Case Report Open Access
A Rare Case of Pancreatitis, Panniculitis and Polyarthritis: The P-P-P Syndrome
Dario Fabbri, Davide Campana, Donatella Santini, Riccardo Casadei, Roberto De Giorgio and Paola Tomassetti*
Department of Medical and Surgical Sciences, St. Orsola-Malpighi Hospital, University of Bologna, Italy
- *Corresponding Author:
- Paola Tomassetti
Department of Medical and Surgical Sciences – University of Bologna
S.Orsola-Malpighi University Hospital - Via Massarenti
9 - 40138, Bologna, Italy
Tel: 390516363558
E-mail: paola.tomassetti@unibo.it
Received date: November 02, 2015 Accepted date: November 16, 2015 Published date: November 30, 2015
Citation: Fabbri D, Campana D, Santini D, Casadei R, Giorgio RD, et al. (2015) A Rare Case of Pancreatitis, Panniculitis and Polyarthritis: The P-P-P Syndrome. J Gastrointest Dig Syst 5:356. doi:10.4172/2161-069X.1000356
Copyright: © 2015 Fabbri D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
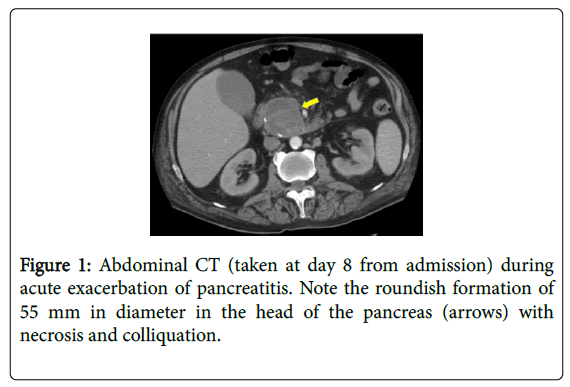
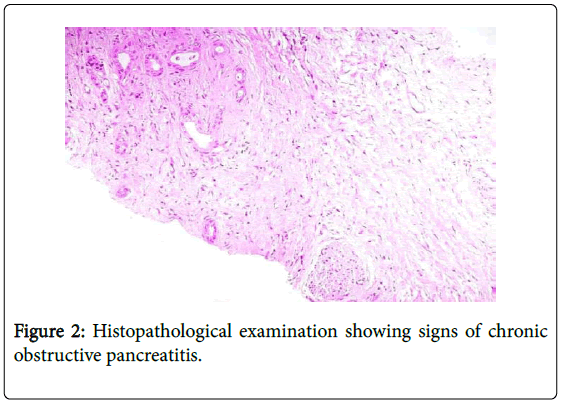
A 70-year-old man was admitted to our Unit because of the onset of symmetric joint pain, and multiple cutaneous erythematous nodules localized to the lower extremities and gluteal region. An arthrocentesis excluded a septic arthritis and systemic and local steroid therapy resulted in a modest improvement of symptoms and cutaneous manifestations. For an acute abdominal pain with an elevation of serum amylase and lipase levels, the patient underwent an abdominal CT that showed a 55 mm roundish mass in the head of the pancreas with necrosis and colliquation, associated with dilatation of the main pancratic duct and thrombosis of the superior mesenteric vein. The pancreatic lesion was biopsied during an endoscopic ultrasonography and the histopathological examination documented a chronic obstructive pancreatitis. Taken together, the clinical manifestations shown by this case highlighted a rare condition referred to as “PPP (i.e. pancratitis, panniculitis, polyarthritis) syndrome” which links pancreatitis to extrapancreatic tissue involvement.
Keywords
PPP Syndrome; Pancreatitis; Panniculitis; Polyarthritis; Erythematous nodules; Pancreatic disease
Introduction
Chronic pancreatitis is an inflammatory process progressively evolving to gland insult with major remodeling of the pancreatic parenchyma. This tissue damage in chronic pancreatitis leads to exocrine and endocrine dysfunction. Several risk factors have been identified, altrough in a non-neglegible percentage of patients the disease remains idiopathic in origin. The primary clinical manifestations of chronic pancreatitis are abdominal pain and recurrent episodes of pancreatitis, while pancreatic insufficiency appears in the late stage of the disease. Rarer complications, such as extrapancratic tissue involvement including panniculitis and arthritis, may also occur. The concomitant association of chronic ancreatitis, skin involvement and joint inflammation is referred to as "pancratitis, panniculitis, polyarthritis" (PPP) syndrome [1-6]. In this very rare cases, the diagnosis of pancreatitis can be dealyed because of the presence of mild abdominal pain and the predominance of cutaneus and articular manifestations [1,7-11]. We herein describe the case of a man with this rare syndrome to show the importance of an early diagnosis which is crucial for the prognosis of this generally fatal clinical association.
Case Report
A 70-year-old man was admitted to our Internal Medicine Unit in April 2013 for the onset of symmetric joint pain. He was smoker and a habitual alcohol drinker (more than 1 L / day since many years). On admission, clinical examination revealed multiple cutaneous erythematous nodules (1-5 cm in size) localized to the lower extremities and gluteal region, with some of them evolving into necrotic abscesses, spontaneously ulcerating and exuding 'fatty material'. Physical examination of the abdomen and the cardiorespiratory systems was unrelevant and vital signs were normal. Laboratory tests showed a remarkable leukocytosis (WBC: 18,000 / mmc, neutrophilis 91%) and a prominent increase of inflammatory indexes (C-reactive Protein: 17.3 g/dL, n.v. <0.80). An autoimmunity profile (ANA, ENA, anti-DNA, rheumatoid factor, anti-CCP, ANCA, C3 and C4, streptozyme test) and oncomarkers were all negative. Also, the patient complained of severe pain involving bilateral ankles, knees, shoulders and elbows joints associated with evident swelling. X-Ray evaluation dis not show any articular / bone changes, while the arthrocentesis demonstrated a yellowish synovial fluid which was negative for bacteria or other infections and therefore excluding a septic arthritis. Systemic (methylprednisolone, 60 mg daily) and local (intrarticular) steroid therapy resulted in a modest improvement of pain.
Moreover, a few days later, the patient experienced an acute abdominal pain with a prominent localization to the mesogastrium. Serum amylase and lipase levels were ten (i.e.: 1037 U/L, n.v. <100) and sixty (3621 U/L, n.v. <60) times over the respective normal values, thus indicating an acute pancreatitis.
An abdominal CT (Figure 1) showed a roundish mass of 55 mm in diameter in the head of the pancreas with necrosis and colliquation. This finding was associated with dilatation of the main pancratic duct and thrombosis of the superior mesenteric vein. The pancreatic lesion was biopsied during an endoscopic ultrasonography (EUS) and the histopathological examination documented a chronic obstructive pancreatitis (Figure 2). Based on the clinical and biochemical alterations we concluded that an acute pancreatitis developed on a chronic disease and that was complicated by a bulky pseudocyst. Meanwhile, the histopathological analysis of the erythematous nodules showed necrotic areas containing “ghost-like” fat cells, a typical feature of pancreatic enzyme-related panniculitis. Due to these findings and the worsening of the clinical picture, steroids were stopped. The risk of a neoplastic component in the pancreatic lesion prompted a rapid referral to surgery. The patient underwent a laparotomic examination disclosing a chronic pancreatitis and a massive post-necrotic pseudocyst connected to the main pancreatic duct. An intraoperative US and histopathology confirmed the existence of a chronic obstructive pancreatitis. The procedure consisted of thorough drainage of pseudocyst content (mainly necrotic tissue) followed by a manual latero-lateral Wirsung-pseudocyst-jejunal anastomosis. In the postoperative phase the patient developed a severe septicemia and, although under an intensive care unit regimen, he died five days after the operation.
Discussion
So far, only 30 cases of PPP syndrome have been reported in the literature. The pathogenesis of this syndrome is still uncelar, although it is widley accepted that pancreatic enzymes, released into systemic circulation, may lead to lipolysis and secondary inflammation in peripheral tissues, like subcutaneus tissues and joints [7,12-14].
Although mainly acute [1], chronic chronic pancreatitis can occur [14-17] in this syndrome as highlighted by this case, while the association with pancreatic adenocarcinoma is quite rare [2]. Panniculitis is usually characterized by erythematous nodules, more frequently localized at the lower limb that can evolve into necrotizing abscess [3-5,18]. The clinical manifestation of pancreatic panniculitis is, however, nonspecific and therefore histopathology of skin lesions is mandatory to unravel, as in this case, pathognomonic hallmarks such as anucleated adipocytes with a thickened shadowy wall and granular basophilic cytoplasm (hence “ghost-like cell” adipocytes) [14,18,19].
Joints can be involved at any level in the PPP syndrome although the number can be quite variable: likewise in our experience, most of the reported cases indicated a symmetric or asymmetric polyarthritis [1], although oligoarthritis and monoarthritis have been also described [16].
The treatment of PPP syndrome is aimed to resolve the pancreatic disease and that is why we referred our patient to surgery. Nonetheless, supportive measures are also important and include fluid / electrolyte replacement, adequate pain control and, if necessary, nutritional support. Steroids and non-steroid anti-inflammatory drugs can only alleviate symptoms related to skin lesions and arthritis [1].
A posteriori, we can conclude that a more rapid diagnosis would have resulted in a better outcome of this patient. Nonetheless, a careful analysis of this case raises some considerations. First, the paucisymptomatic onset of the PPP syndrome was clinically misleading as the patient, despite his clinical history indicated a habit to alcohol consumption, did not complain any symptom suggestive of a pancreatic disorder; secondly, we were unable to establish a clear link between the detected skin lesions to an underlying pancreatitis which was possible after an acute exacerbation of an obstructive pancreatitis, secondary to the large-size pseudocyst obstructing the Wirsung duct; thirdly, the quite rapid progression of the disease which prevented an appropriate timing for referring the patient to surgery. In conclusion, the present case confirmed that, although rare, the PPP syndrome could occur in acute and chronic pancreatitis setting. The latter may have acute re-exacerbation responsible for extrapancreatic (systemic) associations. The clinician should be always aware of the PPP syndrome as it early recognition is crucial for an appropiate management, referral to surgery (if needed) and better outcome.
Acknowledgements
All authors approved the final version of the article, including the authorship list. The authors declare that they have no conflict of interest.
References
- Narváez J, Bianchi MM, Santo P, de la Fuente D, Ríos-Rodriguez V, et al. (2010) Pancreatitis, panniculitis, and polyarthritis. Semin Arthritis Rheum 39: 417-423.
- Borowicz J, Morrison M, Hogan D, Miller R (2010) Subcutaneous fat necrosis/panniculitis and polyarthritis associated with acinar cell carcinoma of the pancreas: a rare presentation of pancreatitis, panniculitis and polyarthritis syndrome. J Drugs Dermatol 9: 1145-1150.
- Fraisse T, Boutet O, Tron AM, Prieur E (2010) Pancreatitis, panniculitis, polyarthritis syndrome: an unusual cause of destructive polyarthritis. Joint Bone Spine 77: 617-618.
- Harris MD, Bucobo JC, Buscaglia JM (2010) Pancreatitis, panniculitis, polyarthritis syndrome successfully treated with EUS-guided cyst-gastrostomy. Gastrointest Endosc 72: 456-458.
- Jose T, Biju IK, Kumar A (2008)'Pancreatitis, polyarthritis, panniculitis syndrome' (PPP syndrome) plus prolonged pyrexia--a rare presentation of chronic pancreatitis. Indian J Gastroenterol 28: 186-188.
- Mustafa KN, Hadidy A, Shoumaf M, Razzuki SA (2010) Polyarthritis with chondronecrosis associated with osteonecrosis, panniculitis and pancreatitis. Rheumatol Int 30: 1239-1242.
- Fine RM (1983) The fine page. Subcutaneous fat necrosis, pancreatitis, and arthropathy. Int J Dermatol 22: 575-576.
- Phillips RM Jr, Sulser RE, Songcharoen S (1980) Inflammatory arthritis and subcutaneous fat necrosis associated with acute and chronic pancreatitis. Arthritis Rheum 23: 355-360.
- Wilson HA, Askari AD, Neiderhiser DH, Johnson AM, Andrews BS, et al. (1983) Pancreatitis with arthropathy and subcutaneous fat necrosis. Evidence for the pathogenicity of lipolytic enzymes. Arthritis Rheum 26: 121-126.
- López A, García-Estañ J, Marras C, Castaño M, Rojas MJ, et al. (1998) Pancreatitis associated with pleural-mediastinal pseudocyst, panniculitis and polyarthritis. Clin Rheumatol 17: 335-339.
- Mourad FH, Hannoush HM, Bahlawan M, Uthman I, Uthman S (2001) Panniculitis and arthritis as the presenting manifestation of chronic pancreatitis. J Clin Gastroenterol 32: 259-261.
- Haller J, Greenway G, Resnick D, Kindynis P, Kang HS (1989) Intraosseous fat necrosis associated with acute pancreatitis: MR imaging. Radiology 173: 193-195.
- Watts RA, Kelly S, Hacking JC, Lomas D, Hazleman BL (1993) Fat necrosis. An unusual cause of polyarthritis. J Rheumatol 20: 1432-1435.
- Shbeeb MI, Duffy J, Bjornsson J, Ashby AM, Matteson EL (1996) Subcutaneous fat necrosis and polyarthritis associated with pancreatic disease. Arthritis Rheum 39: 1922-1925.
- Simkin PA, Brunzell JD, Wisner D, Fiechtner JJ, Carlin JS, et al. (1983) Free fatty acids in the pancreatitic arthritis syndrome. Arthritis Rheum 26: 127-132.
- Kotilainen P, Saario R, Mattila K, Nylamo E, Aho H (1998) Intraosseous fat necrosis simulating septic arthritis and osteomyelitis in a patient with chronic pancreatitis. Arch Orthop Trauma Surg 118: 174-175.
- Menon P, Kulshreshta R (2004) Pancreatitis with panniculitis and arthritis: a rare association. Pediatr Surg Int 20: 161-162.
- Dahl PR, Su WP, Cullimore KC, Dicken CH (1995) Pancreatic panniculitis. J Am Acad Dermatol 33: 413-417.
- Dhawan SS, Jimenez-Acosta F, Poppiti RJ Jr, Barkin JS (1990) Subcutaneous fat necrosis associated with pancreatitis: histochemical and electron microscopic findings. Am J Gastroenterol 85: 1025-1028.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13424
- [From(publication date):
December-2015 - Aug 19, 2025] - Breakdown by view type
- HTML page views : 12393
- PDF downloads : 1031