Research Article Open Access
Hyperbilirubinemia in Patients with Amoebic Liver Abscess: A Study of 75 Cases
Anil Kumar Sarda1, Anurag Mishra1*, Navdeep Malhotra1 and Alpana Manchanda2
1Department of Surgery, Maulana Azad Maulanian College, New Delhi, India
2Department of Radiodiagnosis, Maulana Azad Maulanian College, New Delhi, India
- *Corresponding Author:
- Anurag Mishra
Department of Surgery
Maulana Azad Maulanian College
New Delhi, India
E-mail: anurag.alok@gmail.com
Received date: July 22, 2013; Accepted date: September 11, 2013; Published date: September 13, 2013
Citation: Anil Kumar S, Anurag Mishra, Navdeep Malhotra, Alpana M (2013) Hyperbilirubinemia in Patients with Amoebic Liver Abscess: A Study of 75 Cases. J Gastroint Dig Syst 3:138. doi:10.4172/2161-069X.1000138
Copyright: © 2013 Anil Kumar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Hyperbilirubinemia is a frequent occurrence in patients with amoebic liver abscess (ALA). Despite this, the cause of jaundice has not been established. It is presumed to be either due to parenchymal destruction or due to cholestatis due to pressure on the intrahepatic bile ducts by the abscess cavity or a combination of both. Aim: The present study is designed to study the incidence and the cause of hyperbilirubinemia in patients with ALA. Settings and design: prospective randomized controlled study Methods and material: Study was performed in a tertiary care centre with high volume of patients of liver abscesses. We evaluated 75 patients of liver abscess from December 2008 to March 2010 and based on presence or absence of hyperbilirubinemia, divided into Group I (serum bilirubin ≥ 1 mg/dl) and Group II (serum bilirubin <1 mg/dl). After detailed evaluation, both the Groups were compared on basis of parameters like clinical symptoms (e.g. fever, pain), alcohol intake, leucocytosis, bilirubin levels, liver enzymes, size of cavity, and response to treatment. Statistical analysis used: Chi square test/ Fischer’s exact test was used for qualitative data, and for quantitative data, t-test/Mann Whitney test was used. Results: In this study, we found hyperbilirubinemia in 23 of total 75 ALA patients with incidence of 30.7%. Overall the serum bilirubin values ranged from 0.4 to 11.7 mg/dl (mean=1.551) whereas in group 1 it ranged from 1.3 to 11.7 mg/dl (mean=3.71). The high values of bilirubin were associated with elevated alkaline phosphatase enzyme in 21 of 23 cases (91.3%) however significant biliary radical dilatation could not be found. The Jaundice responded well to the drainage of abscess cavity. Conclusions: Hyperbilirubinemia occurs frequently in cases of amoebic liver abscess which seems to obstructive in nature and it can be treated by surgical drainage of the abscess cavity. Further large volume and more detailed studies are needed to confirm the findings.
Keywords
Amoebic liver abscess (ALA); Hyperbilirubinemia; Jaundice; Obstructive
Introduction
Liver abscess is a common problem in India and is associated with high morbidity and mortality. The incidence of amoebic liver abscess has been reported to vary between 3% and 9% of all cases of amoebiasis, which is found in up to 20% of Indian population. In India, the occurrence of amoebic liver abscess is endemic. Although colonic amoebae are mainly responsible for the development of abscess but most patients with abscess do not have coexistent amoebic colitis. Jaundice in patients with amoebic liver abscess is a frequent occurrence. Its incidence varies between 6% and 29% [1-4]. During the course of illness, one-third of the patients may develop clinical jaundice. The cause of jaundice in patient with amoebic liver abscess has not yet been established. It is thought to be either due to secondary infection of ALA, or pressure of the abscess on hepatic ducts, while other views are that it is due to parenchymal destruction or cholestatic in nature [1,2,5,6]. This study was designed to study the incidence and the actual cause of hyperbilirubinemia in patients with amoebic liver abscess.
Materials and Methods
This study was designed as randomized prospective study and a formal prior approval was taken from the hospital ethical committee. The study was conducted in one surgical unit of a tertiary care hospital, between December 2008 and March 2010 (15 months duration), where 75 patients of amoebic liver abscess (sample size was calculated by using 95% as confidence level and 6% as incidence of ALA with Jaundice) as diagnosed on clinical examination and ultrasonography, were assessed and their clinical history, examination findings, biochemical investigations including amoebic serology and sonographic evidence were recorded on a predetermined Performa. ALA was differentiated from pyogenic abscess on basis of clinical history of no high grade fever, amoebic serology and ultrasound appearances. Patients were thoroughly explained about the study and an informed consent was taken. Any patient with jaundice due to other causes including choledocholithiasis, drug induced or viral hepatitis, stricture and other causes of extra hepatic biliary pathology were excluded from the study. Finally the selected cases were divided into two Groups on the basis of their serum bilirubin levels. Study Group I included patients having hyperbilirubinemia (serum bilirubin ≥ 1 mg/dl) while Group II patients having serum bilirubin levels <1 mg/dl. In addition, cases of Group I also underwent magnetic resonance cholangio-pancreatography (MRCP). All cases were admitted and started on anti-amoebic treatment along with broad spectrum antibiotics and the response was recorded based on improvement in clinical finding, leucocytosis, liver function tests and ultrasonography. In all the Group I cases, percutaneous therapeutic drainage of abscess cavity was performed using pigtail catheter while in Group II, cases with failure of conservative treatment or high risk abscesses (cavity diameter more than five centimeters, lesion near porta hepatis, <10 mm rim of tissue around the abscess) were managed with percutaneous drainage. In such cases the aspirated pus was examined and cultured. The outcomes in terms of resolution of abscess on the basis of ultrasonography and air cavitogram were assessed. The cases were also assessed on basis of the cavity size with reference set at 400 cc, which is the size which warrants surgical drainage as per our protocols.
Statistical analysis
Data was evaluated using Chi square test/ Fischer’s exact test for qualitative data and, t-test/Mann Whitney test for quantitative data.
Results
In the 75 patients under study (67 males, 8 females; M:F=9:1) the mean age was 41.84 years (range 20-65 years). Of these 23 patients (30.7%) had hyperbilirubinemia (total bilirubin ≥ 1 mg/ dl).
All female patients belonged to Group II. Presence of symptoms like fever and abdominal pain was not found to be statistically different in two Groups (n=1.3). Out of 75 patients, 56 patients (74.7%) had history of alcohol intake; all of these patients were males. The ratio was 95.6% in Group I with 22 of 23 cases were found to have history of alcohol intake which was significantly more than Group II.
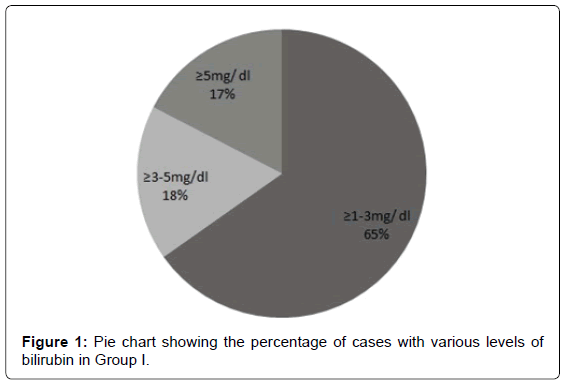
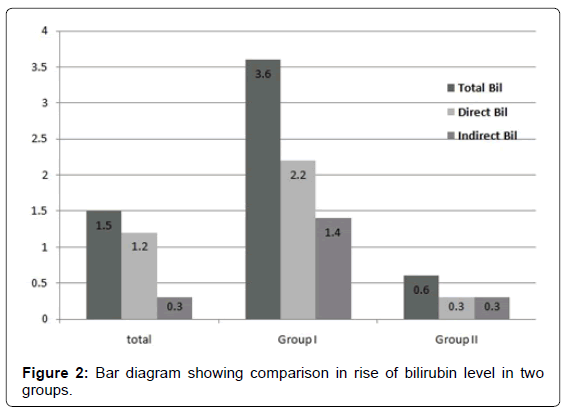
Overall about two-third patients (48 of 75) showed leucocytosis, but the ratio was 95.3% in Group I which was significantly higher than Group II (p=0.000).Serum bilirubin level ranged from 0.4 to 11.7 mg/dl (mean=1.551). Amongst Group I, 15 cases had serum bilirubin level ≥ 1-3 mg/dl (65.21%), four cases had serum bilirubin >3-5 mg/dl (17.4%) and four cases had serum bilirubin >5 mg/dl (17.4%) (Figure 1). In Group I patients, it ranged from 1.3 to 11.7 mg/dl and direct bilirubin was more than the indirect bilirubin in most of the patients (Figure 2). Clinically, icterus was detected in 19 of these patients (25.33%).
Hyperbilirubinemia was found to have positive correlation with size of cavity as eleven patients (47.8%) of Group I had size of the cavity >400 c.c. while only 6 (26.1%) patients had size <200 c.c. and remaining six patients had size of the cavity 200-400 c.c. (26.1%). On other hand in Group II, only 13 patients had size of the cavity >400 c.c (25%) (Table 1).
| Size of the abscess cavity | |||
|---|---|---|---|
| <200 c.c. | 200-400 c.c. | >400 c.c. | |
| Group I (n=23) | 6 26.1% | 6 26.1% | 11 47.8% |
| Group II (n=52) | 13 25% | 23 44.2% | 16 30.8% |
Table 1: Table comparing cavity sizes in two groups.
The serum alkaline phosphatase (SAP) ranged from 78 units to 2765 units (mean=331.19) and 43 (57.33%) patients showed raised values out of which 21 were in Group I (91.3%) and 22 in Group II (42.3%). The mean values of SAP were 540.35 and 238.67 in Group I and II respectively. The difference was found to be significant statistically (p=0.000). In all patients with size of the cavity >400 c.c. (n=24), SAP was raised (100%) while patients with cavity size 200-400 c.c. (n=22) had raised SAP in 18 patients (81.18%) and 16 patients (55.17%) had raised SAP in patients with size of cavity <200 c.c. (n=29). The size of the cavity directly correlated with hyperbilirubinemia as well as with raised SAP levels.
Eleven patients (47.8%) had raised alkaline aminotransferase (ALT) while nine patients (39.1%) had raised aspartate aminotransferase (AST) in Group I. On the other hand, eight patients (15.4%) had raised ALT and 10 patients (19.2%) had raised AST in Group II. Prothrombin time was deranged only in 5 patients requiring vitamin K therapy while FFP was required in one patient.
MRCP was performed in 22 patients out of 23 who had hyperbilirubinemia. In one patient, it was technically not possible because the patient was claustrophobic and restless. Although intrahepatic biliary radical dilatation was seen only in one patient in which MRCP was performed but there was proximity of the abscess to the main biliary ducts in 15 patients. It was seen that 50% (11) patients had cavity size >10 cm and 68.1% (n=15) had abscess cavity near porta hepatis involving segment 1/5/6/7 and multiple segments were involved in n=16 patients (Table 2).
| MRCP findings | No. Of cases (n=22) | Percentage |
|---|---|---|
| IHBR dilatation | 1 | 4.5% |
| CBD attenuated but no IHBR dilatation | 1 | 4.5% |
| IHBR not dilated | 20 | 90.9% |
| Abscess cavity near porta hepatis involving segment 1/5/6/7 | 15 | 68.1% |
| Abscess cavity of large size (>10 cm) | 11 | 50% |
| Multiple abscesses | 12 | 52.2% |
Table 2: Table showing MRCP findings in cases with jaundice.
More than half of cases in Group I (52.2%) showed multiple liver abscesses whereas this number was only 30.8% in Group II (p=0.077). Caudate lobe involvement was seen in two of 23 Group I cases and none of 52 Group II cases. Frequency of complications like rupture in peritoneal cavity were seen in 26.1% patients (n=6) of Group I, while in Group II, it was present only in 3.8% (n=2) cases (Table 3).
| Segments involved | n (%) |
|---|---|
| Segment 1 | 2 (9) |
| Segment 2/3/4 | 5 (22.7) |
| Segment 5/6/7 | 15 (68.18) |
| Segment 8 | 8 (36.36) |
Table 3: Table showing frequency of involvement of various segments.
Medical treatment was started in all patients with broad spectrum antibiotics and metronidazole. Out of 75 patients, 12 responded only to medical management without any surgical intervention. Of these, 11 patients belonged to Group II while only one patient belonged to Group I in whom abscess was in caudate lobe of the liver where access to the abscess cavity was not easy, so percutaneous drainage could not be done. Otherwise in Group I patients, the mainstay of treatment was drainage of abscess done either by ultrasound guided needle aspiration (n=2) or by pigtail catheter insertion (n=20).
Amongst patients with jaundice, 21 improved symptomatically by becoming afebrile, with relief of pain and fall in serum bilirubin levels. There was fall in serum ALP, AST, ALT levels in all patients. Leukocyte counts also decreased in these patients corresponding with clinical improvement. The size of the abscess cavity decreased in all patients after treatment which was documented on ultrasound examination and air cavitogram. Two patients failed to respond and expired.
Discussion
Hyperbilirubinemia is quite common in patients with ALA but the frequency and depth vary. The incidence of jaundice in patients with ALA varies between 6% and 29% [1-4]. Ramachandran et al. [7] reported 137 cases of ALA in which jaundice was seen in 11 patients only (8%), out of which 9 patients had serum bilirubin 2-5mg/ dl and two patients had Serum bilirubin >5 mg/dl. Whereas Sharma and Sarin [8] reported 70 cases of ALA with 33% incidence of jaundice. In our study, 30.7% patients had hyperbilirubinemia out of which four had serum bilirubin >5 mg/dl, four had serum bilirubin in 3-5 mg/dl range and 15 patients had serum bilirubin in 1-3 mg/dl range. Clinically icterus was seen in 25.33% patients.
The mechanism of hyperbilirubinemia in ALA has been studied previously in many studies [2,6]. Various mechanisms were suggested like pressure on biliary ducts at the porta hepatis especially by large abscess [2,7]. Sharma et at observed that jaundice occurs because of intrahepatic obstruction or associated hepatitis and is usually seen in large or multiple abscesses; abscess situated at porta hepatis is more likely to produce jaundice because of extra-hepatic obstruction [8].
In our study, the site and size of ALA was assessed by MRCP in Group I patients. It was seen that 50% (n=11) patients had large cavity size >10 cm or >400 cc. Many studies have shown earlier that larger size of liver abscess is associated with jaundice. This relation of cavity size and jaundice has also been confirmed by necropsies and therefore, the main cause of jaundice in ALA is postulated to be the pressure and distortion of the biliary tree resulting in intrahepatic cholestatis. Drainage of these large abscesses leads to significant improvement of the laboratory parameters including the serum bilirubin, serum ALP, ALT, AST as well as leukocyte count in three to seven days.
Nigam et al. [2] reported that jaundice is more commonly associated with multiple ALA while Sharma and Sarin [8] reported association of right lobe liver abscess to be more common with jaundice. Nigam also observed that abscesses near the inferior surface are more common in patients with hyperbilirubinemia. In our study, the frequency of multiple liver abscesses was more in cases with jaundice (52.2%) as compared to those without jaundice (30.8%). MRCP was performed in Group I patients which showed that in majority of patients (68.1%), the location of cavities were central and in proximity of the main biliary ducts/porta hepatis causing compression of the ducts with or without IHBR dilatation. These were present in right lobe involving segment 5/6/7 or caudate lobe (segment 1). As a fact all cases with caudate lobe involvement were found to have hyperbilirubinemia. When other segments like segment 8 (which is anterolateral to the right branch of portal vein in right lobe) or segments 2, 3, 4a, 4b (left lobe) were involved, there was lesser incidence of jaundice as these are comparatively far away from the porta hepatis.
In the 75 patients under review, serum alkaline phosphatase ranged from 78 units to 2765 units (mean=331.19). In patients in Group I, ALP was raised (ranging from 109 to 2765 with a mean value of 540.35 units) in 91.3% patients (n=21). In Group II patients, ALP value range from 78 to 868 units (mean=238.67 units) and ALP was raised in 42.3% patients (n=22) {p=0.000, statistically significant}. Earlier reports showed raised ALP in 76% cases of amebic liver abscess [9]. High ALP levels may be seen in 60-80% cases of amebic liver abscess. The average ALP level had been reported to be 24 KA units. It returned to normal after resolution of the abscess [4]. In our study, we also found a correlation between ALP, size of the cavity and bilirubin levels. In all patients with size of the cavity >400 c.c. (n=24), serum ALP was raised (100%). Patients with size 200-400 c.c. (n=22) had raised ALP in 18 patients (81.18%). While 16 patients (55.17%) had raised ALP in patients with size of cavity <200 c.c. (n=29). So, it was observed that increase in the size of the cavity correlates with hyperbilirubinemia as well as with raised ALP levels suggesting the obstructive pathology. This fact was further proven by the decrease in the ALP levels in all patients after drainage of the abscess even before the bilirubin levels came down.
This study tries to find out the likely cause of jaundice and its actual incidence in ALA cases in a scientific manner. All patients in the study were followed as in patients, thus reducing the dropout rate to nil. It also enabled us to follow the trends of jaundice with clinical and radiological improvements. Though the number of 75 cases of ALA with jaundice is small to quote true incidence, it is significant enough to realize to expect and investigate patients of ALA for possible jaundice. Further systematic reviews are needed with higher number of cases to finally establish the cause and management of such patients.
Summary and Conclusion
In conclusion, 30.7% of the patients under review had hyperbilirubinemia the cause of which in our observation was obstruction. Despite the fact that there was no radiological evidence of obstruction, this was indicated by high ALP and very early reversal to normal bilirubin levels after rupture of the abscess or drainage. Further evidence is of the fact that large abscesses especially those near the main bile ducts are more prone to cause hyperbilirubinemia. On the basis of our study, we advocate drainage of ALA along with the institution of medical therapy at the outset of all the abscesses more than 400 c.c. and in those associated with complications even if size is less.
References
- Singh V, Bhalla A, Sharma N, Mahi SK, Lal A, et al. (2008) Pathophysiology of jaundice in amoebic liver abscess. Am J Trop Med Hyg 78: 556-559.
- Nigam P, Gupta AK, Kapoor KK, Sharan GR, Goyal BM, et al. (1985) Cholestasis in amoebic liver abscess. Gut 26: 140-145.
- Hughes MA, Petri WA Jr (2000) Amebic liver abscess. Infect Dis Clin North Am 14: 565-582, viii.
- Gupta RK, Pant CS (1986) Ultrasound demonstration of amoebic liver abscess causing obstructive jaundice. Australas Radiol 30: 329-331.
- Sarda AK, Kannan R, Gupta A, Mahajan V, Jain PK, et al. (1998) Amebic liver abscess with jaundice. Surg Today 28: 305-307.
- Datta DV, Chhuttani PN (1971) Cholestasis in patients with amoebic liver abscess. Am J Dig Dis 16: 977-984.
- Ramachandran S, Goonatillake HD, Induruwa PA (1976) Syndromes in amoebic liver abscess. Br J Surg 63: 220-225.
- Sharma MP, Sarin SK (1987) Amoebic liver abscess in a North Indian hospital--current trends. Br J Clin Pract 41: 789-793.
- Khanna S, Chaudhary D, Kumar A, Vij JC (2005) Experience with aspiration in cases of amebic liver abscess in an endemic area. Eur J Clin Microbiol Infect Dis 24: 428-430.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 19134
- [From(publication date):
October-2013 - Dec 22, 2025] - Breakdown by view type
- HTML page views : 14224
- PDF downloads : 4910