Using a Text-Messaging Intervention to Promote Behavior Change in Undeserved Adolescents in a Mobile Health Clinic
Received: 03-Jan-2019 / Accepted Date: 28-Mar-2019 / Published Date: 05-Apr-2019 DOI: 10.4172/2375-4494.1000384
Abstract
Purpose: We developed and implemented a novel text-messaging intervention (TMI) to disseminate knowledge about adolescent-relevant health issues to underserved adolescents treated in a mobile health clinic (MHC) setting. The goal was to both increase participants’ knowledge and support positive change in participants’ health-related behaviors.
Methods: Patients from our mobile clinic sites were invited to participate in a text-messaging intervention with the aim of increasing health-related knowledge and promoting behavior change. Participants chose 1-2 topics from a list of 15 adolescent-relevant health issues. For each topic chosen, participants completed a program consisting of three text messages in a quiz format each week for 14 weeks. Participants were encouraged to reply with their answer choice; after doing so, they received a response message with the correct answer, a brief explanation, and follow-up information. Prior to and after completion of each program, participants completed a ten-item questionnaire. The results of the pre- and post-intervention assessments were compared using Wilcoxon Signed-Rank tests to identify changes in perceived knowledge, self-efficacy and health-related behaviors.
Results: 72 adolescents from our clinics completed between one and four interventions each during the 18-month-long study. Significant improvement from pre- to post-survey was found in self-reported knowledge for 7 of 14 intervention topics and self-reported behavior for 8 of 14 intervention topics.
Conclusions: Participants who engaged with the TMI showed self-reported improvements in topic-related knowledge, self-efficacy and health-related behavior choices. TMIs have considerable potential to deliver relevant health-related information and to support positive changes in participant’s health-related behaviors.
Keywords: Adolescents; Medically uninsured; Underserved; Mobile health clinic; Short messaging service; Text messaging intervention; Health-related behaviors; Collaboration
Introduction
Encouraging and supporting patients’ efforts toward making positive changes in health-related behaviors (HRB) is crucial to improving their health outcomes. There are many barriers to providing this support to patients; this is particularly true with adolescents, where limited contact time with providers, incongruent communication styles, and lack of patient engagement can erode clinical influence. These barriers are even more pronounced for at-risk adolescents, including uninsured and homeless youth [1,2]. Providers of adolescent health care, and especially those that work with at-risk youth, must develop interventions that address these barriers and actively engage patients in the prevention and treatment process.
Developing adolescent-focused interventions is one of the primary missions of the Stanford Teen Health Van. The Van is a mobile medical clinic which provides free, comprehensive primary health care services to uninsured and underinsured teens and young adults. We partner with schools and community agencies to provide regular clinic services at multiple sites from San Francisco to San Jose. Services are provided to approximately 400 unique adolescents each year. While ethnically diverse, members of our patient community typically share multiple bio psychosocial stressors: substance use and lack of family and economic support are common, and approximately 40% have been homeless at some point in the past year. The Teen Health Van serves as a mobile medical home for this diverse group of adolescents; a place where they can receive treatment for illness, but also where they can gain knowledge and direction to aid them in optimizing wellness. To support meaningful behavior change in this large adolescent population, it is essential to utilize interventions that can both provide effective adolescent-relevant education and overcome barriers to patient engagement.
Short message service (SMS) or text messaging is a communication medium widely accessible to and very popular with adolescents across a wide demographic spectrum. Most studies have found that 95-99% of adolescents have access to a SMS-enabled device [3-5]. Likewise, many adolescents report text messaging as their preferred mode of communication, even when other modes are freely available [3-6].
Text-messaging interventions (TMI) have been shown to be beneficial and cost-effective as an adjunct to standard medical treatments with adolescents [3-10]. The majority of TMIs to date have utilized reminder messages (e.g., supporting medication adherence or regular blood glucose testing) or motivational messages to encourage adherence to a previously-defined treatment regimen. Notably few programs have attempted to deliver novel health information to promote health-related behavior change; and fewer still have been aimed at the adolescents, and then only in limited clinical settings. Given its broad availability, the flexibly and adaptability of its platform and its popularity with adolescents, text messaging would seem to have great potential as a means of providing relevant health care education to adolescents [11].
We collaborated with the adolescent patients of our mobile health clinic to develop a TMI to disseminate health information relevant to adolescents. Our goals were to increase their knowledge of relevant health issues and support change in health-related behaviors. A pilot study of this program demonstrated that a TMI was both feasible and engaging for an underserved adolescent population. For this study, we offered enrollment in our TMI to all adolescents seen at every clinic site. We hypothesized that our participants would report significant improvement in perceived knowledge and self-reported health-related behaviors. These results would support the view that TMI can be an effective tool for disseminating information and increasing participants’ knowledge about adolescent-relevant healthcare issues, and this in turn can effectively support positive change in participants’ health-related behaviors.
Methods
Intervention
A multidisciplinary team of mobile health clinic providers (a physician, nurse practitioner, licensed clinical social worker, and a registered dietitian) compiled a list of 15 adolescent-relevant health topics based upon a review of the visit diagnoses most frequently encountered in our clinic. The topics chosen were: Abdominal Pain, Asthma, Birth Control, Depression and Anxiety, Fitness, Headaches, Mental Health, Nutrition, Relationships, Sexually Transmitted Infections (STIs), Stress, Substance Abuse, Tobacco Cessation and Weight Management. Educational messages for each topic were developed by the Teen Health Van staff noted above and compiled a program of 42 individual messages [12]. The messages were then reviewed by 12 adolescent patients from several mobile health clinic sites to provide feedback on content, clarity, format, length and timing of message delivery. Notably, several adolescent reviewers suggested that changing the TMI structure to an interactive quiz format would be more engaging than sending TMI content as simple informative statements. In response to this, clinic staff restructured the messages into a question-and-answer (true/false and multiple choice) format. Other suggestions from adolescents for optimizing engagement which were integrated into the TMI included limiting the number of text messages to a total of 3 messages per week (Monday, Wednesday and Friday) and sending text messages in the late afternoon (17:00.)
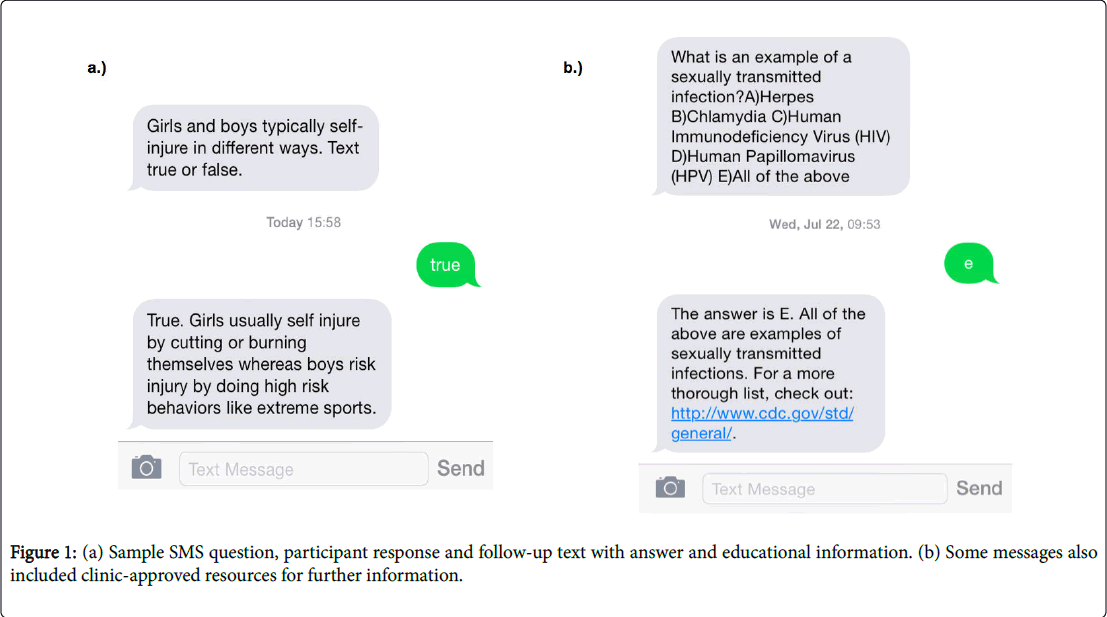
Following this initial review, we contracted with a health communications developer (Care Message) to develop a HIPAA- and PHI-compliant SMS platform to deliver message content. The messages for each program were converted into SMS format, as questions which invited participants to text a reply with a selected answer choice (Figure 1). Every reply received a response message with the correct answer, an explanation, and follow-up information. Participants were sent three text messages per week for 14 weeks, for a total of 42 text messages per program [13,14]. Participants could elect to receive program texts using their own SMS-enabled device or one provided to them at no cost by the Verizon Foundation, with unlimited text messaging credit for the duration of the study. Participants were given the choice of receiving messages in English or Spanish.
A small incentive (participant’s choice of either two free movie tickets or a gift card to a department store, each with a value of $20) was offered to all participants who remained enrolled for the duration of the intervention and replied to 50% or more messages for one or more topics.
Participants
All patients visiting our mobile health clinic were eligible to participate in the intervention. Participation was based solely on patient interest, and we did not recruit patients based on any characteristic or condition.
Measures
Prior to starting each program, participants completed a topicspecific pre-intervention questionnaire consisting of 10 questions. Most questionnaires presented answer choices in a 4-point Likert scale format, though some questionnaires contained questions with 3-point and true/false answer choices.
For 7 of the 14 topics, approximately half of the questions assessed perceived knowledge and half assessed behavior choices (Asthma, Birth Control, Nutrition, Stress, Substance Abuse, Tobacco Cessation, Weight Management.) For 4 topics (Abdominal Pain, Fitness, Headache, Stress) the majority of questions addressed perceived knowledge; for the remaining 3 topics (Depression and Anxiety, Relationships and Self-Esteem) most questions inquired about behavior choices.
Upon completion of each texting program, participants were asked to complete the topic-specific questionnaire a second time.
This project was approved by the Stanford University Institutional Review Board.
Results
Analysis
Responses from pre- and post-intervention questionnaires were compiled and coded numerically. Participants were included in our final analyses if: 1) their response rate for the intervention was greater than 50% and 2) they completed both pre- and post-intervention questionnaires. Information regarding the number of participants, their response rates and rates of questionnaire completion are presented in Table 1.
| Participants enrolled | 240 |
|---|---|
| Intervention enrollment for each participant | One: n=12 (5%) |
| Two: n=194 (81%) | |
| Three: n=21 (9%) | |
| Four: n=13 (5%) | |
| Participants with Response Rate (RR) >= 50% | 121 (50%) |
| Participants with completed Pre-+Post-questionnaire | 79 (33%) |
| Participants with RR>=50%+completed questionnaire (inclusion criteria) | 72 (30%) |
Table 1: Participant, registration, response rates and inclusion criteria for analysis.
We performed non-parametric statistical analysis of responses (the Wilcoxon Signed-Rank Test) using SSPS to assess for significant intratopic change in perceived knowledge and self-reported behavior. One of the 15 intervention topics (Mental Health) did not have a sufficient number of participants and thus was not included in the analysis.
Results of analyses of pre- and post-intervention questionnaire responses regarding perceived knowledge are presented in Table 2. Mean Post-Intervention scores were higher for all 14 topics, with differences that were significant for 7 topics (Asthma, Birth Control, Fitness, Stress, Substance Abuse, Tobacco Cessation and Weight Management), not significant for 3 topics (Abdominal Pain, Headache and STIs) with the remaining 4 topics (Depression and Anxiety, Nutrition, Relationships and Self Esteem) having insufficient questions about perceived knowledge for inclusion in analysis. Notably, the topics for which we did not see a significant difference were those with the lowest number of respondents.
| Topic | Pre-Intervention Score (mean ± SD) | Post-Intervention Score (mean; SD) | p value |
|---|---|---|---|
| Asthma (n=26) | 2.91 ± 0.52 | 4.00 ± 0 | .000 * |
| Relationships (n=15) | n/a | ||
| Fitness (n=11) | 1.97 ± 0.36 | 2.97 ± 0.10 | .003 * |
| Weight Management (n=11) | 1.92 ± 0.26 | 2.32 ± 0.05 | .007 * |
| Substance Abuse (n=10) | 1.08 ± 0.19 | 1.98 ± 0.06 | .003 * |
| Tobacco Cessation (n=10) | 2.46 ± 0.16 | 3.88 ± 0.25 | .005 * |
| Stress (n=8) | 2.38 ± 0.35 | 3.05 ± 0.14 | .017 * |
| Birth Control (n=7) | 2.70 ± 0.54 | 4.07 ± 0.31 | .016 * |
| Depression/Anxiety (n=7) | n/a | ||
| Nutrition (n=6) | 1.86 ± 0.22 | 3.0 ± 0 | n/a |
| STIs (n=4) | 2.54 ± 0.25 | 3.50 ± 0 | 0.066 |
| Self Esteem (n=4) | n/a | ||
| Abdominal Pain (n=3) | 2.19 ± 0.28 | 3.89 ± 0 | 0.109 |
| Headache (n=3) | 2.26 ± 0.45 | 3.96 ± 0.06 | 0.109 |
| Significance threshold: p<0.05 (indicated by *). | |||
Table 2: Results of Wilcoxon Signed-Rank Test comparing pre and post intervention questionnaire score for perceived knowledge (higher scores = higher self-reported knowledge). Topics listed in decreasing order by number of participants per program.
Results of analyses of pre- and post-intervention questionnaire responses regarding self-reported behavior change knowledge are presented in Table 3. Mean Post-Intervention scores were higher for all 14 topics, with differences were significant for 8 topics (Asthma, Birth Control, Depression and Anxiety, Fitness, Relationships, Substance Abuse, Tobacco Cessation and Weight Management), not significant for 2 topics (Nutrition, Self Esteem) with the remaining 4 topics (Abdominal Pain, Headache, Stress and STIs) having insufficient questions about perceived knowledge for inclusion in analysis. As with perceived knowledge, the two topics for which we did not see a significant difference were among those with the lowest number of respondents.
| Topic | Pre-Intervention Score (mean ± SD) | Post-Intervention Score (mean; SD) | p value |
|---|---|---|---|
| Asthma (n=26) | 3.02 ± 0.92 | 4.93 ± 0.10 | .000 * |
| Relationships (n=15) | 4.19 ± 0.58 | 4.96 ± 0.10 | .001 * |
| Fitness (n=11) | n/a | ||
| Weight Management (n=11) | 1.18 ± 0.23 | 2.82 ± 0.23 | .003 * |
| Substance Abuse (n=10) | 3.04 ± 1.08 | 4.2 ± 0.69 | .024 * |
| Tobacco Cessation (n=10) | 3.76 ± 0.94 | 5.24 ± 0.45 | .007 * |
| Stress (n=8) | n/a | ||
| Birth Control (n=7) | 3.83 ± 0.86 | 4.90 ± 0.09 | .018 * |
| Depression/Anxiety (n=7) | 3.26 ± 0.39 | 3.96 ± 0.15 | .012 * |
| Nutrition (n=6) | 1.11 ± 0.17 | 2.56 ± 0.27 | .023 * |
| STIs (n=4) | 2.75 ± 0.35 | 3.75 ± 0.00 | 0.066 |
| Self Esteem (n=4) | 2.33 ± 0.47 | 3.22 ± 0.83 | 0.14 |
| Abdominal Pain (n=3) | n/a | ||
| Headache (n=3) | n/a | ||
| Significance threshold: p<0.05 (indicated by *). | |||
Table 3: Results of Wilcoxon Signed-Rank Test comparing pre and post intervention questionnaire scores for self-reported behavior (higher scores = more improved self-reported behavior). Topics listed in decreasing order by number of participants per program.
Discussion
Text messaging has become a favored method of communication for adolescents from a wide range of ethnic and socioeconomic backgrounds, and virtually all adolescents possess text messagingenabled devices and texting data plans.3-5 Given this, text messaging would seem to be a logical choice for connecting with and providing health interventions for adolescents. In this study, adolescents completing our TMI had improved post-intervention scores for perceived knowledge and self-reported behavior change for all topics, with significant improvement in for the majority of topics included in analysis. These findings support the utility of TMIs for disseminating health-related information, with the goal of supporting improved wellness.
While our results are encouraging, there are certain limitations to this study. Study participation was voluntary, and thus our participants may have been more receptive to TMI than the general adolescent population. Our clinic population is uninsured and primarily Latino; given this demographic makeup, our results may be less applicable to other groups of adolescents. While our results show significant prepost changes for almost all topics, the power of the results for several topics is limited by small sample sizes.
To generate the most effective educational messages for adolescents, it is essential to involve the adolescents themselves in the development of their interventions. Previous work has demonstrated that acknowledging adolescents as experts on their issues and enlisting them in active evaluation and development of clinical programs results in more relevant content and optimized delivery. Furthermore, interventions that have been refined based on feedback from adolescents have improved patient engagement. We involved adolescents in each step of the pilot intervention development process. We did note that adolescents commented very positively on aspects of the intervention suggested by their peers (e.g., the question-andanswer format, the text message length, etc.), and this suggests that adolescents should play a prominent role in the development of future projects.
The most important next steps in TMI development are, broadly: 1) to refine the structure and delivery of TMI, and 2) to develop methods to better assess their true utility as interventions to promote behavior change. We have continued to refine our TMI program (e.g., standardizing pre-/post questionnaires, automating questionnaire completion and data tabulation) and will continue to make this intervention available to all patients of the Teen Health Van. In future interventions, it would be optimal to expand TMIs to utilize two-way communication between patients and health providers, with individual questions serving as springboards to prompt participants to reach out to clinic medical staff with any personal questions or concerns.
Conclusion
TMIs allow health care providers to connect to teen patients on a more regular and less formal basis via a broadly accessible medium with which teens are generally very comfortable and often more easily engaged. As a result, they show great promise as a means of increasing dissemination of health-related information to adolescents (and by extension, supporting them in making more positive health behavior choices) while simultaneously increasing their engagement with healthcare interventions and their medical home.
Acknowledgements
We would like to thank the Lucile Packard Foundation for Children’s Health and the Children’s Health Fund, who are the primary funders of the LPCH Teen Health Van. A grant from the Verizon Foundation provided support for this study. Care Message provided the PHI- and HIPPA-compliant platform utilized. Lucile Packard Children’s Hospital Stanford provided a community investment grant for this project.
References
- Murphy DC, Klinghoffer I, Fernandez-Wilson JB, Rosenberg L (2000) Mobile health units: Design and implementation considerations. AAOHN Journal 48: 526-532.
- Redlener I, Redlener D (1994) System-based mobile pediatric care for homeless children - the anatomy of a working program. Bulletin of the New York Academy of Medicine 71: 49-57.
- Cole-Lewis H, Kershaw T (2010) Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews 32: 56-69.
- Hall AK, Cole-Lewis H, Bernhardt JM (2015) Mobile text messaging for health: a systematic review of reviews. Annual Review of Public Health 36: 393-415.
- Militello LK, Kelly SA, Melnyk BM (2012) Systematic review of text-messaging interventions to promote healthy behaviors in pediatric and adolescent populations: implications for clinical practice and research. Worldviews Evidence Based Nursing 9: 66-77.
- Lau PW, Lau EY, Wong DP, Ransdell L (2011) A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. Journal of Medical Internet Research 13: e48.
- Haug S, Schaub MP, Venzin V, et al. (2013) A pre-post study on the appropriateness and effectiveness of a Web- and text messaging-based intervention to reduce problem drinking in emerging adults. Journal of Medical Internet Research 15: e196.
- Suffoletto B, Callaway CW, Kristan J, et al. (2013) Mobile phone text message intervention to reduce binge drinking among young adults: study protocol for a randomized controlled trial. Trials 14: 93.
- Haug S, Meyer C, Dymalski A, et al. (2012) Efficacy of a text messaging (SMS) based smoking cessation intervention for adolescents and young adults: study protocol of a cluster randomised controlled trial. BMC Public Health 12: 51.
- Britto MT, Munafo JK, Schoettker PJ et al. (2012) Pilot and feasibility test of adolescent-controlled text messaging reminders. Clinical Pediatrics (Philadelphia) 51: 114-121.
- Stewart TC, Harrington J, Batey B, Merritt NH, Parry NG (2015) From focus groups to production of a distracted driving video: Using teen input to drive injury prevention programming. Journal of Trauma and Acute Care Surgery. 79(3) Supplement 1 Forging New Frontiers: The 19th Annual Conference of the Injury Free Coalition for Kids 3:S42-S47.
- Heary CM, Hennessy E (2002) The use of focus group interviews in pediatric health care research. Journal of Pediatric Psychology 27: 47-57.
- Crowley R, Wolfe I, Lock K et al. (2011) Improving the transition between paediatric and adult healthcare: a systematic review. Archives of Disease in Childhood 96: 548-553.
- Irons M, Tomaszewski K, Muñoz Buchanan CR, Trent M (2015) Understanding Adolescent Nonresponsiveness to Text Messages: Lessons from the DepoText Trial. Journal of Urban Health 92: 502-512.
Citation: Ammerman SD, Halpern-Felsher B, Weiss C (2019) Using a Text-Messaging Intervention to Promote Behavior Change in Undeserved Adolescents in a Mobile Health Clinic. J Child Adolesc Behav 7: 384. DOI: 10.4172/2375-4494.1000384
Copyright: © 2019 Ammerman SD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3829
- [From(publication date): 0-2019 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 2913
- PDF downloads: 916