Review Article Open Access
Management of Non Variceal Upper Gastrointestinal Bleed
Sherif Safwat*
Mid Essex Health Authority, UK
- *Corresponding Author:
- Sherif Safwat
Mid Essex Health Authority, UK
E-mail: Sherif.Safwat@meht.nhs.uk
Received date: March 08, 2013; Accepted date: March 31, 2013; Published date: April 02, 2013
Citation: Safwat S (2013) Management of Non Variceal Upper Gastrointestinal Bleed. J Gastroint Dig Syst S3:004. doi:10.4172/2161-069X.S3-004
Copyright: © 2013 Safwat S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Upper gastrointestinal bleeding has 10% in-hospital mortality. Despite significant advances in the management, there has not been any improvement in mortality. The only improvement over the last 25 years has been in variceal bleeds. Increasing age and comorbidities are the major factors related to mortality. Early endoscopic management of severe upper GI bleeds improves survival. Adopting a system which identifies severe bleeding and vulnerable patients is essential.
Keywords
GI Bleeds; Variceal; Haematemesis; Comorbidities
Scores to Identify High Risk and Low Risk Patients
The various scoring systems aim to identify significant bleeds and patients with comorbidities that would worsen the outcome [1-7] (Table 1).
| Glasgow-Blatchford Score | |
|---|---|
| Admission risk marker | Score component value |
| Blood Urea | |
| ≥ 6.5 <8.0 | 2 |
| ≥ 8.0 <10.0 | 3 |
| ≥ 10.0 <25.0 | 4 |
| ≥ 25 | 6 |
| Haemoglobin (g/L) for men | |
| ≥ 12.0 <13.0 | 1 |
| ≥ 10.0 <12.0 | 3 |
| <10.0 | 6 |
| Haemoglobin (g/L) for women | |
| ≥ 10.0 <12.0 | 1 |
| <10.0 | 6 |
| Systolic blood pressure (mm Hg) | |
| 100-109 | 1 |
| 90-99 | 2 |
| <90 | 3 |
| Other markers | |
| Pulse ≥ 100 (per min) | 1 |
| Presentation with melaena | 1 |
| Presentation with syncope | 2 |
| Hepatic disease | 2 |
| Cardiac failure | 2 |
A score of 6 or more is associated with a greater than 50% need for intervention, while a score of zero means that hospitalization is not required [7].
Table 1: Glasgow-Blatchford Score.
Rockall Score
The two scoring systems are useful in identifying the high and low risk patients, but clinical judgment is superior [8-10]. It is also worth noting that GI bleeding in inpatients has a three folds increase in mortality [11-12]. So in general a patient who has a witnessed haematemesis or melena in hospital has a significant bleed and requires special attention. A systolic blood pressure below 100 a heart rate above 100 per minute, Haemoglobin level below 10 gm/dl and a high urea in a bleeding patient should alert you that an early endoscopic intervention is warranted (Table 2).
| Variable | Score 0 | Score 1 | Score 2 | Score 3 |
|---|---|---|---|---|
| Age | <60 | 60- 79 | >80 | |
| Shock | No shock | Pulse >100 | SBP <100 | |
| BP >100 | ||||
| Systolic | ||||
| Co-morbidity | Nil major | CHF, IHD, major morbidity | Renal failure, liver failure, metastatic cancer | |
| Diagnosis | Mallory-Weiss | All other diagnoses | GI malignancy | |
| Evidence of bleeding | None | Blood, adherent clot, spurting vessel |
8 points put patient in high risk, while 2 points or less is low risk.
Table 2: Rockall score.
Preparing the Patient for Endoscopic Intervention
Resuscitation of the haemodynamically unstable patient with gastrointestinal bleeding is vital, particularly if they are elderly or have comorbidities. There are certain issues with bleeders that should be highlighted:
1. Avoid overzealous filling of your patient. As any good plumber would tell you, the first rule of good plumbing; before fixing the leak you need to switch off the main water supply. Aim to keep the systolic BP at 100 mmHg and Hemoglobin at 7 gm/ dl [13]. These patients are better treated in specialized or high dependency units, particularly the vulnerable elderly and patients with co-morbidities. If variceal bleed is suspected Portal pressure (Hepatic venous pressure gradient) should be reduced by the use of Terlipressin or somatostatin [14,15].
2. Correct significant clotting disorders.
3. Decide on the place for endoscopy and the support required: either A&E, operating theatre, endoscopy unit or ITU. This depends on what is available in your hospital, the risk of aspiration and the availability of specialist endoscopy nurses.
4. Patients with suspected variceal bleed benefit from prophylactic antibiotics as it improves mortality [16-18].
5. Intravenous proton pump inhibitor: This should be given in serious GI bleeds; 80 mg IV pantoprazole stat followed by 8 mg per hour for 72 hours or40 mg qds. There is controversy about the use of ppi prior to endoscopic therapy of non variceal GI bleed. Although it does not improve mortality, it is associated with significant down staging of endoscopic lesions [19,20].
6. IV Erythromycin prior to endoscopy improves visibility during endoscopy [21].
Endoscopic Management
Bleeding peptic ulcer
Two sites in the upper GI tract are associated with significant bleeds due to anatomical proximity to arteries. Posterior wall of first part of duodenum from gastrodudenal artery and proximal lesser curve of stomach from left Gastric artery.
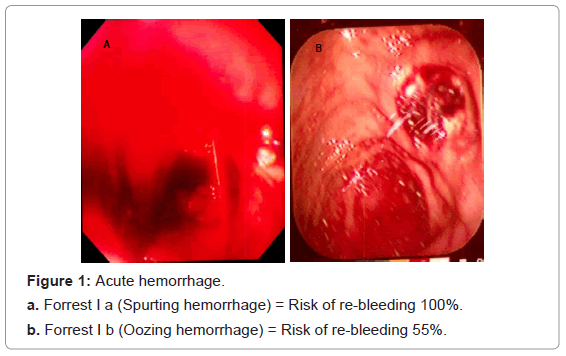
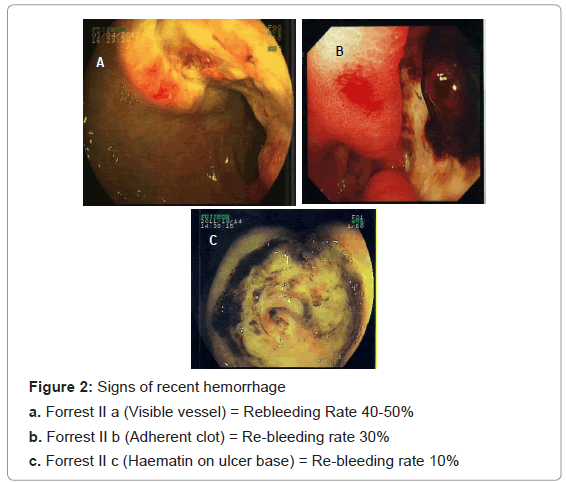
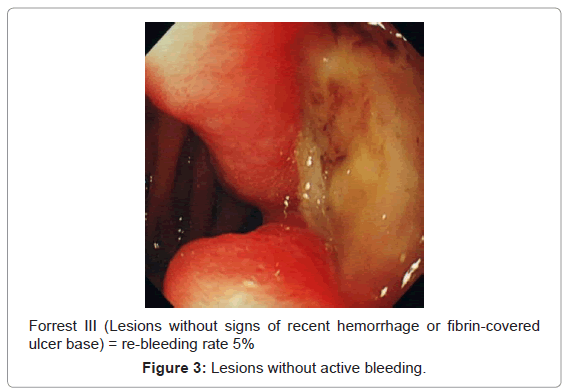
There are several endoscopic features that give indication to the seriousness of the bleed and the risk of re-bleeding. The Forrest classification describes various degrees of bleeding from ulcers and the re-bleeding risk associated. Other factors associated with failure of haemostasis are ulcer size, presence of shock at presentation and previous ulcer bleeding.
Forrest classification [22]
(Figure 1) (Figure 2) (Figure 3)
Strategies for a successful endoscopic haemostasis
Keeping the systolic blood pressure at around 100 mmHg and restricting the use of blood transfusions unless the Haemoglobin is 7 gms or less gives the endoscopist an advantage with a less bloody field, allows for better visualization of the ulcer field and improves survival [23].
Three modalities are available to control ulcer bleeding; adrenaline (1:10000) injection, Heat probe and clips. Adrenaline injection, although not proven to improve survival as a single modality, it is a very useful temporary method to control the bleeding by both its tamponade effect and vasoconstriction [24]. If a visible vessel is seen it can be tackled by either heat probe or clip without prior adrenaline injection. When a clot is seen, injecting adrenalin at the base of the ulcer, around the clot loosens it, and it can be washed off by water spray. If the clot does not wash away, you may shave it off using a snare. Once the clot is dislodged any visible vessel should be dealt with either with heat probe or clip. Attempts should be repeated till you can see a clean ulcer base.
Surgical treatment would be required if endoscopic intervention fails to stop the bleeding. Information regarding the site of bleeding is important to be passed on to the surgeon. In case of failure to identify the bleeding point triple phase CT angiography is required and interventional angiography can be used to control the bleeding.
After successful treatment of a bleeding peptic ulcer, gastric ulcer patients should be re-scoped in 6 weeks to ensure healing. Duodenal ulcer patients do not require re-scoping but they would benefit from H pylori eradication.
Other Causes of Upper GI Bleed
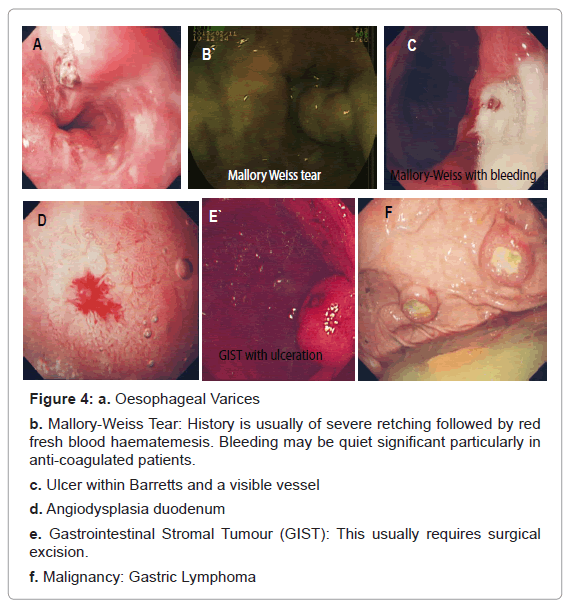
(Figure 4 (a-f))
Figure 4: a. Oesophageal Varices
b. Mallory-Weiss Tear: History is usually of severe retching followed by red
fresh blood haematemesis. Bleeding may be quiet significant particularly in
anti-coagulated patients.
c. Ulcer within Barretts and a visible vessel
d. Angiodysplasia duodenum
e. Gastrointestinal Stromal Tumour (GIST): This usually requires surgical
excision.
f. Malignancy: Gastric Lymphoma
Conclusion
Management of the upper GI bleed should not be perplexing as long as you are well prepared. As Billy Connelly said ‘There is no such thing as bad weather, only bad clothes’.
References
- Carbonell N, Pauwels A, Serfaty L, Fourdan O, Lévy VG, et al. (2004) Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology 40: 652-659.
- Chalasani N, Kahi C, Francois F, Pinto A, Marathe A, et al. (2003) Improved patient survival after acute variceal bleeding: a multicenter, cohort study. Am J Gastroenterol 98: 653-659.
- Thomopoulos K, Theocharis G, Mimidis K, Lampropoulou-Karatza Ch, Alexandridis E, et al. (2006) Improved survival of patients presenting with acute variceal bleeding. Prognostic indicators of short- and long-term mortality. Dig Liver Dis 38: 899-904.
- Crooks C, Card T, West J (2011) Reductions in 28-day mortality following hospital admission for upper gastrointestinal hemorrhage. Gastroenterology 141: 62-70.
- Lim LG, Ho KY, Chan YH, Teoh PL, Khor CJ, et al. (2011) Urgent endoscopy is associated with lower mortality in high-risk but not low-risk nonvariceal upper gastrointestinal bleeding. Endoscopy 43: 300-306.
- Hsu YC, Chung CS, Tseng CH, Lin TL, Liou JM, et al. (2009) Delayed endoscopy as a risk factor for in-hospital mortality in cirrhotic patients with acute variceal hemorrhage. J Gastroenterol Hepatol 24: 1294-1299.
- Stanley AJ, Ashley D, Dalton HR, Mowat C, Gaya DR, et al. (2009) Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: multicentre validation and prospective evaluation. The Lancet 373: 42-47.
- Rockall TA, Logan RF, Devlin HB, Northfield TC (1996) Risk assessment after acute upper gastrointestinal haemorrhage. Gut 38: 316-321.
- Vreeburg EM, Terwee CB, Snel P, Rauws EA, Bartelsman JF, et al. (1999) Validation of the Rockall risk scoring system in upper gastrointestinal bleeding. Gut 44: 331-335.
- Farooq FT, Lee MH, Das A, Dixit R, Wong RC (2012) Clinical triage decision vs risk scores in predicting the need for endotherapy in upper gastrointestinal bleeding. Am J Emerg Med 30: 129-134.
- Müller T, Barkun AN, Martel M (2009) Non-variceal upper GI bleeding in patients already hospitalized for another condition. Am J Gastroenterol 104: 330-339.
- Lanas A, Aabakken L, Fonseca J, Mungan ZA, Papatheodoridis GV, et al. (2011) Clinical predictors of poor outcomes among patients with nonvariceal upper gastrointestinal bleeding in Europe. Aliment Pharmacol Ther 33: 1225-1233.
- Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, et al. (2013) Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med 368: 11-21.
- Abraldes JG, Villanueva C, Bañares R, Aracil C, Catalina MV, et al. (2008) Hepatic venous pressure gradient and prognosis in patients with acute variceal bleeding treated with pharmacologic and endoscopic therapy. J Hepatol 48: 229-236.
- Ioannou G, Doust J, Rockey DC (2003) Terlipressin for acute esophageal variceal hemorrhage. Cochrane Database Syst Rev 1: CD002147.
- Bernard B, Grangé JD, Khac EN, Amiot X, Opolon P, et al. (1999) Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology 29: 1655-1661.
- Chavez-Tapia NC, Barrientos-Gutierrez T, Tellez-Avila FI, Soares-Weiser K, Uribe M (2010) Antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding. Cochrane Database Syst Rev : CD002907.
- Augustin S, Altamirano J, González A, Dot J, Abu-Suboh M, et al. (2011) Effectiveness of combined pharmacologic and ligation therapy in high-risk patients with acute esophageal variceal bleeding. Am J Gastroenterol 106: 1787-1795.
- Hsu YC, Perng CL, Yang TH, Wang CS, Hsu WL, et al. (2010) A randomized controlled trial comparing two different dosages of infusional pantoprazole in peptic ulcer bleeding. Br J Clin Pharmacol 69: 245-251.
- Sreedharan A, Martin J, Leontiadis GI, Dorward S, Howden CW, et al. (2010) Proton pump inhibitor treatment initiated prior to endoscopic diagnosis in upper gastrointestinal bleeding. Cochrane Database Syst Rev 7: CD005415.
- Bai Y, Guo JF, Li ZS (2011) Meta-analysis: erythromycin before endoscopy for acute upper gastrointestinal bleeding. Aliment Pharmacol Ther 34: 166-171.
- Guglielmi A, Ruzzenente A, Sandri M, Kind R, Lombardo F, et al. (2002) Risk assessment and prediction of rebleeding in bleeding gastroduodenal ulcer. Endoscopy 34: 778-786.
- Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, et al. (2013) Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med 368: 11-21.
- Vergara M, Calvet X, Gisbert JP (2007) Epinephrine injection versus epinephrine injection and a second endoscopic method in high risk bleeding ulcers. Cochrane Database Syst Rev : CD005584.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15362
- [From(publication date):
specialissue-2013 - Dec 19, 2025] - Breakdown by view type
- HTML page views : 10638
- PDF downloads : 4724