Case Report Open Access
“A Cystic Mass in the Head of the Pancreas” Case Report of Schwannoma
Saleg Patricia1*, Alcaraz Alvaro1, Romero Eugenia1, Roussy Guillermo1 and Maraschio Martin2
1Department of General Surgery, Private Hospital of Cordoba, Argentina
2Chief of Liver Transplantation, Private Hospital of Cordoba, Argentina
- *Corresponding Author:
- Patricia Saleg
Department of General Surgery
Private Hospital of Cordoba, Argentina
E-mail: patosaleg_08@hotmail.com
Received date: March 16, 2013; Accepted date: May 06, 2013; Published date: May 08, 2013
Citation: Patricia S, Alvaro A, Eugenia R, Guillermo R, Martin M (2013) “A Cystic Mass in the Head of the Pancreas” Case Report of Schwannoma. J Gastroint Dig Syst S3:006. doi: 10.4172/2161-069X.S3-006
Copyright: © 2013 Patricia S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
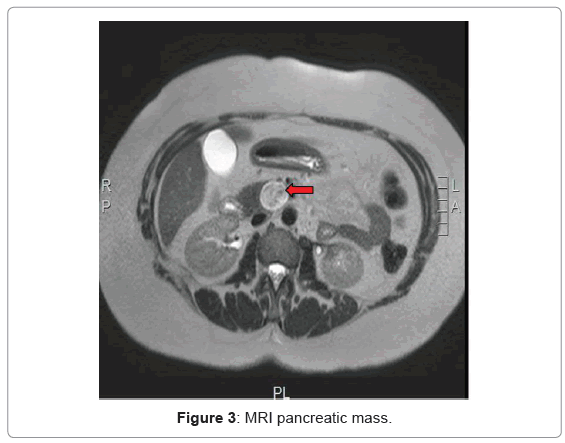
We report a case of a female (61 years) who presented with unspecific abdominal symptoms which motivated us a scan. This showed a cyst in the head of the pancreas. An abdominal CT scan confirmed the presence of a cystic tumor in the uncinated process of the pancreas measuring 27 mm in diameter, and nonspecific lymphadenopathy over the hepatic hilum. A MRI showed findings consistent with a Mucinous Cystic Neoplasia (MCN) at the pancreatic head. A pancreaticoduodenectomy was performed with excellent postoperative course, being the patient discharged from the hospital on POD 10. Pathological analysis showed a duodenal schwannoma of 31 × 24 mm (S-100 protein positive, CD 117 negative). No further treatment was indicated.
Keywords
Pancreatic schwannoma; Duodenal schwannoma; Pancreatic mass; Pancreaticoduodenectomy; Pancreatic cyst
Introduction
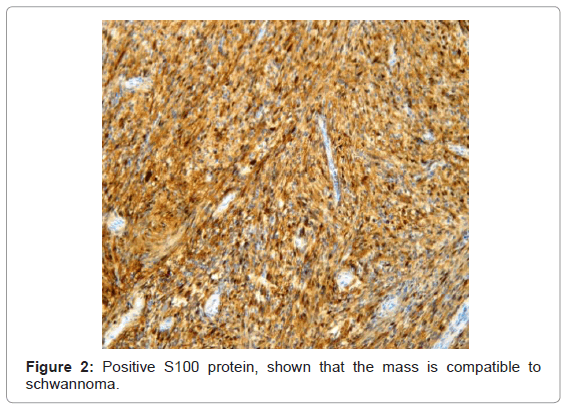
Small bowel tumors are rare, representing 3% of all gastrointestinal malignancies [1]. Less than 30% of these tumors are found in the duodenal region. Gastrointestinal schwannomas are extremely rare neoplasms that represent less than 1% of all gastrointestinal tract neoplasms [2,3]. Schwannomas usually occur in the extremities, but can also be found in the trunk, head and neck, retroperitoneum, mediastinum, pelvis and rectum. Among the GI tract, they occur most commonly in the stomach (60-70% of cases), followed by the colon and rectum in frequency. The location in the esophagus or duodenum is extremely rare. Most schwannomas are benign tumors [4]. Incidence in males almost equals females, presenting most frequently within the fifth or sixth decade of life. Immunohistochemistry plays a central role in the diagnosis of schwannoma being positive for protein S-100 protein. Radical excision with free margins (R0) offers the best curative chance.
The authors consider the present case as important because there are few literatures about this neoplasia that are very uncommon. The authors conclude that pancreatic schwannomas should be considered in the differential diagnosis of cystic neoplasms of the pancreas, although the diagnosis can only be confirmed by microscopic examination.
Clinical Case
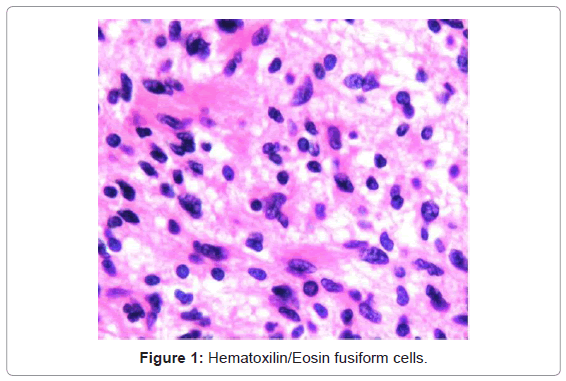
Female patient aged 61 with a history of hypertension, hypothyroidism and obesity presents in the clinic with dyspepsia and irritable bowel syndrome starting several months earlier. Physical examination was unremarkable and lab tests were within normal limits. An abdominal US showed a cyst in the pancreas head, which could not be characterized, and a lymphadenopathy in the hepatic hilum, measuring 40 mm in diameter (Figure 1). An abdomen CT scan confirmed the lymphadenopathy and the cyst in the pancreas uncinated process, 27 mm in diameter. A MRI with cholangiography showed that the cyst had well-defined walls, had slightly heterogeneous content and in turn small cyst inside of 9 mm findings most compatible with a mucinous cystadenoma (Figure 3). A pancreaticoduodenectomy was performed. A mass in the head of the pancreas was found. The postoperative course was unremarkable; being the patient discharged 10 days after the surgery. The histological analysis showed a duodenal schwannoma of 31 × 24 mm in diameter. We perform an inmunohistochemical analysis to differentiate schwannoma from the gastrointestinal stromal tumor. Immunohistochemistry S-100 protein positive (Figure 2), CD 117 negative compatible to schwannoma.
Discussion
Schwannomas are rare tumors arising from Schwann cells that cover the peripheral nerves, and are difficult to differentiate from leiomyomas. Schwannomas usually occur in the extremities, but can also be found in the trunk, head and neck, retroperitoneum, mediastinum, pelvis and rectum. Schwannomas of the gastrointestinal tract have distinct histological features that differentiate them from other schwannomas [5,6]. Gastrointestinal schwannomas occur most commonly in the stomach (60-70% of cases), followed by the colon and rectum in frequency. Schwannomas of the esophagus, pancreas and duodenum are extremely rare. Most present within the second or third portion of the duodenum or in the head of the pancreas rarely in the rest of the pancreas. They usually occur within the fifth and sixth decade of life, as it presented in our case. Sex distribution is equal [7]. Schwannomas in the pancreas may be asymptomatic for years and the symptoms are usually nonspecific, as it happened in our patient. However, some cases may present with pain, intestinal bleeding or bowel obstruction if the mass grows faster and compresses the second porcion of duodenum. Pancreas tumors usually present a cystic morphology in the CT and MRI scans, mimicking pancreatic mucinous cystadenomas or cystadenocarcinoma [8,9]. Histologically, gastrointestinal schwannomas are spindle cell tumors with a pattern of microtrabecular, peripheral lymphoid cuffs, and occasionally germinal centers, usually not showing a nuclear palisading pattern as often presents conventional schwannomas, and are histologically S-100 positive as in this case. Moreover, it has been recently shown that gastrointestinal schwannomas lack genetic alterations, supporting the theory that this variety of schwannomas is different from conventional schwannomas [10]. It is believed that they arise in the myenteric plexus because of its immunophenotypical similarities. Both schwannomas and myenteric plexus cells expressed positivity for S-100 protein and glial fibrillary acidic protein. Gastrointestinal schwannomas are benign tumors which rarely undergo malignant transformation and mostly have an excellent prognosis after surgical resection with free margins. These tumors vary considerably in size and about two thirds may undergo degenerative changes including cysts inside, calcification, hemorrhage, hyalinization and xanthomatous infiltration.
Conclusion
The pancreatic schwannoma is very rare, but an important pathological condition. It should be considered in the differential diagnosis of cystic neoplasms of the pancreas, although the diagnosis can only be confirmed by microscopic examination. The surgical approach depends mainly on tumor size and location, and eventually histologic features. The response to chemotherapy and radiation therapy remains uncertain.
References
- Almo KM, Traverso LW (2001) Pancreatic schwannoma: an uncommon but important entity. J Gastrointest Surg 5: 359-363.
- Dorsey F, Taggart MW, Fisher WE (2010) Image of the month. Pancreatic schwannoma. Arch Surg 145: 913-914.
- Mummadi RR, Nealon WH, Artifon EL, Fleming JB, Bhutani MS (2009) Pancreatic Schwannoma presenting as a cystic lesion. Gastrointest Endosc 69: 341.
- Wu YL, Yan HC, Chen LR, Chen J, Gao SL, et al. (2005) Pancreatic benign schwannoma treated by simple enucleation: case report and review of literature. Pancreas 31: 286-288.
- Novellas S, Chevallier P, Saint Paul MC, Gugenheim J, Bruneton JN (2005) MRI features of a pancreatic schwannoma. Clin Imaging 29: 434-436.
- Feldman L, Philpotts LE, Reinhold C, Duguid WP, Rosenberg L (1997) Pancreatic schwannoma: report of two cases and review of the literature. Pancreas 15: 99-105.
- Burd DA, Tyagi G, Bader DA (1992) Benign schwannoma of the pancreas. AJR Am J Roentgenol 159: 675.
- Weiss SW, Langloss JM, Enzinger FM (1983) Value of S-100 protein in the diagnosis of soft tissue tumors with particular reference to benign and malignant Schwann cell tumors. Lab Invest 49: 299-308.
- Barcena Barros JM, Manuel Palazuelos JC, Concha García A, Val Bernal JF, Naranjo Gómez A, et al. (1988) Benign schwannoma of the pancreas. Rev Quir Esp 15: 158-159.
- Rösch T, Kapfer B, Will U, Baronius W, Strobel M, et al. (2002) Accuracy of endoscopic ultrasonography in upper gastrointestinal submucosal lesions: a prospective multicenter study. Scand J Gastroenterol 37: 856-862.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13988
- [From(publication date):
specialissue-2013 - Nov 10, 2025] - Breakdown by view type
- HTML page views : 9329
- PDF downloads : 4659