Comparison of results from different imputation techniques for missing data from an anti-obesity drug trial. PLoS One 9: e111964.
- Del Re AC, Maisel NC, Blodgett JC, Finney JW (2013) Intention-to-treat analyses and missing data approaches in pharmacotherapy trials for alcohol use disorders. BMJ Open 3: e003464.
- Molnar FJ, Hing MMS, Hutton B, Fergusson DA (2009) Have last-observation-carried-forward analyses caused us to favour more toxic dementia therapies over less toxic alternatives? A systematic review. Open Med 3: e31-50.
- Dossing A, Tarp S, Furst DE, Gluud C, Bejene J, et al. (2014) Interpreting trial results following use of different intention-to-treat approaches for preventing attrition bias: A meta-epidemiological study protocol. BMJ Open 4: e005297.
- Tolea MI, Galvin JE (2016) The relationship between mobility dysfunction staging and global cognitive performance. Alz Dis Assoc Disord 30: 230-236.
- Tolea MI, Morris JC, Galvin JE (2016) Trajectory of mobility decline by type of dementia. Alzheimer Dis Assoc Disord 30: 60-66.
- Tolea MI, Morris JC, Galvin JE (2015) Longitudinal associations between physical and cognitive performance among community-dwelling older adults. PLoS One 10: e0122878.
- Juan YH, Livneh H, Huang HJ, Lu MC, Yeh CC, et al. (2019) Decreased risk of dementia among patients with traumatic brain injury receiving acupuncture treatment: A population-based retrospective cohort study. J Head Trauma Rehabil 34: E17-E23.
- Lanza G, Centonze SS, Destro G, Vella V, Bellomo M, et al. (2018) Shiatsu as an adjuvant therapy for depression in patients with Alzheimer's disease: A pilot study. Complement Ther Med 38: 74-78.
- Dossing A, Tarp S, Furst DE, Gluud C, Wells GA, et al. (2016) Modified intention-to-treat analysis did not bias trial results. J Clin Epidemiol 72: 66-74.
Citation: Willcox T, Rosenfeld A, Tolea MI, Galvin JE (2019) The Effects of Acupuncture on Mild Cognitive Impairment: A Pilot Study. J Alzheimers Dis Parkinsonism 9:479. DOI: 10.4172/2161-0460.1000479
Copyright: © 2019 Willcox T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3931
- [From(publication date): 0-2019 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 3044
- PDF downloads: 887