Parathyromatosis Coexisting with Papillary Thyroid Microcarcinoma
Received: 31-Jul-2011 / Accepted Date: 15-Nov-2011 / Published Date: 19-Nov-2011 DOI: 10.4172/2161-0681.1000103
Abstract
Summary: The aim of this report is to describe a fortuitely discovered association between parathyromatosis and papillary thyroid microcarcinoma. Case description: A 56 year old woman presented with a pyelic relapsed stone, bone pains, neurovegetative complaints and iPTH = 348 ng/l as manifestations of recurrent primary hyperparathyroidism after a right inferior parathyroid adenoma exeresis done elsewere six years ago. Ultrasonography showed a 5 mm hypoechoic zone at the lower pole of the right lobe of the thyroid. At the operation an irregular, unbounded, white-yellowish mass 5 mm in diameter was identified lateral and below the thyroid pole together with 15-20 nodules of 1-2 mm scattered on the distal surface of the gland and also in the areolar fibrofatty surrounding atmosphere. Excision and biopsy of the mass and of two main nodules showed the presence of parathyroid issue and the operation is finally completed to a thyroid lobectomy. Definitive paraffin examination evidencied multiple poorly outlined nests of benign parathyroid tissue but also a minute foci of papillary thyroid carcinoma. Two years after the operation the patient is symptom free without any local recurrence and in normal biological parameters. Discussion: Coexistence between parathyromatosis - a rare but challenging cause of hyperparathyroidism – and thyroid (micro) carcinoma a more frequent encountered lesion is an entirely coincidental occurrence. The preoperative diagnosis of both conditions - particularly of the latter one – is rarely anticipated. In such intraoperative fortuitous finding the intervention must include an en bloc thyroid lobectomy together with periglandular and retro-sternal fibrofatty tissue. This strategy is beneficent also for the eventually nonidentified thyroid microcarcinoma. Conclusions: Preoperative and intraoperative evaluation for recurrent primary and renal hyperparathyroidism must be exhaustive considering possible coexisting thyroid lesions. Indeed in our knowledge there have been no reports in the literature mentioning this unprecedented entity.
Keywords: Parathyromatosis; Thyroid microcarcinoma; Reoperation; Thyroid lobectomy
308034Introduction
Postoperative clinical, biochemical or histological persistence or recurrences observed in primary and renal hyperparathyroidism are determined by inadequate operations, existence of ectopic or supranumerary glands, parathyroid carcinoma, MEN 1 and also by parathyromatosis, a rare recently described entity. This latest lesion consists of hyperfunctioning parathyroid tissue disposed as micronodules or cellular aggregates capriciously scattered in the cervical loge and mediastinum but also on/in the thyroid gland, thymic rests, adipose and muscular surrounding soft structures [1-4].
Sporadic case reports and small surgical series of parahyromatosis distinguished two pathogenic varieties: - the first of them is due to the hyperplasia of glandular nests from embryological descent of parathyroids; - the second and more frequent one is determined by the inadvertent intraoperative fracture of glandular capsule or parenchyma which can become implanted in the surgical area [5,6].
The diagnosis of parathyromatosis seldom confounded with parathyroid carcinoma is difficult, the lesion often escaping to imaging studies, being identified only intraoperatively or by microscopic examination [7]. The mainstay treatment of this bizarre lesion is surgery however a coherent operative strategy is missing due to the small number of cases. Administration of calcimimetics have controversial effects. Both methods seems to be unable to assure an optimistic percentage of definitive cure [8]. Like another parathyroid lesions parathyromatosis can be associated with different thyroid pathological changes. The present case described the fortuitous coexistence of parathyromatosis with papillary thyroid carcinoma, an entity which have not yet be reported in the literature.
Case description
A 56 year old woman is admitted in our clinic with recurrent primary hyperparathyroidism six years after a right inferior adenoma removal done elsewere. The diagnosis is sustained by the relapse in the last year of pyelic lithiasis with frequent renal colics, osteoarticular pains, anorexia and dyspeptic symptoms, myasthenia, emotional irritability and depression. The laboratory tests showed raised levels of iPTH – 348 ng/l and alkaline phosphatase – 195 iu/l but normal values of seric calcium and phosphorus. Ultrasonography noticed an unhomogeneous hypoechoic zone of about 5 mm in diameter situated at the inferior right pole of the thyroid gland, image unsustained by Tc- 99m tetrophosmin scan which only indicates diminished tracer uptake. (Figure 1)
The reintervention going on in a “hostile” surgical field determined by fibrosis and adherences identified an irregular, not bounded, whiteyellowish, 5 mm mass, situated laterally and under the inferior pole of the thyroid to which it is adhering and extended in the thyrothymic ligament. Moreover about 15-20 similar micronodules until 2 mm are scattered on the surface or even inlaided in the thyroid tissue or in the fibrofatty atmosphere of the tracheoesophageal groove. Excision and frozen section of the main mass and two of the satellite lesions showed the presence of hypercellular parathyroid tissue without stigma of malignancy.
However the impossibility to exclude the presence of a carcinoma conduced to an extended thyroid lobectomy involving the isthmus and 3-4 cm from thyrothymic ligament retrosternally together with parathyroid fibrofatty tissues.
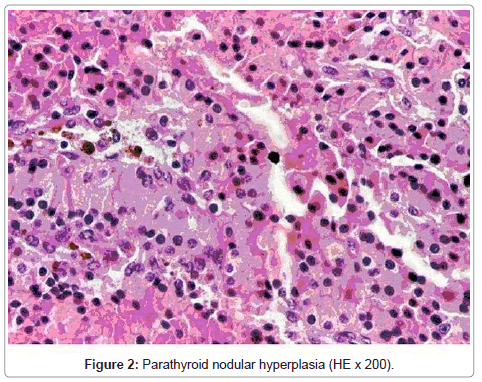
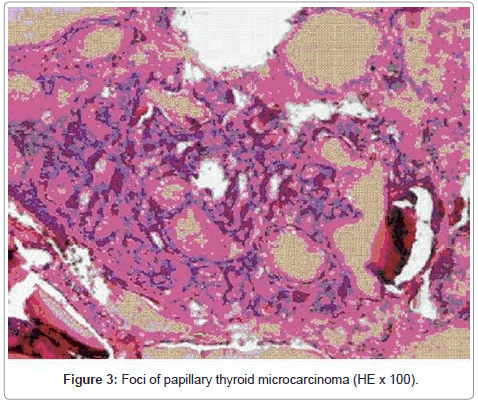
The definitive paraffin examination confirmed the existence of many fold microgrowths and cellular agregates composed of benign parathyroid chief cells with uniform nuclei and clear cytoplasma without atypia but also a limited foci of papillary thyroid microcarcinoma measuring about 2 mm, without tissular, vascular or lymphatic extension. Figure 2, 3 considering the characters of both lesions, especially of those of incidentally discovered thyroid microcarcinoma, periodical recurring at regular intervals of the patient was decided. At 6, 12 and 24 months postoperatively she is symptom free without any local recurrence and normocalcemic. Levels of iPTH and TSH are 76, 46 and 29 ng/l respectively 1,5, 2 and 2,5 ml/l. However the effects of the adopted surgical solution, beneficial for each of diseases, are unfortunately no definitive imposing a long-period supervision.
Discussion
Parathyromatosis was initially mentioned by Palmer [9] which described the lesion in a patient with tertiary hyperparathyroidism and by Reddick [10] which proposed the actual denomination.“De novo” observations without any preceding operations and primitive (onthogenic) cases are very rare appearing preferentially in patients with refractory renal hyperparathyroidism on chronic hemodialysis while the more common second type occurs after spillage and seeding of glandular tissue indifferently of pathologic substratum [11,12]. However in primary hyperparathyroidism the risk of fracture of the capsule and glandular tissue seeding is minimal in the exeresis (even minimally invasive) of adenomas and also rare notified in operations for parathyroid hyperplasia.
The majority of cases are recorded after parathyroidectomies for renal hyperparathyroidism where the dissection and handling of the little glands recommended to be done at the minuscule pedicle’s level and also the eventually sections can produce solutions of continuity of the capsule or parenchyma.
It must be remembered that chronic kidney failure consitued a permanent stimulating factor concerning the both embryonary and postoperative glandular rests. Otherwise even the hypertrophy and hyperplasia of the transplanted fragment of the “most normal” gland in the arm or another locations is considered a variety of parathyromatosis. Rarely evoked or affirmed before operation the diagnosis of this condition is however suggested by the context of previous parathyroid operation and by persistence or recurrence of the clinical and bioumoral syndrome. Imaging explorations included ultrasonography which identified multiple hypoechoic areas scattered deeply and superficially in the anterior cervical and retromanubrial territories sometimes in atypical locations and often hypervascularised at Doppler examination and related uptake at single-proton emission computer tomography better observed with a parallel collimator than with a pinhole one. Fine needle aspiration biopsy appeared utile in some observations [7,11,14]. For all these conditions intraoperative exploration confirmed by definitive paraffin examinations constituted the main elements of diagnosis.
Macroscopically the lesions appeared as multiple (until 80) irregular white-yellowish nodules, with 1-30 mm O aleatory distributed in the perithyroid atmosphere, usually in the side previously operated in the tracheoesophageal groove, on or in the thyroid gland, in the superior mediastinum, in all of these suggering initially the presence of secondary carcinomatous deposits. Cicatriceal modifications and fibrosis render more difficult the evaluation. Microscopic characters attests the lesion’s benignity: trabecular disposition, presence of mitoses and nuclear pleomorfism without vascular or lymphatic invasion. However the examination can surprisingly discover malignant aspects or the coexistence of another cancerous pathology as in our observation [15]. The treatment of parathyromatosis cannot be standardized owing to small number of cases. Surgery represents the necessary resource both for the diagnosis and the therapeutics, operative strategy being ad-hoc established in the majority of cases depending of the absence of preoperative diagnosis and lesional surprises with their chaotic distribution and (un)recognition or confusion with a carcinoma [5,7,9,16,17]. The main objective of the operation is as complete as possible excision of the hyperfunctionally glandular tissue which is practically impossible to do because beyond the identificable microlesions there are microscopic foci which once cannot be visualized. Therefore a semblable attitude with that for carcinomas is adopted as is were en block exeresis of all the visible lesions together with the ipsilateral thyroid lobe and the surrounding fibrofatty atmosphere from the thyroid cartilage to the thymic lodge [18]. A radical surgical act become more difficult because of the unequally degree of development of the parathyroid lesions at the time of intervention, the eventually residual foci influenced by their stimulating factors continuing their own evolution and imposing repeated more and more difficult operations. The high parathyromatosis potential for recurrences engendered skepticism regarding both the eficacity of its surgical treatment and prognosis, some authors assigning an irreversible course of this entity. Percutaneous ethanol injection with subsequent ischemic necrosis together with administration of biphosphonates, vitamine D analogues and especially calcimimetics was also proposed in the therapy of parathyromatosis. The last ones completes and prolongs the clinical effects of surgery and stabilized for notable intervals the levels of iPTH, calcium and phosphates [19-21].
Conclusion
Even if the prevalence of nonmedullary thyroid microcarcinoma in the parathyroid gland surgery is notable, the coexistence of this neoplasia with parathyromatosis was not yet been reported and our case seems to be the first related one in medical literature.
Inspite of possible pathogenic speculations for a causative relationships this immediate association remains a simple coincidence. Every endocrine surgeon needs to be aware of the possible synchronous presence of thyroid and parathyroid lesions, careful exploration of both glands is mandatory in surgery for hyperparathyroidism in order to exclude the presence of a thyroid carcinoma. Incidentally discovered (micro) nodulary thyroid lesions should be prompt submitted to a frozen section diagnosis and no less than a total lobectomy must be done.
Consent: The patient has given her consent for the case report to be published
Competing interest: The authors mentioned that they have not competing interest
Author’s contribution: MRD was the major contributor in writing the manuscript.MG and SD performed the clinical assessement and the literature review. MG confirmed the diagnosis by histopathological findings. All authors read and approved the final manuscript.
Acknowledgements
The authors thanks dr E Popescu for its friendly support in the manuscript typewriting
References
- Rattner DW, Marrone GC, Kasdon E, Silen W (1985) Recurrent hyperparathyroidism due to implantation of paratiroid tissue. Am J Surg 149: 745-748.
- Fitko R, Roth SI, Hines JR, Roxe DM, Cahill E (1990) Parathyromatosis in hyperparathyroidism. Hum Pathol 21: 234-237.
- Kollmorgen CF, Aust MR, Ferreiro JA, McCarthy JT, van Heerden JA (1994) Parathyromatosis: a rare yet important cause of persistent and recurrent hyperparathyroidism. Surgery 116: 111-115.
- Stehman-Breen C, Muirhead N, Thorning D, Sherrard D (1996) Secondary hyperparathyroidism complicated by parathyromatosis. Am J Kidney Dis 28: 502-507.
- Lentsch EJ, Withrow KP, Ackermann, Bumous IM (2003) Parathyromatosis and recurrent hyperparathyroidism. Arch Otolaryngol Head Neck Surg 129: 894-896.
- Lee PC, Mateo RB, Clarke MR, Brown ML, Carty SE (2001) Parathyromatosis a cause of recurrent hyperparathyroidism. Endocr Pract 7: 189-192.
- Carpenter JM, Michaelson PG, Linder TK, Hinni ML (2007) Parathyromatosis. Ear Nose Throat J 86: 21.
- Matsuoka S, Tominaga Y, Sato T, Uno N, Goto N et al. (2007) Recurrent renal hyperparathyroidism caused by parathyromatosis. World J Surg 31: 299-305.
- Palmer JA, Brown WA, Kerr WH, Rosen IB,Watters NA (1975) The surgical aspects of hyperparathyro-idism. Arch Surg 110: 1004-1007.
- Reddick RL, Costa JC, Marx SJ (1977) Parathyroid hyperplasia and parathyromatosis. Lancet 1: 549.
- Tublin ME, Yim JH, Carty SE (2007) Recurrent Hyperparathyroidism Secondary to Parathyromatosis. Clinical and Imaging Findings. J Ultrasound Med 26: 847- 851.
- Fernandez-Ranvier GG, Khanasfshar E, Jensen K, Zarnegar R, Lee J, et al. (2007) Parathyroid Carcinoma, Atypical Parathyroid Adenoma or Parathyromatosis ?. Cancer 110: 255-264.
- Melck AL, Carty SE, Seethala RR, Armstrong MJ, Stang MT, et al. (2010) Recurrent hyperparathyroid-ism and forearm parathyromatosis after total parathyroidectomy. Surgery 148: 867-873.
- Koukouraky S, Stathaki M, Stylianou K, Daphnis E, Karkavitsas N (2007) Parallel hole versus pinhole collimator for technetium-99m sestamibi scintigraphy in the diagnosis of parathyromatosis. Hell J Nucl Med 10: 33.
- Baloch ZW, Fracker D, LiVolsi VA (2001) Parathyromatosis a cause of recurrent hyperparathyroidism: a cytologic diagnostic. Diagn Cytopathol 25: 403-405.
- Evans CF, Mansfield L, Shama AK (2005) Recurrent hyperparathyroidism caused by parathyromatosis. Hosp Med 66: 424-425.
- Daphnis E, Stylianou K, Katsipi I, Stratigis S, Karamitopoulou E, et al. (2006) Parathyromatosis and the challenge of treatment. Am J Kidney Dis 48: 502- 505.
- Sokol MS, Kasolius J, Schaaf M, D'Avis J (1993) Recurrent hyperparathyroidism from benign seeding: a review of recommendations for management. Surgery 113: 456-461.
- Noritaka O, Satoshi K, Yusei S, Kazuhiro O, Eiichi O, et al. (2000) A hemodialysed patient with parathyromatosis after total parathyroidectomy whose PTH was successful controled by percutaneous ethanol therapy and reoperation. J Jap Soc Dial Therap 36: 1267-1271.
- Unbehaun R, Lauerwald W (2007) Successful treatment with cinacalcet HCl in a patient with end-stage renal failure and refractory secondary hyperparathyroidism due to parathyromaosis. Clin Neph-rol 67: 188-192.
- Eriguchi R, Umacoshi J, Tominaga Y (2008) Successful treatment of inoperable recurrent secondary hyperpara-thyroidism with cinacalcet HCl. NDT Plus 1: 218-220.
Citation: Diaconescu MR, Glod M, Grigorovici Mirela, Smaranda D (2011) Parathyromatosis Coexisting with Papillary Thyroid Microcarcinoma. J Clinic Experiment Pathol 1:103. DOI: 10.4172/2161-0681.1000103
Copyright: © 2011 Diaconescu MR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15415
- [From(publication date): 11-2011 - Nov 24, 2025]
- Breakdown by view type
- HTML page views: 10576
- PDF downloads: 4839