Translation, Cross - Cultural Adaptation and Validation of English "Mishel Uncertainty Illness Scale - Adult Form" into Bangla
Received: 29-Oct-2020 / Accepted Date: 20-Nov-2020 / Published Date: 27-Nov-2020
Abstract
The aim of the study was to translate and validate the English version of the “Mishel Uncertainty Illness Scale – Adult Form” into Bangla for assessing illness uncertainty in patients with cancer in Bangladesh. Nurses use the scale to promote patient care and improve their knowledge by using this scale. MUIS – A form has 33 items on Likert scale from 1 (strongly disagree) to 5 (strongly agree) points under four dimensions. During analysis item no # 15 was excluded. Researchers first translate the scale into Bangla and back translated into English through translation process. Adaptation and validation of the pre – Bangla version was accomplished through three successive tests; comprehensively, validity and test – retest reliability. Content validity was found excellent 0.06. The reliability coefficient was very good for 32 items was 0.738 after eliminating some items. α=0.263 – 0.701 for its four factors. The consistency of the instrument with three weeks interval was excellent t=0.745. The Bangla version of uncertainty in illness scale had a good validity and reliability and was useful in assessing illness uncertainty in patients with cancer in Bangladesh. Nurses use the scale to promote patient care and improve their knowledge by using this scale.
Keywords: Translation; Cross – cultural adaptation; Validation; Reliability; MUIS – A; Uncertainty
Introduction
Uncertainty in illness can occur in conditions that are acute and chronic [1] defined uncertainty as “the inability to determine the meaning of illness related events” and further stated that “it is the cognitive state when the person cannot adequately structure or categorize an event because of lack of sufficient cues.” Uncertainty occurs in a situation in which the decision maker or patient is unable to assign definite value to objects or events and/or is unable to predict outcomes accurately [2]. Patients suffering from chronic disease such as cancer experience illness uncertainty different from patients with acute illness. In acute illness, patients experience uncertainty at diagnosis but are offered treatment to relieve symptoms and reduce uncertainty. In chronic illnesses like cancer where treatment might not be available or unnecessary, too expensive, delayed, patients must learn to live with continued uncertainty [3].
In 1981, the Mishel Uncertainty Illness Scale (MUIS) was introduced and has undergone rigorous psychometric testing. The MUIS – A form has four factors. These are ambiguity, complexity, inconsistency and unpredictability. Ambiguity is defined as bodily warning about the condition of the illness that are unclear and most of the time they are confused and concern with other illness. Complexity is about treatment and whether or not it will work and the difficulty in understanding health care system. Inconsistency is about repeatedly changing information provided by health care provider and is consistent with previous information. Physical symptoms that changed continuously and make it difficult to predict and compare present illness with previous illness experience [4,5]. The instrument contains 33 items on Likert scale from 1 (strongly disagree) to 5 (strongly agree). The instrument’s scores range between 33 and 165, and higher scores indicate greater uncertainty [6,7].
A scale can be used to measure the benefits of interventions designed to manage uncertainty in patients with cancer. The most frequently and widely used scale is the Mishel Uncertainty in Illness Scale-Adult form (MUIS-A) for adult patients. The scale is a valid and reliable measure that has been used in multiple studies and translates into Italy, Pearsian version [5,8]. No scale was translated, culturally adapted and validated to measure uncertainty among cancer patients in Bangladesh. The objectives of the study were to translate, cross – culturally adapt and validate the English Mishel Uncertainty in Illness Scale- Adult (MUIS) – A form into Bengali and to determine validity and test its reliability.
Materials and Methods
This was a descriptive quantitative type of study conducted from July 2018 to June 2019. Interview schedule was performed at Department of Oncology.
Scale information
Mishel Uncertainty in Illness Scale, Adult (MUIS-A) form has total 33 items. Reverse score items 6, 7, 10, 12, 21, 25, 27, 28, 30, 31, 32, 33. For the four factor analysis, eliminate item #15 and sum the remaining 32 items for a total score and determine the mean. Higher scores indicate greater uncertainty. Ambiguity (mean of items: 3,4,8,9,13,14 ,16,17,18,20,23,24,26) Complexity (mean of items: 6,7,10,28,31,32,33) Inconsistency (mean of items: 1,2,5,11,19,22,29) Unpredictability (mean of items: 12, 21,25,27,30).
Adaptation and validation of the pre – Bengali version
This step was accomplished through three successive tests. Comprehensively, validity and test – retest reliability.
Statistical procedure
These data were checked, verified for consistency and edited for finalized result. After editing and coding, the data were entered into the computer by using SPSS software. Scale internal consistency was measured by Cronbach’s alpha for the total scale and each subscale separately. The reliability was measured by the Maan Whitney test.
Results
Sample characteristics
Participants’ characteristics are depicted in Table 1. The mean age of participants was 47.18 (SD=13.55) years. Most of them were male (52.7%) and married (98.1%) and Muslim (95.2%). According to educational degree, most of participants (46.7%) had primary education, while, 31.5% had obtained secondary education and only 12.1% participants had completed graduation.
| Characteristics | Category(s) | (%) | M(SD) |
|---|---|---|---|
| Age (years) | < 19 - 40 | 34.7 | 47.18 (13.55) |
| > 40 | 64.7 | ||
| Min = 19 years Max = 75 years | |||
| Sex | Male | 52.7 | - |
| Female | 47.3 | ||
| Marital Status | Married | 98.1 | |
| Unmarried | 9.7 | ||
| Widowed | 1.2 | ||
| Religion | Muslim | 95.2 | |
| Hindu | 4.8 | ||
| Education | Primary | 46.7 | |
| Secondary | 31.5 | ||
| Higher Secondary | 9.7 | ||
| Above | 12.1 | ||
Table 1: Participants characteristics.
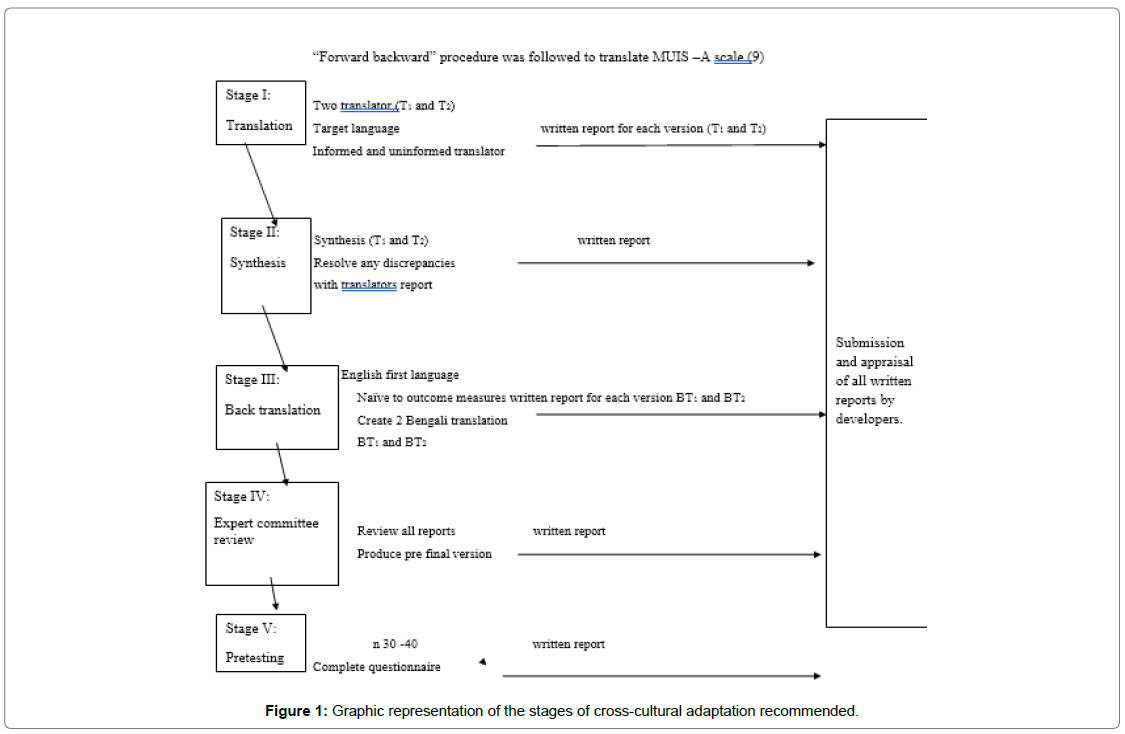
More than Fifty-eight percent (58.2%) of respondents had been diagnosed less than 6 months, while, only 10.3% of respondents had been diagnosed more than 1.5 years. More than ninety three percent (93.8%) of them had no metastasis and only 5.6% had metastasis (Figure 1 and Table 2).
| Characteristics | Category(s) | n | (%) |
|---|---|---|---|
| Time Since Diagnosis | Less than 6 months | 96 | 58.2 |
| 6 months1 day –1year | 40 | 24.2 | |
| 1 year1 day- 1.5 years | 12 | 7.3 | |
| >1.5 years | 17 | 10.3 | |
| Metastasis | Yes | 9 | 5.6 |
| No | 152 | 93.8 |
Table 2: Participants characteristics.
Content validity
In order to examine the content validity index (CVI), the translated scale was given to three experts in the field, a specialist in clinical psychology, a palliative medicine physician and a faculty of a medical college. Two of them rated each item as 1 (agreed), 0 (undermined), or -1 (disagreed). The content validity index was calculated using summation of score from each expert divided by the number of experts. So, CVI was 0.06. [10].
Internal consistency reliability (Cronbach’s Alpha)
The Cronbach’s α for total scale was 0.648. After eliminating items 7, (When I have pain, I know what this means about my condition) 2,(I have a lot of questions without answers)11, (The doctors say things to me that could have many meanings)19, (I have been given many differing opinions about what is wrong with me) and 22 (The results of my tests are inconsistent) the value of the reliability coefficient was satisfactory (Cronbach’s α=0.734).
In this study, the reliability coefficient for ambiguity dimension containing 13 items was not satisfactory (Cronbach’s α=0.611). It achieved the recommended threshold of 0.600. Though by deleting items three, nine, thirteen, fourteen, eighteen and twenty three, the value of the reliability coefficient was satisfactory (Cronbach’s α=0.701).
The reliability coefficient, calculated for the complexity dimension containing seven items was not also satisfactory (Cronbach’s α=0.526). After deleting item six, the value of the reliability coefficient improved and achieve the recommended threshold of 0.600, Cronbach’s α=0.620 [5].
In this study, inconsistency dimension exhibited was very low (Cronbach’s α=0.263). The low value of the Cronbach’s a (0.500), calculated for the original five-item unpredictability dimension, after eliminating items 12 ,21 and 30, the value of the Cronbach’s alpha was improved (a=0.601).
We checked reliability of the MUIS among cancer patients between 3 weeks interval. The result showed that uncertainty in illness scale was internally very consistent. This result was not statistically significant (Table 3).
| Variable | Category | Mean Rank | t | p |
|---|---|---|---|---|
| Uncertainty in Illness | Test | 21.1 | 0.745 | 0.325 |
| Retest | 19.9 |
Table 3: Uncertainty in illness.
Discussion
Illness uncertainty is a concept that resonates with patients diagnosed and living with cancer and was evident this group of patients in Bangladesh. Though it was important in Bangladesh, there was no tool to measure uncertainty in illness, especially for patients with cancer. Therefore, the aim of the study was to translate and validate the MUIS - A into Bangla among patients with cancer.
In this study, the MUIS-A scale was translated into Bangla and cheeked its cross cultural adaptation and validation. When a tool is translated or used in another culture or society, it is essential to evaluate its cross cultural adaptation and validation because that may not be appropriate in the new society [11]. In this study, cross cultural adaptation, content validity, internal consistency reliability and testretest reliability of this tool were assessed. Based on the findings, the Bangla version of MUIS-A generally is a good scale. Other studies also showed the same results [3,6,10]. This tool has been translated in to a least 12 other languages reflective of the global experience of illness uncertainty among people living with chronic conditions [12,13].
Conclusion
This study demonstrated that the Bengali version of the MUIS - A had established validity and reliability. Therefore, it is applicable to assess uncertainty in illness among patients with cancer in Bangladesh. Nurses can use the tool to assess illness uncertainty in their patients’ care and seek to identify interventions to help them manage their uncertainty. A limitation of the present study was the use of an interview schedule to complete the questionnaire. In Bangladesh, patients were not accustomed to completing questionnaires by themselves. This study will support the future study of assessment and intervention of uncertainty among cancer patients in Bangladesh.
Acknowledgement
This research project was supported by a grant from University Grant Commission through Bangabandhu Sheikh Mujib Medical University, Dhaka.
References
- Mishel MH (1988) Uncertainty in illness. The Journal of Nursing Scholarship 20: 225-232.
- Lin L, Yeh CH, Mishel MH (2010) Evaluation of a conceptual model based on Mishel’s theories of uncertainty in illness in a sample of Taiwanese parents of children with cancer: A cross-sectional questionnaire survey. Int J Nurs Stud 47: 1510-1524.
- Baresari ZB, Abbaszadeh A, Heydarirad G, Khabazkhoob M (2018) The psychometrics of the Persian version of the “cancer fatigue scale†in Iran. EurAsian J Biosci 12: 149-156.
- Bailey DE, Landerman L, Barroso J, Bixby P, Mishel MH, et al. (2009) Uncertainty, symptoms, and quality of life in persons with chronic Hepatitis C. Psychosomatics 50: 138-146.
- Giammanco MD, Gitto L, Barberis N, Santoro D (2015). Adaptation of the M ishel Uncertainty of Illness Scale (MUIS) for chronic patients in Italy. Journal of Evaluation in Clinical Practice 21(4): 649-655.
- Byun E (2013) Effects of uncertainty on perceived and physiological stress and psychological outcomes in stroke-survivor caregivers. University of Pennsylvania.
- Vera N (2009) The relationship between uncertainty in illness and anxiety in patients with cancer.
- Garofalo JP, Choppala S, Hamann HA, Gjerde J (2009) Uncertainty during the transition from cancer patient to survivor. Cancer Nurs 32: E8–14.
- Beaton D, Bombardier C, Guillemin F, Ferraz MB (2007) Recommendations for the cross-cultural adaptation of the DASH & QuickDASH outcome measures.
- DeVon HA, Block ME, Moyle-Wright P, Ernst DM, Hayden SJ, et al. (2007) A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh 39: 155-164.
- Hillen MA, Butow PN, Tattersall MHN, Hruby G, Boyle FM, et al. (2013) Validation of the English version of the trust in oncologist scale (TiOS). Patient Educ Couns 91: 25-28.
- Germino BB, Mishel MH, Crandell J, Porter L, Blyler D, et al. (2013) Outcomes of an uncertainty management intervention in younger african american and caucasian breast cancer survivors. Oncol Nurs Forum 40: 11.
- Kearney MH (2017) The discussion section tells us where we are. Res Nurs Health 40: 289-291.
Citation: Khatun Z, Bailey DE, Ahmad N (2020) Translation, Cross - Cultural Adaptation and Validation of English “Mishel Uncertainty Illness Scale - Adult Form” into Bangla. J Palliat Care Med 10: 383.
Copyright: © 2020 Khatun Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
9th World Conference on Nursing Education & Nursing Practice
Toronto, Canada
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Usage
- Total views: 1601
- [From(publication date): 0-2020 - Sep 21, 2024]
- Breakdown by view type
- HTML page views: 941
- PDF downloads: 660