The Importance of Oral Health during Pregnancy for Preventing Gingivitis: A Case Report
Received: 19-Feb-2022 / Manuscript No. johh-22-55006 / Editor assigned: 22-Feb-2022 / PreQC No. johh-22-55006 (PQ) / Reviewed: 08-Mar-2022 / QC No. johh-22-55006 / Revised: 14-Mar-2022 / Manuscript No. johh-22-55006 (R) / Accepted Date: 14-Mar-2022 / Published Date: 21-Mar-2022 DOI: 10.4172/2332-0702.1000304
Abstract
Pregnancy is a transient physiological condition which brings about different changes in all parts of woman’s body.
These complex physiological changes can affect woman oral health and compromise that of the unborn child: the maintenance of optimal conditions of the oral cavity of the woman is crucial for the best outcome of pregnancy and for the promotion of the oral health of the unborn child.
Keywords: Oral Health; Oral Health Education; Pregnancy
Keywords
Oral Health; Oral Health Education; Pregnancy
Introduction
In recent decades, many studies have shown the association between maternal oral infections and adverse pregnancy outcomes.
Existing scientific evidence emphasizes the association between the presence and severity of gum infections and premature birth, fetal growth retardation, spontaneous abortion, preeclampsia. The role of these infections as a possible risk factor or co-cause of adverse pregnancy outcomes has not, however, always been confirmed while the possibility of vertical transmission, from mother to child, of bacteria that cause tooth decay has been demonstrated. Gingival bleeding often causes the pregnant woman to decrease the brushing of teeth resulting in greater accumulation of bacterial plaque and further impairment of the general state [1].
Dietary and oral hygiene changes, morning gravidic hyperemesis, esophageal reflux disease can cause tooth tissue demineralization with enamel erosion and increase the risk of tooth decay if appropriate preventive interventions are not planned [2].
Case Report
A 33-year-old woman, 3-month pregnancy, gravidic gingivitis, no systemic pathologies.
What she referred
Pain in the gums, gums that bleed when brushing, swollen, tense gums, easily traumatizable, high estrogen levels, hyper emesis gravid arum [3-5].
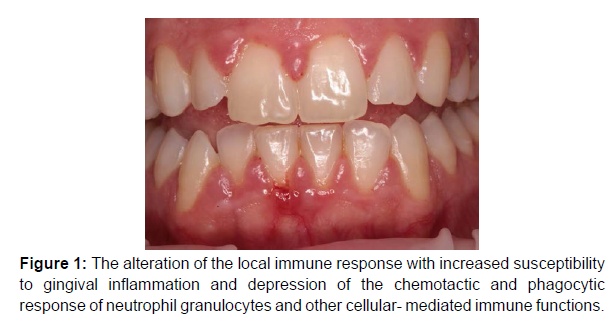
During the objective examination we find what the patient said the alteration of the local immune response with increased susceptibility to gingival inflammation and depression of the chemotactic and phagocytic response of neutrophil granulocytes and other cellularmediated immune functions (Figure 1).
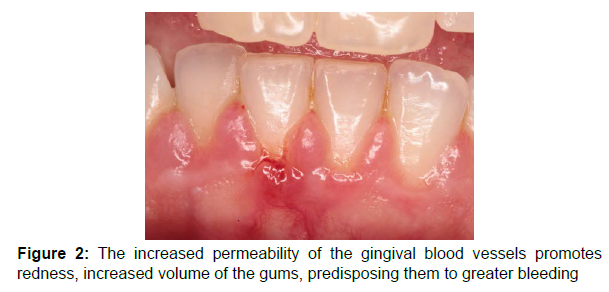
The increased permeability of the gingival blood vessels promotes redness, increased volume of the gums, predisposing them to greater bleeding (Figure 2).
Professional treatment
She received perinatale care with a periodontal treatment.
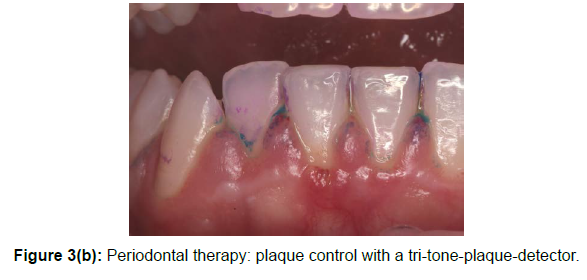
Periodontal therapy consisted of plaque control with a tri-toneplaque- detector, removing with airflow and scaling (Figure 3(a, b)).
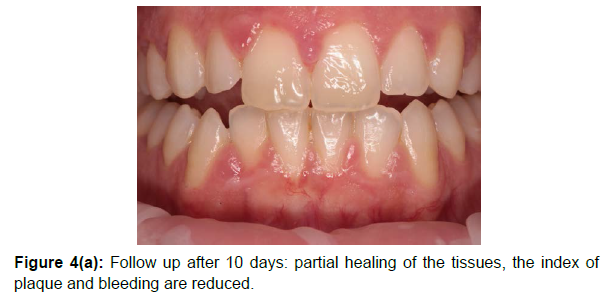
Maintenance therapy was provided every to 10 days for 1month, and consisted of oral hygiene instruction and supragingival plaque removal by instrumentation, as needed (Figure 4a, 4b).
After the first oral hygiene session we obtained a partial healing of the tissues. The index of plaque and bleeding are reduced.
The teaching and reinforcement of the information of personal oral hygiene techniques have contributed to obtaining excellent results already at the first follow-up after 10 days.
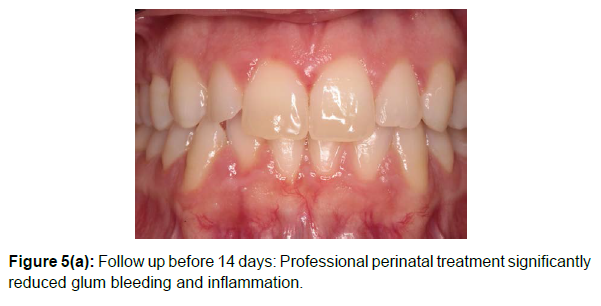
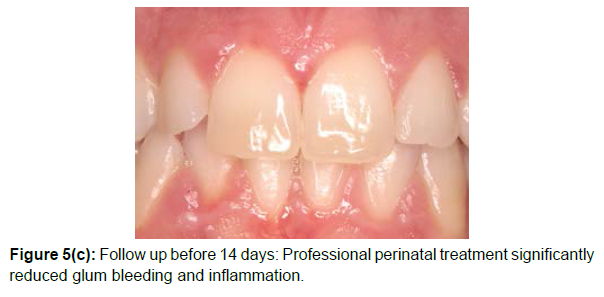
Follow-up 14 days
We have made dietary changes that have led to the disappearance of gravidic hyperemesis (Figure 5(a-c)). Reduction of: plaque and bleeding index, gum edema, gums pain [6].
Professional perinatal treatment significantly reduced glum bleeding and inflammation.
Conclusion
Dental procedures during pregnancy are safe and necessary: every pregnant woman should be assessed for dental hygiene habits and oral problems. The maintenance of optimal conditions of the oral cavity of the woman is crucial for the best outcome of pregnancy. Good oral hygiene, brush twice a day and floss once a day, good nutrition, regular visits to the dental hygienist can prevent gingivitis in early stages.
Conflict of Interest
We declare that we have no conflict of interest.
References
- Bobetsis YA, Barros SP, Offenbacher S (2006) Exploring the relationship between periodontal disease and pregnancy complications. J Am Dent Assoc 137: S7-S13.
- Gajendra S, Kumar JV (2004) Oral health and pregnancy: a review. N Y State Dent J 70(1): 40-44.
- Dye BA, Vargas CM, Lee JJ, Magder L, Tinanoff N (2011) Assessing the relationship between children's oral health status and that of their mothers. J Am Dent Assoc 142(2): 173-183.
- Albert DA, Begg MD, Andrews H F, Williams SZ, Ward A, et al. (2011) An examination of periodontal treatment, dental care, and pregnancy outcomes in an insured population in the United States. Am J Public Health 101(1): 151-156.
- Shrout MK, Comer RW, Powell BJ, McCoy BP (1992) Treating the pregnant dental patient: four basic rules addressed. J Am Dent Assoc 123(5): 75-80.
- Calabrese N, Calabrese A, Nibali L, Rosati A, Fiengo S, et al. (2010) Is there any association between periodontitis and preterm low birth weight?. J Matern-Fetal Neonatal Med 23(11): 1288-1293.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Morittu S, Barbieri S, Simonini M (2022) The Importance of Oral Health during Pregnancy for Preventing Gingivitis: A Case Report. J Oral Hyg Health 10: 304. DOI: 10.4172/2332-0702.1000304
Copyright: © 2022 Morittu S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3945
- [From(publication date): 0-2022 - Dec 23, 2025]
- Breakdown by view type
- HTML page views: 3233
- PDF downloads: 712