Case Report Open Access
Percutaneous Endoscopic Gastrostomy and Buried Bumper Syndrome
Elias Makhoul*, Ralph Kamel, Naim Hanna and Anthony Zaarour
Department of Gastroenterology and Hepatology, University Hospital Notre Dame de Secours, Byblos, Lebanon
- Corresponding Author:
- Makhoul Elias, MD
Department of Gastroenterology and Hepatology
Faculty of Medicine and Sciences, Holy spirit University USEK
University Hospital Notre Dame De Secours
Jbeil-Byblos, BP: 3, Byblos, Lebanon
Tel: +9613711787
E-mail: eliemakhoul@hotmail.com
Received Date: July 21, 2016; Accepted Date: September 13, 2016; Published Date: September 18, 2016
Citation: Makhoul E, Kamel R, Hanna N, Zaarour A (2016) Percutaneous Endoscopic Gastrostomy and Buried Bumper Syndrome. J Gastrointest Dig Syst 6:469. doi:10.4172/2161-069X.1000469
Copyright: © 2016 Makhoul E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Percutaneous Endoscopic Gastrostomy (PEG) is a method of placing percutaneously a tube into the stomach by endoscopy. This technique is a relatively safe and effective method indicated in the treatment of neurologic diseases with irreversible swallowing problem or proximal esophageal pathology. Complications can occur including pain at the site, leakage of stomach contents and malfunction of the tube. Possible complications include infections of the PEG site, aspiration, bleeding and perforation. In this article we would like to bring to attention a rare complication of PEG, the Buried Bumper Syndrome (BBS) that presented in an 86-year-old female with gradual migration of the internal bumper alongside the stoma tract outside the stomach.
Keywords
Percutaneous endoscopic gastrostomy; Buried bumper syndrome
Case Report
An eighty-six-year-old female patient with no known past surgical history, presented to our institution for persisting swallowing disorders one month after an ischemic cerebrovascular accident.
The patient was hemodynamically stable, well conscious and oriented but she was experiencing generalized fatigue and weight loss. The decision of PEG tube placement was taken and the patient was discharged one week following the procedure without any complications.
Six months later, the patient presented to the emergency department of our institution complaining of abdominal pain that started few days prior to her presentation. The pain wasn't controlled by analgesics and was going in crescendo, and the patient started developing fever one day before.
Upon examination, the patient was febrile. On inspection of the abdomen, there was an induration with redness around the PEG tube. Her abdomen was soft with severe pain upon palpation around the indurated area. The rest of the exam was strictly normal.
The patient was admitted to the hospital, blood cultures were taken in the ER and she was put on intravenous antibiotics and symptomatic treatment. Routine blood tests showed an increased white blood cells count to 16500/mcL and a CRP level of 200 mg/dl.
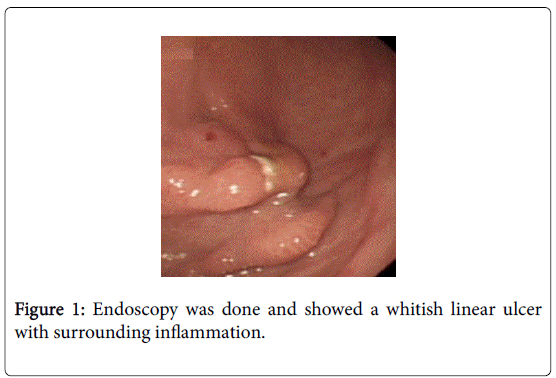
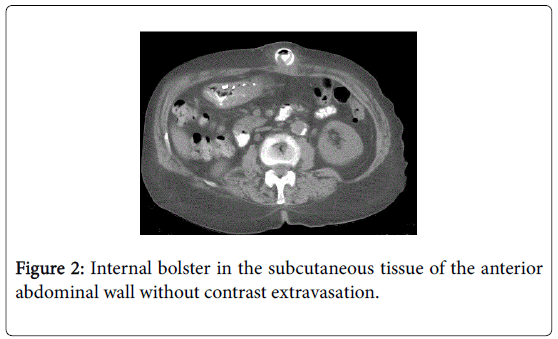
Endoscopy was done and showed a whitish linear ulcer with surrounding inflammation and no bolster was found (Figure 1). An abdominal CT scan with IV and PO contrast showed an internal bolster visualized medially at the sub-umbilical level in the subcutaneous fat in front of the rectus abdominis muscle without contrast extravasation. No hematoma or abscess or fistula was found (Figure 2).
Surgical extraction of the internal bolster was done with placement of surgical jejunostomy tube. The postoperative period was uneventful and the patient was discharged on day five.
Discussion
Percutaneous endoscopic gastrostomy (PEG) is a relatively safe and effective method of nutrition delivery, first introduced in 1980 by Gauderer and Ponsky in a pediatric population [1].
A full spectrum of consequences exists related to the PEG placement, the most frequent one being wound infection up to 40% [2]. However, the incidence of serious complications requiring specific management is only 0.4%-4.4%. These complications are generally diagnosed prior to patient discharge and include insertion site leakage with peritonitis, necrotizing fasciitis of the anterior abdominal wall, hemorrhage and laceration or perforation to internal organs [3].
Buried bumper syndrome (BBS) is a rare complication of PEG tube placement [4]. This incident occurs when the internal bolster of the PEG tube migrates along its tract and becomes trapped anywhere between the gastric wall and the abdominal skin. Most cases take place as a late complication, months to years after PEG tube placement, but many earlier cases have been reported, the shortest being six days after the procedure [5]. The reported incidence of BBS varies amongst the literature depending on quality of PEG procedures and underreporting in real life, but is typically 0.3 to 2.4% [6].
Several risk factors associated with BBS have been identified, including multiple gauze pads placement between the external bumper and the skin, excessive tube traction by patient or caregivers, and PEG tube characteristics, like a sharp tapered flange, a hard plastic composition, or a small inner bumper [4]. Gastric acid secretion also causes modification in the physical characteristics of the bumper and favors ulceration and necrosis of gastric mucosa at the bumper site [7]. Cases of BBS with the use of PEG tube with balloon catheters are extremely rare [4].
Clinical presentation of BBS varies, ranging from mild abdominal discomfort or pain, especially following feeding, inability to introduce feeds through the tube due to tube obstruction by gastric mucosa overgrowth, and peritubular leaks with outward bulging of the tube, to more serious events such as abdominal wall cellulitis, fasciitis, or abscess, peritonitis, gastrointestinal bleeding and death [8].
The diagnosis is usual made by physical exam, showing a fixed PEG tube with a palpable internal bolster and a protruding external bolster [9]. Imaging exams can be done to confirm the diagnosis or locate the exact position of the PEG tube inside the abdominal wall, such as tube series, abdominal Computerized Tomography scan, Magnetic Resonance Imaging or Ultrasound [10]. However, upper GI endoscopy is the preferred procedure to be done, since it can be used to confirm the diagnosis and as a therapeutic tool [4].
Removing the PEG tube is the mainstream treatment, along with antibiotic administration and wound care [11]. Depending on its type, the PEG tube can be removed externally with or without abdominal incision, or internally using an endoscopic snare to pull it out through the mouth [12]. Surgery is also an alternative in worse cases. If the original site is salvageable, a replacement tube can be inserted through the same tract. Otherwise, a new location should be picked for the new tube [4].
Preventive measures with patients and caregivers education are recommended to avoid this complication, such as regular wound cleaning, allowing 1 to 2 cm between the external bumper and the skin, placing the gauze pads over and not under the external bumper, and pushing the tube inside and rotating it before manipulating the external bolster [13].
Conclusion
In conclusion, endoscopists need to be aware of the spectrum of complications related to placement of the external bolster, such as the buried bumper syndrome. Attention to detail at the time of placement and careful follow-up in the period immediately following should help prevent the development of more serious sequelae. At the first sign of an adverse event or injury to the PEG tract, urgent endoscopy and the initiation of multiple therapeutic strategies should be effective in preserving the PEG site and allowing continuation of enteral feeding.
References
- Gauderer MW, Ponsky JL, Izant RJ (1980) Gastrostomy without laparotomy: a percutaneous endoscopic technique. Journal of pediatric surgery 15:872-875.
- Blumenstein I, Shastri YM, Stein J (2014) Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol 20: 8505-8524.
- McClave SA, Jafri NS (2007) Spectrum of morbidity related to bolster placement at time of percutaneous endoscopic gastrostomy: buried bumper syndrome to leakage and peritonitis. Gastrointestinal endoscopy clinics of North America 17:731-746.
- Cyrany J, Rejchrt S, Kopacova M, Bures J (2016) Buried bumper syndrome: A complication of percutaneous endoscopic gastrostomy. World J Gastroenterol 22: 618-627.
- Khalil Q, Kibria R, Akram S (2010) Acute buried bumper syndrome. South Med J 103: 1256-1258.
- Venu RP, Brown RD, Pastika BJ, Erikson LW (2002) The buried bumper syndrome: a simple management approach in two patients. Gastrointestinal endoscopy 56:582-584.
- Foutch PG, Woods CA, Talbert GA, Sanowski RA (1988) A critical analysis of the Sacks-Vine gastrostomy tube: a review of 120 consecutive procedures. Am J Gastroenterol 83: 812-815.
- Tsai JJ, Lin HJ (2009) Clinical manifestations and management of buried bumper syndrome in patients with percutaneous endoscopic gastrostomy. Gastrointestinal endoscopy 69: 1193.
- Gençosmanoglu R, Koç D, Tozün N (2003) The buried bumper syndrome: migration of internal bumper of percutaneous endoscopic gastrostomy tube into the abdominal wall. Journal of gastroenterology 38: 1077-1080.
- Krull CM, Dennison AC (2016) A Case Series: The Identification of Buried Bumper Syndrome With Abdominal Computed Tomography Scan in Two Severely Brain Injured Rehabilitation Patients.
- Geer W, Jeanmonod R (2013) Early presentation of buried bumper syndrome. West J Emerg Med 14: 421-423.
- Biswas S, Dontukurthy S, Rosenzweig MG, Kothuru R, Abrol S (2014) Buried bumper syndrome revisited: a rare but potentially fatal complication of PEG tube placement. Case Rep Crit Care 2014: 634953.
- Delegge MH (2015) Gastrostomy tubes: Complications and their management.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12844
- [From(publication date):
October-2016 - Sep 23, 2024] - Breakdown by view type
- HTML page views : 12139
- PDF downloads : 705