Two Cases of Advanced Malignant Melanoma Occurring from the Esophagus
DOI: 10.4172/aot.s2.1000001
Abstract
We made a diagnosis as a malignant melanoma and conducted esophagectomy. She had DAC-Tam as a palliative chemotherapy after detecting recurrence. But she had wasted away and died within 14 months being diagnosed with her disease. Histological findings revealed malignant melanoma arise from esophagus with liver metastasis. She had nivolumab as first line therapy and ipilimumab subsequently, but she had wasted away and died within 6 months being diagnosed with her disease. Esophageal melanoma was very rare disease. Development of immune-check inhibitor and molecular targeting therapy changed the prognosis for patients.
Case-1
A 57-year-old woman was admitted with a complaint of fatigue and anemia (serum hemoglobin, 5.6 g/dl). We detected an irregular tumor 4 cm in diameter in the lower esophagus, using an upper endoscopic test; melanosis was detected near the tumor. An esophageal biopsy revealed large tumor cells possessing minimal cytoplasm and hyperchromatic indistinct nucleoli based on Hematoxylin and Eosin (HE) staining. We performed esophagectomy and the final staging, on histopathological examination, was IIIA (UICC-6). She was administered DAV-Feron (DTIC, ACNU, VCR and Interferonβ) as adjuvant chemotherapy. However, she was diagnosed with recurrence of the melanoma in the peritoneum in March 2010. We initiated DAM-Tam (DTIC, ACNU, CDDP and tamoxifen) as palliative chemotherapy. She had grade 3 neutropenia and grade 2 fatigues, but these adverse events were controlled to reduce dose settings. She progressively weakened and died within 14 months of being diagnosed with the disease.
Case-2
A 67-year-old woman visited complaining of fatigue. A type 1 tumor with blue pigment deposition in the lower esophagus was detected on upper endoscopy and liver metastasis was observed using Positron Emission Tomography-Computed Tomography (PET-CT). An esophageal biopsy revealed large tumor cells possessing minimal cytoplasm and hyperchromatic indistinct nucleoli based on HE staining. Immunostaining revealed that the tumor cells were positive for S-100 and Melan A, and negative for HMB-45. Histological findings revealed malignant melanoma that had arisen from the esophagus. We initiated nivolumab therapy based on the negative results of the B-RAF V600E mutational test. She exhibited no adverse events after the administration of nivolumab. However, CT revealed progression of the disease within 3 months. We changed to ipillimumab. However, she progressively weakened and died within 6 months of being diagnosed with the disease. Esophageal melanoma was very rare disease. Development of immune-check inhibitor and molecular targeting therapy changed the prognosis for patients.
Keywords: Melanoma; Esophageal cancer; Molecule targeting therapy; Immune-check point inhibitor
Introduction
Esophageal melanoma is a rare occurrence (0.1%-0.2% of malignant esophageal tumors) [1,2]. Malignant melanoma arises from melanocytes and can be classified as mucosal and cutaneous. Mucosal melanomas are rare and account for approximately 1% of all melanomas. They arise primarily in the head and neck, anorectal, and vulvovaginal regions (55%, 24%, and 18% of cases respectively). The esophagus is the rarest site of origin for mucosal melanoma. Treatment of resectable melanoma is based on standard guidelines, and surgical esophagectomy is the only radical curative treatment. Adjuvant therapy after surgery is conducted based on the therapy for cutaneous melanoma. However, the malignant potential is so high that the duration from surgery to recurrence is usually very brief. An anti-cancer medication based on decarbonize for patients with metastasis has been administered for many decades. However, the prognosis of melanoma is poor against that treatment. The response rate is low and the 5-year survival rate has been reported to be less than 5% [2]. In recent years, the developments of both immune checkpoint inhibitors and molecular agents have influenced adjuvant treatment and the treatment for metastatic and recurrent cases. Herein, we report our experience with two cases of metastatic and recurrent melanoma.
Case Report
Case-1
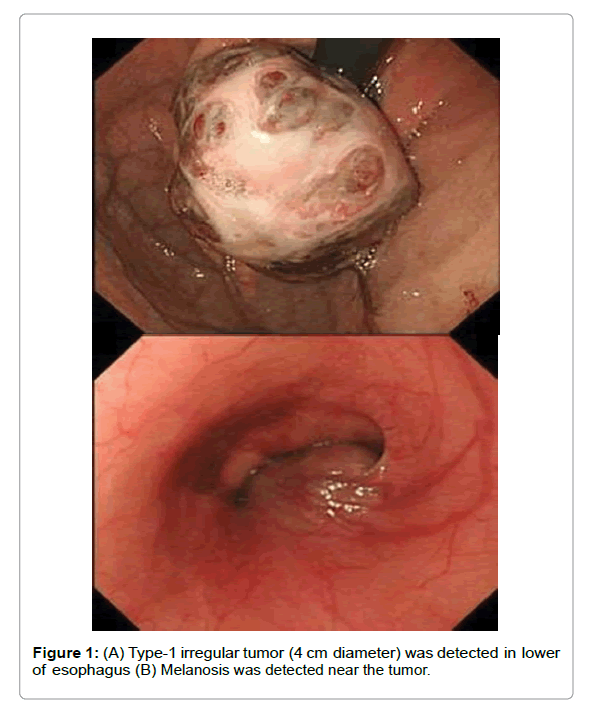
A 57-year-old woman was admitted with a complaint of fatigue and anemia (serum hemoglobin, 5.6 g/dl) on June 2009. We detected an irregular tumor 4 cm in diameter (Figure 1) in the lower esophagus, using an upper endoscopic test; melanosis was detected near the tumor. An esophageal biopsy revealed large tumor cells possessing minimal cytoplasm and hyperchromatic indistinct nucleoli based on Hematoxylin and Eosin (HE) staining. Immunostaining tests revealed that the tumor cells were positive for HMB-45 and Melan A, and negative for S-100. We diagnosed the patient with malignant melanoma (Union for International Cancer Control (UICC) Stage III), based on both pathological and imaging findings. We performed esophagectomy in June 2009 and the final staging, on histopathological examination, was IIIA (UICC-6). She was administered DAV-Feron (80 mg/m2 DTIC on days 1-5, 60 mg/m2 ACNU on day 1, 0.5 mg/m2 VCR on day 1, 3000000 units IFNβ on days 1-5, local injection every 4 weeks) as adjuvant chemotherapy. However, she was diagnosed with recurrence of the melanoma in the peritoneum in March 2010. We initiated DAM- Tam (220 mg/m2 DTIC on days 1-3, 60/m2 ACNU on day 1, 25 mg/ m2 CDDP on days 1-3, 20 mg/body tamoxifen on 1-28 every 4 weeks) as palliative chemotherapy. She had grade 3 neutropenia and grade 2 fatigues, but these adverse events were controlled to reduce dose settings. She progressively weakened and died within 14 months of being diagnosed with the disease.
Case-2
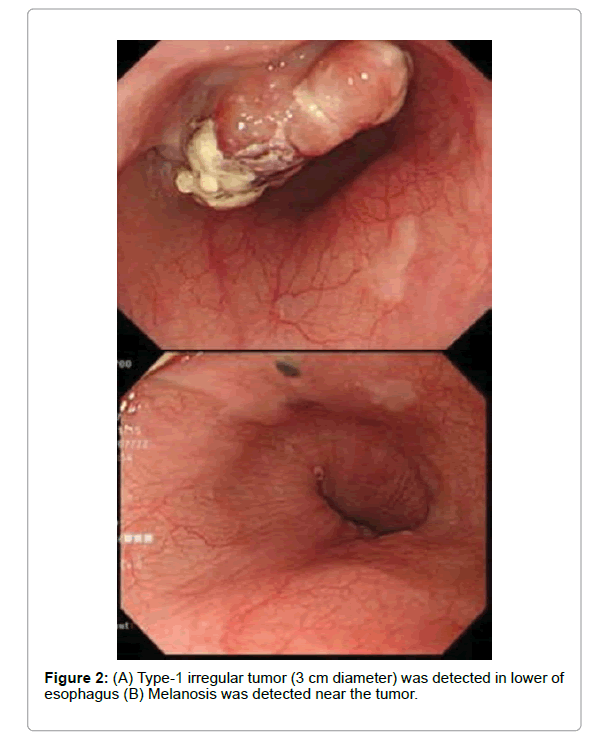
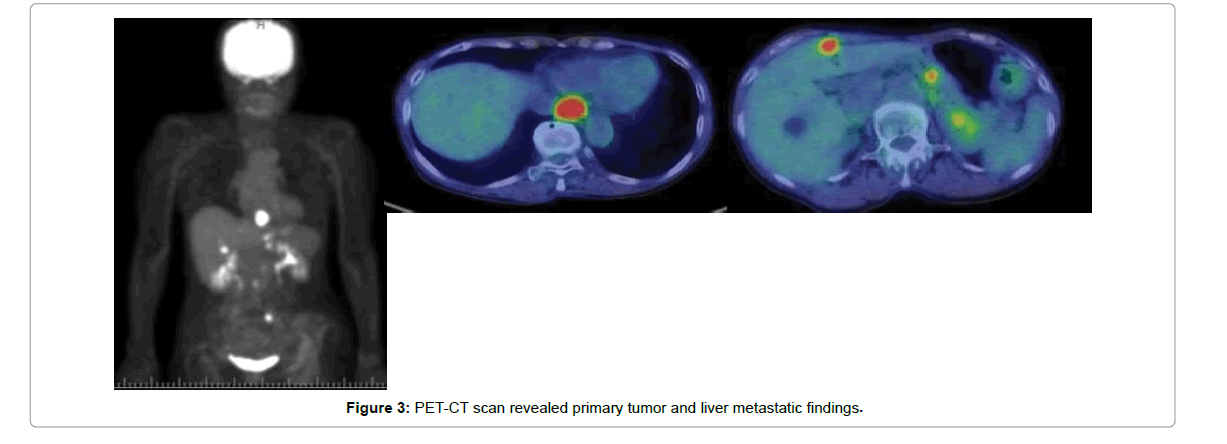
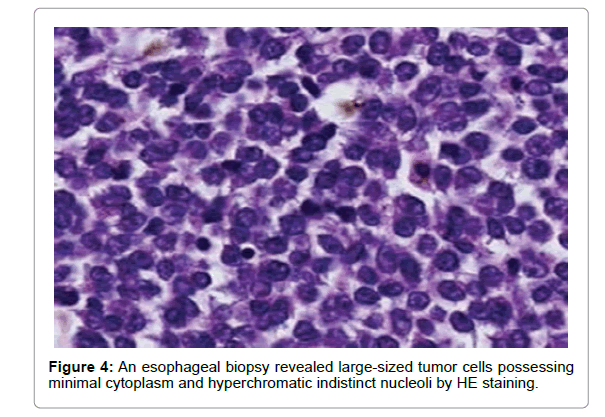
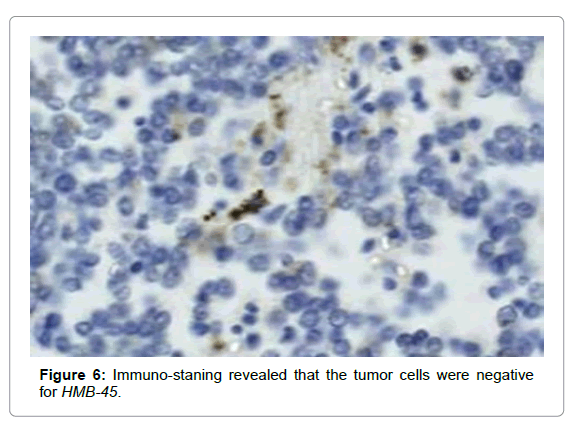
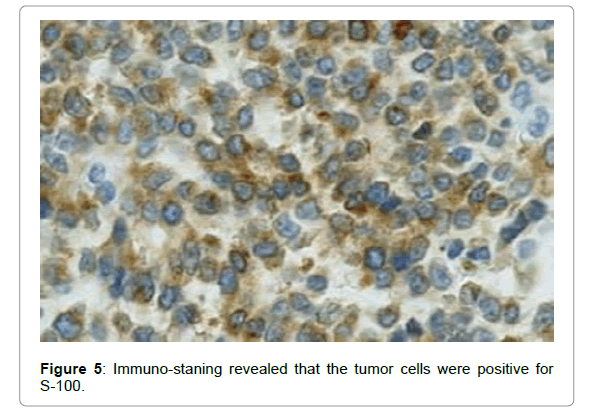
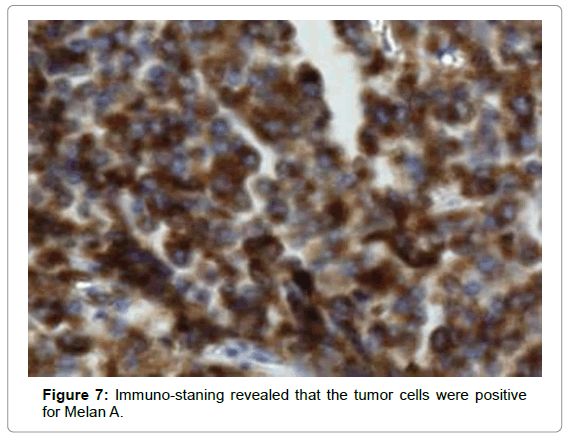
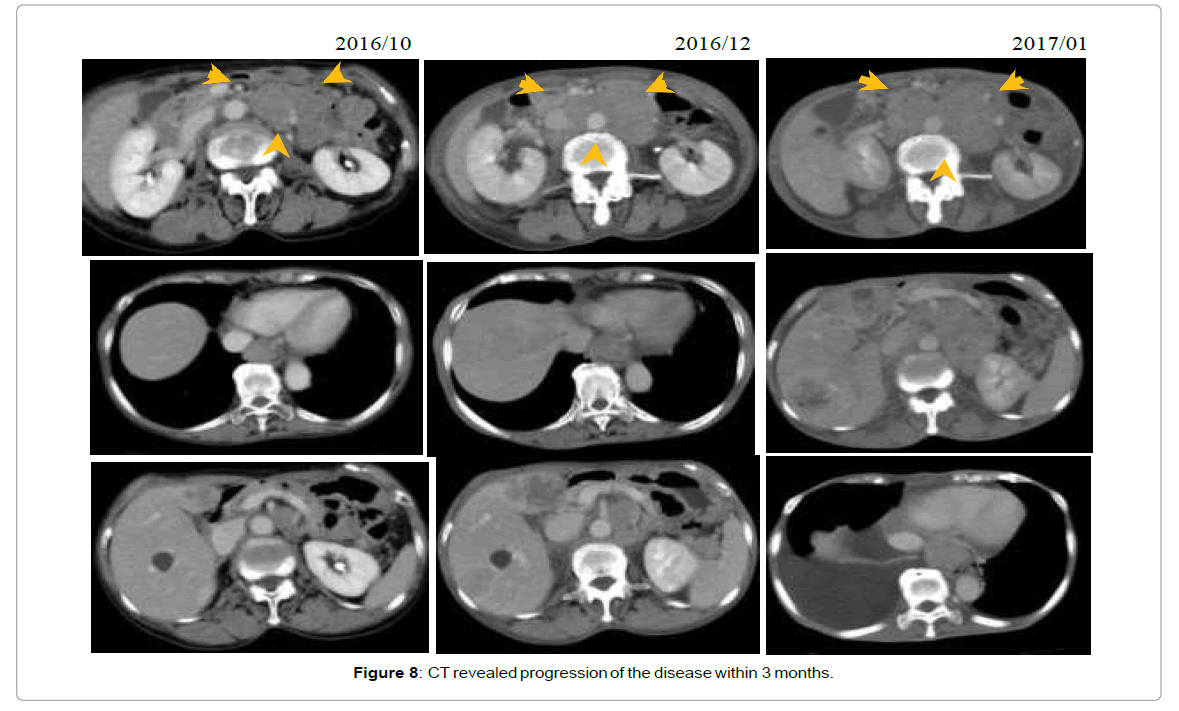
A 67-year-old woman visited our hospital, in August 2016, complaining of fatigue. A type 1 tumor (Figure 2) with blue pigment deposition in the lower esophagus was detected on upper endoscopy, and liver metastasis was observed using Positron Emission Tomography–Computed Tomography (PET-CT) (Figure 3). An esophageal biopsy revealed large tumor cells possessing minimal cytoplasm and hyperchromatic indistinct nucleoli based on HE staining (Figure 4). Immunostaining revealed that the tumor cells were positive for S-100 (Figure 5) and Melan A (Figure 6), and negative for HMB- 45 (Figure 7). Histological findings revealed malignant melanoma that had arisen from the esophagus. We initiated nivolumab (2 mg/ kg on day 1 every 3 weeks) therapy based on the negative results of the B-RAF V600E mutational test in September 2016. She exhibited no adverse events after the administration of nivolumab. However, CT revealed progression of the disease within 3 months (Figure 8). We changed to ipillimumab (3 mg/kg every 3 weeks) therapy in January 2017. However, she progressively weakened and died within 6 months of being diagnosed with the disease.
Results and Discussion
Esophageal melanoma is a rare occurrence (0.1%-0.2% of malignant esophageal tumors) [1,2]. The peak age of onset is in the 60s-70s and the male-to-female ratio is 2:1. Common sites of occurrence are from the mid to lower esophagus. The rate of multi-occurrence is 35.1%. Melanosis is detected in 0.11% of normal individuals but is thought to be a precursor lesion because of its coexistence in 10%-30% cases of esophageal melanoma. Seventy percent of patients experience difficulties in swallowing at diagnosis. Delayed diagnosis is common after growing up because of soft tissue compared to normal esophageal cancer tissue, and moderate invasion vertically. Endoscopic techniques are useful for the detection of tumors. Elevated lesions with unleveled surfaces and with black, blue, purple, and brown color in morphologic features is common. However, it is difficult to make a diagnosis based only on HE staining, in which case non-colored tumors occur [2].
Staining for S-100, HMB-45, and MelanA are useful to make a diagnosis in these cases.
Biopsies for cutaneous melanoma are contra indicatory because of the risk of hematogenous metastasis. However, biopsies for esophageal melanoma are not contra indicatory because of the lack of prognostic differences between biopsy and non-biopsy cases. Forty percent of patients exhibit lymph node or organ metastasis at prior diagnosis. The liver (31%-39%) is the most common metastatic site [1,2].
Treatment for mucosal melanoma, including those of esophageal origin, is based upon therapy for cutaneous melanoma. Curative treatment only requires a surgical approach. Preventive lymphadenectomy is useful to improve patient prognosis [3]. Chalkiadakis [1] et al., in 1985, reported that the 5-year survival rate was 4.2% and median overall survival time was 14 months after curative surgery. However, in recent years, the 5-year survival rate has improved up to 30%, owing to the widespread implementation of endoscopic tests [4]. Local injection of IFN-β for skin melanoma was reported as a useful adjuvant therapy, in the 1980s [5]. DAV-Feron therapy (DTIC/ ACNU/VCR plus local injection of IFN-β) as an adjuvant therapy is used frequently in Japan [6,7]. We used DAV-Feron therapy as adjuvant therapy after surgery, for case 1. However, these regimens are not recognized as standard because recent retrospective studies have not shown significant improvement of survival, and no randomized control trials have been conducted.
Treatment of metastatic esophageal melanoma is largely based upon experiences with patients having cutaneous melanoma. Decarbonize has been most frequently used as anti-cancer medication in patients with advanced metastatic melanoma. However, the response rate, complete response rate, and long-term response rate were low, 10%-20%, 5%, and less than 2%, respectively [8,9]. Thus, several combination therapies have been attempted in the past. The DAC-Tam modified ‘’Dartmouth regimen’’ from BCNU to ACNU was developed in Japan [10]. We used DAC-Tam as palliative chemotherapy, but this was unsuccessful in our case. Recently, decarbonize has not shown any significant survival benefits in randomized control trials or evidence of improving survival in meta-analyses [11,12].
Clinical studies depending on the development of molecular biology have been progressing rapidly in recent years. Ipillimumab is an anti-cytotoxic T-lymphocyte antigen-4. This is the first clinically applicable immune checkpoint inhibitor in oncological history with proven survival benefits in a phase III randomized study [13]. The current approved drugs for metastatic melanoma in the National Comprehensive Cancer Network guidelines that are applicable for insurance in Japan are follows. Nivolumab [14] and keytruda [15] are immune checkpoint inhibitors targeting the Programmed Death Ligand 1 (PD-L1/PD-1 pathways. Vemurafenib [16] and dabrafenib plus trametinib [17] are molecular targeting agents for patients with BRAF V600E mutation-positive metastasis. We have used nivolumab as first-line therapy because the patient in case 2 did not harbor a BRAF V600E mutation, and we used ipillimumab as second-line therapy subsequently. However, we received no response to both immune checkpoint inhibitor drugs in the patient with esophageal melanoma.
Conclusion
In conclusion, we herein report our experiences with two cases of metastatic and recurrent melanoma. Clinical studies depending on the development of molecular biology have been progressing rapidly in recent years. Ipillimumab is an anti-cytotoxic T-lymphocyte antigen-4. This is the first clinically applicable immune checkpoint inhibitor in oncological history with proven survival benefits in a phase III randomized study. However, we received no response to both immune checkpoint inhibitor drugs in the patient with esophageal melanoma.
Competing Interests
The authors state that they have no Conflict of Interest.
References
- Chalkiadakis G, Wihlm JM, Morand G, Bousson MW, Witz JP (1985) Primary malignant melanoma of the esophagus. Ann Thorac Surg 39: 472-475.
- Sabanathan S, Eng J, Pradhan GN (1989) Primary malignant melanoma of the esophagus. Am J Gastroenterol 84: 1475-1481.
- Yu H, Huang XY, Li Y, Xie X, Zhou JL, et al. (2011) Primary malignant melanoma of the esophagius: A study of clinical features. Pathology, management and prognosis. Dis Esophagus 24: 109-113.
- Volpin E, Sauvanet A, Couvelard A, Belghiti J (2019) Primary malignant melanoma of the esophagius : A case report and review of the literature. Dis Esophagus 15: 244-249.
- Ishihara K (1983) Clinical trials of human fibroblast interferon in the treatment of malignant tumors of the skin. J Jpn Soc Cancer Ther 18: 41-53.
- Yamamoto A, Ishihara K (1996) Clinical study of DAV+IFN-beta therapy combination adjuvant therapy with intravenous DTIC, ACNU and VCR, and local injection of IFN-beta-for malignant melanoma. Int J Immunother 12: 73-78.
- Matsumoto T, Yokota K, Sawada M, Shibata S, Yasue S, Et al. (2013) Postoperative DAV-IFN-beta therapy does not improve survival rates of stage ? and stage ? melanoma patients significantly. J Eur Acad Dermatol Venereol 27: 1514-1520.
- Hill GJ, Krementz ET, Hill HZ (1984) Dimethyl triazeno imidazole carboxamide and combination therapy for melanoma IV. Late results after complete response to chemotherapy (Central Oncology Group protocols 7130, 7131, and 7131A). Cancer 53: 1299-1305.
- Eigentler TK, Caroli UM, Radny P, Garbe C (2003) Palliative therapy of disseminated malignant melanoma: A systematic review of 41 randomised clinical trials. Lancet Oncol 4: 748-759.
- Chapman PB, Einhorn LH, Meyers ML, Saxman S, Destro AN, et al. (1999) Phase multicenter randomized trial of the Dartmouth regimen versus dacarbazine in patients with metastatic melanoma. J Clin Oncol 17: 2745.
- Crosby T, Fish R, Coles B, Mason M (2000) Systemic treatments for metastatic cutaneous melanoma, Cochrane Database Syst Rev.
- Sasse AD, Sasse EC, Clark LGO (2009) Chemo immunotherapy versus chemotherapy for metastatic malignant melanoma. Cochrane Database Syst Rev.
- Hodi FS, O’Day OSJ, McDermott DF, Weber RW, Sosman JA, et al. (2010) Improved survival with ipillimumab in patients with metastatic melanoma. N Engl J Med 363: 711-723.
- Long VG, Atkinson V, Ascierto PA, Robert C, Hassel JC, et al. (2016) Effect of nivolumab on health-related quality of life in patients with treatment-naïve advanced melanoma: Results from the phase III CheckMate 066 study. Ann Oncol 27: 1940-1946.
- Ribas A, Puzanov I, Dummer R, Schadendorf D, Hamid O, et al. (2015) Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): A randomized, controlled, phase 2 trial. Lancet Oncol 16: 908-918.
- Flaherty KT, Puzanov I, Kim KB, Ribas A, McArthur GA, et al. (2010) Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med 363: 809-819.
- Long GV, Stroyakovskiy D, Gogas H, Levchenko E, Braud FD, et al. (2015) Dabrafenib and trametinib versus dabrafenib and placebo for Val600 BRAF-mutant melanoma: A multicentre, double-blind, phase 3 randomised controlled trial. Lancet 386: 444-451
Citation: Hiramoto S, Kikuchi A, Hori T, Mikako T, Yamaga Y, et al. (2021) Two Cases of Advanced Malignant Melanoma Occurring from the Esophagus. J Oncol Res Treat S2:001. DOI: 10.4172/aot.s2.1000001
Copyright: © 2021 Hiramoto S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3160
- [From(publication date): 0-2021 - Dec 03, 2025]
- Breakdown by view type
- HTML page views: 2281
- PDF downloads: 879