Treatment of Trigeminal Neuralgia by Relieving the Posterior Cervical Muscle Stiffness with Parietal Acupoint Therapy: Case Reports
Received: 17-Oct-2018 / Accepted Date: 29-Nov-2018 / Published Date: 03-Dec-2018 DOI: 10.4172/2167-0846.1000331
Abstract
Introduction: Trigeminal neuralgia is sudden-onset, sharp, stabbing, and recurrent pain that is provoked by trigger factors within the distributed branch area of the trigeminal nerve. Although surgical intervention, which primarily comprises micro vascular decompression (MVD), and medication are mainstream treatment options to relieve pain, the indication and efficacy of these approaches depend on each case. Recently, tenderness in the greater occipital nerve area in patients with craniofacial pain has been reported, indicating a vital role of nociceptive afferents with the involvement of trigeminal branches through the trigeminocervical complex (TCC). Here, we present two improved cases of trigeminal neuralgia with parietal acupoint therapy (PAPT) by treating the muscle stiffness of the posterior cervical region.
Case Reports: In Case 1, a 64-year-old female who presented with right typical trigeminal neuralgia symptom with posterior cervical muscle stiffness and occipital numbness on the same side. Remarkably, her pain was triggered by head flexion. The unusually dilated greater occipital artery was suspected to be associated with the greater occipital nerve (GON) stimulation, resulting in the exacerbation of pain during head flexion. The pain was effectively controlled with parietal acupoint therapy and occipital nerve block (ONB). In Case 2, a 63-year-old female presented with trigeminal neuralgia after dental treatment with the posterior cervical muscle stiffness. Three cycles of PAPT performed once a week completely relieved her muscle stiffness and trigeminal pain without medication.
Conclusions: The nociceptive stimuli from the posterior cervical region are vital contributory factors to initiate trigeminal neuralgia. This report reveals that relieving the posterior cervical muscle stiffness by parietal acupoint therapy for the treatment of trigeminal neuralgia is effective. Hence, this noninvasive treatment for trigeminal neuralgia should be considered before prescribing medication or performing surgical interventions.
Keywords: Trigeminal neuralgia; Posterior cervical stiffness; Nociceptive stimuli; Trigeminocervical complex; Parietal acupoint therapy
Introduction
Trigeminal neuralgia is sudden-onset, sharp, stabbing, and recurrent pain that is provoked by trigger factors within the distributed branch area of the trigeminal nerve. Regarding the pathophysiology, the neurovascular contact is widely accepted as the primary cause of classical trigeminal neuralgia. Hence, microvascular decompression (MVD) is acknowledged as more superior to other treatment regarding evidence with immediate and continuous pain relief [1,2]. However, a recent study on patients with classical trigeminal neuralgia reported no significant difference of existence on neurovascular compression between the symptomatic and asymptomatic sides, 81% versus 70%, respectively [3]. Accordingly, regarding the treatment of trigeminal neuralgia, the surgical approach is selected with discretion, and other treatment options including medications, such as carbamazepine, topiramate, lamotrigine, and other anticonvulsants, are considered as the other options. Recently, beneficial reports that patients with a primary headache rely on the neck pain and restricted rotation, indicating an implication of the cervical musculoskeletal system, have increased [4-6]. Likewise, we have often experienced that patients with craniofacial pain, not only migraine and tension-type headache, but also trigeminal neuralgia are accompanied by neck pain or stiffness. In apparent work regarding the occipital nerve block (ONB) treatment for the craniofacial pain, the existence of tenderness at the GON area in patients and the efficacy for ONB have been indicated, suggesting a vital role of nociceptive afferents from the posterior cervical region through the trigeminocervical complex (TCC), which results in hyperactivity with trigeminal branches [7]. Moreover, some reports revealed that effective treatment options in the cervical spine region are manual therapy [8] and chiropractic [9] for pain relief of trigeminal neuralgia.
Parietal acupoint therapy (PAPT), which we reported earlier, is scalp acupuncture using the somatotopic representative microsystem that displays the entire body anatomically and functionally and can relieve symptoms immediately and effectively using acupoints corresponding to the areas in which patients complain of pain or stiffness [10]. Here, we report two cases of treated trigeminal neuralgia by relieving the posterior cervical muscle stiffness with PAPT.
Case Reports
Case 1
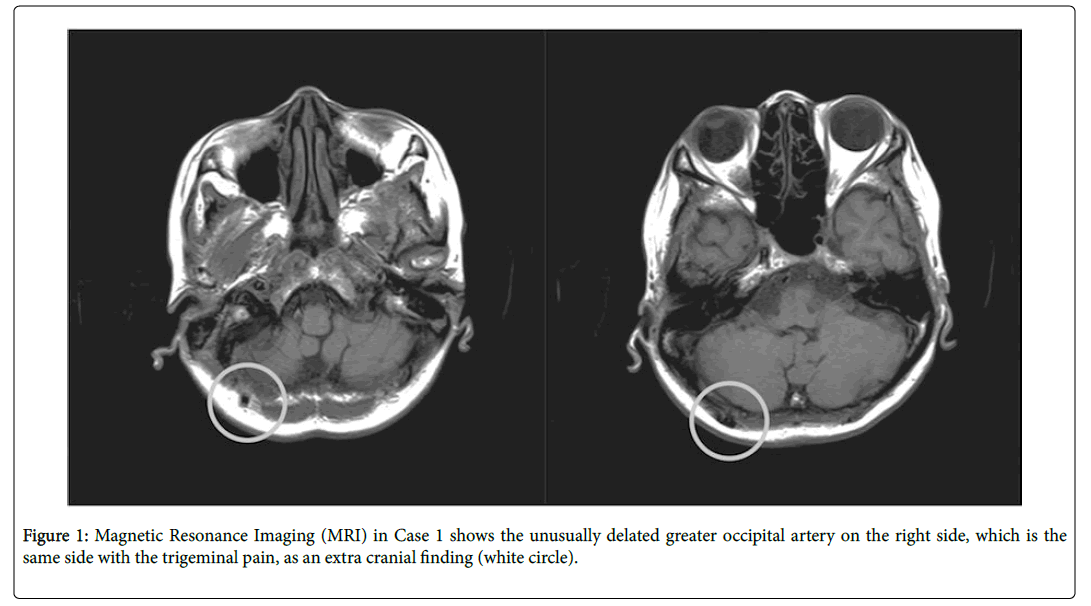
A 64-year-old female was diagnosed with typical trigeminal neuralgia in the right maxillary (V2) area 2 years ago in another hospital. Accordingly, carbamazepine, an anticonvulsant, was prescribed as Magnetic Resonance Imaging (MRI)/Magnetic Resonance Angiography (MRA) detected no intracranial abnormality, such as brain tumor or vascular malformation, and no apparent vascular contact on the trigeminal nerve. Although carbamazepine (200 mg per day) remained effective for 1.5 years, her pain recurred and became frequent on a daily basis. She visited our hospital complaining of sharp and intermittent pain in the right maxillary (V2) area, accompanied by posterior cervical muscle stiffness and occipital numbness on the same side. Notably, trigger points on the right upper trapezius and splenius capitis muscle were detected. Remarkably, the trigeminal pain triggered with head flexion. MRI/MRA revealed no intracranial abnormality, except for unusually dilated greater occipital artery on the right side as an extracranial finding (Figure 1).
Accordingly, we initiated PAPT using parietal cervical (PC) points to release the posterior cervical muscle stiffness on the first day she visited. We inserted 5-7 sterilized disposable needles (J-Type 0.25 mm-30 mm; SEIRIN Co., Japan) into palpated points at a depth of 10-15 mm on PC3 to PC6 areas. The patient was kept in a sitting position and rested for 30 min after therapy. Immediately after the first PAPT procedure, the posterior cervical muscle stiffness relieved and the patient’s sharp pain on the right maxillary region vanished, except for a blunt sense on the right maxillary region during the head flexion. We considered the unusually dilated greater occipital artery was held accountable for the GON stimulus; hence, ONB using 5 cc of 0.5% levobupivacaine hydrochloride was selected as the second approach in 2 weeks after first PAPT. ONB effectively alleviated her remaining symptom. Each of those treatments has been performed once a week. After those treatment for 2 months, her symptoms were wellcontrolled by only taking 200 mg of carbamazepine per day, as same as before her symptoms has been worse.
Case 2
A 63-year-old female had trigeminal neuralgia on the left side after dental treatment for years. She exhibited no abnormal evidence on the dental treatment region. She has been taking clonazepam, an anticonvulsant, as prescribed for a half year. During her first visit to our hospital, she complained of pain in the left maxillary (V2) area triggered with a light touch. In addition, the posterior cervical muscle stiffness with trigger points on the left upper trapezius and splenius capitis muscle was detected. Similar to Case 1, we performed PAPT using PC points for the posterior cervical muscle stiffness. After three cycles of the procedure performed once a week, the patient’s trigeminal pain was relieved entirely without medication.
Discussion
To the best of our knowledge, this is the first report of treating trigeminal pain by relieving the posterior cervical muscle stiffness with scalp acupuncture. In both cases, PAPT targeting the posterior cervical region alleviated not only the neck stiffness with the disappearance of trigger points on the upper trapezius and splenius capitis muscle but also the trigeminal pain on the maxillary (V2) area. In our experience, it is not rare to confirm the cervical musculoskeletal impairment, such as muscle pain and stiff and restricted rotation, in the posterior cervical region in patients with trigeminal neuralgia. Regarding the mechanism underlying the occurrence of coexisting events, the potential for the convergence of sensory input from the upper three cervical segments and the trigeminal nerve through the trigeminocervical nucleus has been discussed. Reportedly, the TCC is formed such that afferent nerves from the trigeminal and occipital (C1-3) nerve branches are projected in the trigeminal cervical nucleus [11,12].
In Case 1, as the blunt sense on the right maxillary region persisted during head flexion after PAPT, ONB was performed by an anesthesiologist because of the suspicion that unusually dilated greater occipital artery was affecting the GON, resulting in the exacerbation of stimuli during head flexion. Besides the pain in the frontal region innervated by the ophthalmic (V1) area of the trigeminal nerve, the pain in the occipital region innervated by the GON is often reported. In addition, regarding the treatment of trigeminal neuralgia with the involvement of the second and third (V2 and V3) trigeminal branches, the efficacy of ONB has also been established [13]. Although certain mechanisms underlying the efficacy remain unclear, it is suggested that ONB results in the inhibition on the GON and extracranial collaterals of the maxillary and mandibular nerve activities [14], leading to the improved nociceptive afferent stimuli.
In Case 2, despite the absence of any problem in the dental treatment, the trigeminal pain occurred soon after the treatment. Notably, such events have often been reported earlier. Shinozaki et al. compared the attitude of pain relief on the orofacial pain, by a local anesthetic injection around the painful orofacial region, at the muscle trigger points and the deep cervical plexus block in eight patients with orofacial pain with neck symptoms; the authors asserted that the deep cervical plexus block was the most effective, inferring that certain types of orofacial pain originate from cervical structures [15].
In other clinical findings, local anesthetic injections into the cervical muscle could potentially decrease the orofacial pain intensity besides decreasing the cervical muscle pain [16]. According to the anatomical findings in the cervical trigeminal nucleus, studies considered that the first branch of the trigeminal nerve was extensively projected into the C1-C3 cervical spinal region. Conversely, projections of the second and third branches of the trigeminal nerve to the cervical level were relatively less [17,18]. Thus, cervical muscular impairment has been considered unlikely to contribute to the referred pain associated with the maxillary (V2) and mandibular (V3) areas. However, both cases in this study exhibited improved trigeminal pain in the maxillary region by relieving the posterior cervical muscle stiffness.
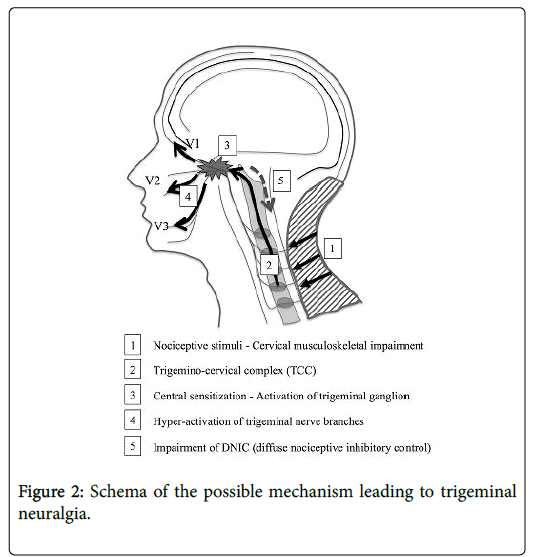
The nociceptive impulses from the periphery, including muscles, dura, and joints on the cervical region could be accountable for the sensitization of second- and third-order neurons in the central nervous system and continuous afferent input lead to the sensitization in the TCC resulting in the initiation of trigeminal neuralgia, even in the maxillary (V2) and mandibular (V3) areas. Thus, cervical musculoskeletal impairment should be considered a potential factor to lead to the enhanced activation of nociceptive pathways, contributing to the development of trigeminal pain. Regarding the mechanism underlying the TCC-associated trigeminal pain, not only nociceptive stimuli, which was mentioned previously, but also diffuse nociceptive inhibitory control (DNIC) should be discussed.
In a case report with a migraine, Piovesan et al. reported that the attack intensity decreased by massaging the GON territory; the authors asserted the contribution of both nociceptive stimuli from the peripheral input and impairment of DNIC on association with the pain intensity [19]. In fact, studies have highlighted which factors are closely associated with the mechanism of the analgesic effect of acupuncture and DNIC [20]. In our previous study, PAPT treatment using the PC points was effective for not only neck/shoulder stiffness but also pain relief. Figure 2 presents the mechanism underlying the trigeminal pain. Nociceptive stimuli from the cervical musculoskeletal impairment activate the trigeminal ganglion through the TCC, resulting in the subsequent hyperactivity on trigeminal distal nerve branches. Under similar conditions, DNIC is impaired resulting in the increased pain sensitivity. The treatment of PC points by PAPT might contribute toward both the reduction of main nociceptive stimuli because of the cervical musculoskeletal impairment and improve the DNIC impairment directly.
In conclusion, the nociceptive stimuli from the posterior cervical region are essential contributory factors to initiate trigeminal neuralgia. This report reveals that relieving the posterior cervical muscle stiffness by PAPT for the treatment of trigeminal neuralgia is effective. Hence, this noninvasive treatment for trigeminal neuralgia should be considered before prescribing medication or performing surgical interventions.
Ethics Approval And Consent To Participate
The study was approved by the ethics committee of JCHO Yokohama Central Hospital (Reference number: 2018-2019). All enrolled patients provided a written informed consent to participate in the study.
Consent for Publication
Written informed consent was obtained from the patients for publication of this case report and accompanying images. Additionally, patient privacy, particularly the name, date of birth, date of medical treatment, place of birth and residence, family name, and photographs of patients, has been maintained. Other identifying information (previous medical doctor, relevant medical institution ID, and clinical examinations and corresponding data) have not been stated.
The first author is responsible for managing and ensuring the confidentiality of patient data and personal information. Copies of explanation documents concerning the “case report” and consent forms have been provided to the patients.
Availability of Data and Material
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Funding
Not applicable.
Acknowledgments
The authors would like to thank Enago (www.enago.jp) for the English language review.
References
- Pagni CA, Fariselli L, Zeme S (2008) Trigeminal neuralgia. Non-invasive techniques versus microvascular decompression. It is really available any further improvement? Acta Neurochir Suppl 101: 27-33.
- Barker FG II, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD (1996) The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med 334: 1077-1083.
- Maarbjerg S, Wolfram F, Gozalov A, Olesen J, Bendtsen L (2015) Significance of neurovascular contact in classical trigeminal neuralgia. Brain 138: 311-319.
- Carvalho GF, Chaves TC, Gonçalves MC, Florencio LL, Braz CA, et al. (2014) Comparison between neck pain disability and cervical range of motion in patients with episodic and chronic migraine: A cross-sectional study. J Manipulative Physiol Ther 37: 641-646.
- Ashina S, Bendtsen L, Lyngberg AC, Lipton RB, Hajiyeva N, et al. (2015) Prevalence of neck pain in migraine and tension-type headache: A population study. Cephalagia 35: 211-219.
- Ferracini GN, Florencio LL, Dach F, Bevilaqua Grossi D, Palacios-Ceña M, et al. (2017) Musculoskeletal disorders of the upper cervical spine in women with episodic or chronic migraine. Eur J Phys Rehabil Med 53: 342-350.
- Jürgens TP, Müller P, Seedorf H, Regelsberger J, May A (2012) Occipital nerve block is effective in craniofacial neuralgias but not in idiopathic persistent facial pain. J Headache Pain 13: 199-213.
- Grgić V (2010) Influence of manual therapy of cervical spine on typical trigeminal neuralgia: A case report. Lijec Vjesn 132: 21-24.
- Rodine RJ, Aker P (2010) Trigeminal neuralgia and chiropractic care: A case report. J Can Chiropr Assoc 54: 177-186.
- Aoyama N, Fujii O, Yamamoto T (2017) Efficacy of parietal acupoint therapy: Scalp acupuncture for neck/shoulder stiffness with related mood disturbance. Med Acupunct 29: 383-389.
- Shigenaga Y, Okamoto T, Nishimori T, Suemune S, Nasution ID, et al. (1986) Oral and facial representation in the trigeminal principal and rostral spinal nuclei of the cat. J Comp Neurol 244: 1-18.
- Marfurt CF, Rajchert DM (1991) Trigeminal primary afferent projections to ‘‘non-trigeminal’’ areas of the rat central nervous system. J Comp Neurol 303: 489-511.
- Jürgens TP, Müller P, Seedorf H, Regelsberger J, May A (2012) Occipital nerve block is effective in craniofacial neuralgias but not in idiopathic persistent facial pain. J Headache Pain 13: 199-213.
- Schüler M, Messlinger K, Neuhuber W, De Col R (2011) Comparative anatomy of the trigeminal nerve fibres in the middle cranial fossa and their extracranial projections in rats and humans. Cephalalgia 31: 41-42.
- Shinozaki T, Sakamoto E, Shiiba S, Ichikawa F, Arakawa Y, et al. (2006) Cervical plexus block helps in diagnosis of orofacial pain originating from cervical structures. Tohoku J Exp Med 210: 41-47.
- Mellick LB, Mellick GA (2008) Treatment of acute orofacial pain with lower cervical intramuscular bupivacaine injections: A 1-year retrospective review of 114 patients. J Orofac Pain 22: 57-64.
- Bogduk N (1983) The anatomy and mechanism of cervical headaches. Proceedings of cervical headache symposium.
- Bogduk N (1989) The anatomy of headache. Proceedings of headache and face pain symposium.
- Piovesan EJ, Di Stani F, KowacsPA, Mulinari RA, Radunz VH, et al. (2007) Massaging over the greater occipital nerve reduces the intensity of migraine attacks: evidence for inhibitory trigemino-cervical convergence mechanisms. Arq Neuropsiquiatr 65: 599-604.
- Bing Z, Villanueva L, Le Bars D (1990) Acupuncture and diffuse noxious inhibitory controls: Naloxone-reversible depression of activities of trigeminal convergent neurons. Neuroscience 37: 809-818.
Citation: Aoyama N, Kubota N, Fujii O (2018) Treatment of Trigeminal Neuralgia by Relieving the Posterior Cervical Muscle Stiffness with Parietal Acupoint Therapy: Case Reports. J Pain Relief 7: 331. DOI: 10.4172/2167-0846.1000331
Copyright: © 2018 Aoyama N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6579
- [From(publication date): 0-2018 - Nov 15, 2025]
- Breakdown by view type
- HTML page views: 5622
- PDF downloads: 957