A Rare Case of Vertebral Osteomyelitis as a Complication of Colon Cancer
Received: 14-Jul-2018 / Accepted Date: 03-Aug-2018 / Published Date: 10-Aug-2018 DOI: 10.4172/2161-069X.1000574
Keywords: Colon cancer; Osteomyelitis; E. coli; Bacteremia
Case Description
A 66-year-old female with a Past medical history of Type II Diabetes mellitus, pancreatitis, and hypertension was admitted with complains of fever and shaking chills for 2 days prior to her admission, along with complains of lower back pain which she attributed to a fall few days prior to admission. She was found to have a lactic acid level of 4.8 on admission. A chest X-ray obtained during admission was consistent with left lower lobe pneumonia, and patient was started on IV antibiotics for community acquired pneumonia. After adequate fluid resuscitation, her lactic acidosis resolved. A day after admission, patient developed leukocytosis with a white count of 12.8, and bands of 65, and pro-calcitonin level was 29.02. Urine analysis and Urine culture obtained were negative, however, blood cultures from admission grew E. coli . Patient was started on IV antibiotics.
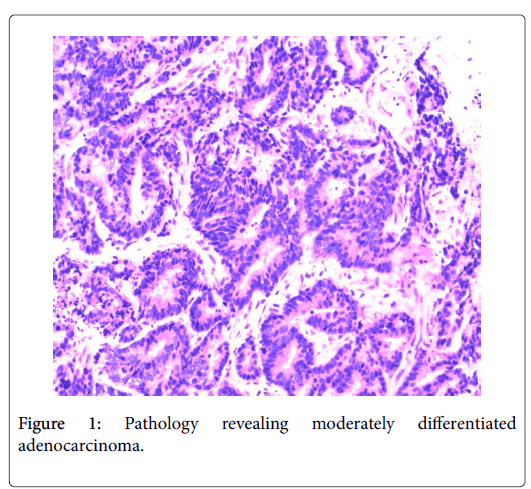
A CT chest/abdomen/pelvis was consistent with left lower lobe pneumonia, and no other gross abnormality was identified. During her stay in the hospital, patient continued to complain of pain in her lower back. Unable to tolerate an MRI at this time, patient was sent for a CT lumbar spine that showed some mild degenerative changes (and central stenosis at L3-L4 and L4-L5 levels). Two days after finishing her antibiotic course, patient was noted to be febrile. Repeat blood cultures were again found to be positive for E. coli , and antibiotics were resumed. A repeat CT chest/abd/pelvis with contrast showed new findings of a probable infectious spondylitis and diskitis. MRI findings confirmed findings of discitis, osteomyelitis and bilateral paraspinal abscesses. Since no obvious source for the bacteria was identified, patient was scheduled for a NM gallium scan which showed an abnormal persistent uptake in the region of the lower lumbar spine and the paraspinal region suggestive of inflammation, along with an apparent colitis. The patient underwent a colonoscopy, during which a cecal mass was identified with no evidence of colitis. Pathology report obtained from the cecal mass biopsy was consistent with moderately differentiated adenocarcinoma (Figure 1 and Table 1).
| Gender | Age | PMHx | Initial Blood Cultures | Repeat Blood Cultures | Pathology |
|---|---|---|---|---|---|
| Female | 66 | Diabetes, HTN, Pancreatitis | E. coli | Persistent E. coli |
Moderately differentiated adenocarcinoma |
Table 1: Basic characteristics and demographic of patient.
Patient eventually underwent a laparoscopic right colectomy. The tumor, which was 3.7 cm, was found to extend deeply into the muscularis propria, and was consistent with moderately differentiated adenocarcinoma. The tumor stage was found to be pT3, N0. Colon cancer is one of the leading causes of death in the United States and ranks as the third most commonly diagnosed cancer in males after prostate and lung, and the second in females after breast cancer, with the rates being substantially higher in males than females. Historically it was linked that certain blood stream infection raise the suspicion of colon cancer, given the possibility that a breach in the colonic mucosa could generate a portal of entry for the colonic flora into the blood stream. Even though the colonic mucosa provides an inhabitant of hundreds of different species of organisms, this case study attempts to provide an association between recurrent E. coli bacteremia and colon cancer. Hence it could serve as an early signal to pursue further investigations for colon cancer.
Discussion
Colorectal Cancer (CRC) has been cited as the second leading cause of death of all the cancers affecting both males and female. Colon cancer is one of the leading causes of death in the United States. It ranks as the third most commonly diagnosed cancer in males after prostate and lung, and the second in females after breast cancer, with the rates being substantially higher in males than females [1]. Early diagnosis of the cancer in its early stage, and treatment is thus crucial in decreasing mortality. It is essential that physician’s be vigilant and be able to suspect and screen patient in order to establish an early diagnosis and possible cure. Our patient on admission presented with symptoms that were vague and was found to have E. coli bacteremia upon initial work-up. There have been many studies which have reported incidence’s of bacteremia presenting as an initial sign of colon cancer.
In fact, the association between Streptococcus bovis bacteremia and colon cancer has been well established. Some cases have also reported the association between bacteremia caused by other species including Streptococcus viridans [1], Clostridrium septicum [1], Streptococcus sanguis [2,3]. However, reports of bacteremia caused of E. coli and colo-rectal cancer are rare. Furthermore, our patient went on to develop osteomyelitis of her spine as a result of seeding from the bacteremia. Such complications due to bacteremia in colon cancer patients are rare. Robbins et al. reported a case of a patient who presented with vertebral osteomyelitis caused by Streptococcus bovis [4]. Even though a few cases reported association of vertebral osteomyelitis caused by Streptococcus bovis bacteremia [1], no similar cases of vertebral osteomyelitis due to E. coli bacteremia secondary to colon cancer were ever reported. Recognition of recurrent bacteremia with bacteria which colonizes the intestine [5], should raise suspicion of breach through the intestinal wall and the possibility of colonic neoplasms should be promptly investigated.
References
- Lin CY, Chao PC, Hong GJ, Tsai YT, Lee CY, et al. (2008) Infective endocarditis from Streptococcus viridans associated with colonic carcinoma: A case report. J Card Surg 23: 263-265.
- Mulita A, Ajayi T (2014) Streptococcus viridians bacteraemia and colonic adenocarcinoma. BMJ Case Rep.
- Fass R, Alim A, Kaunitz JD (1995) Adenocarcinoma of the colon presenting as Streptococcus sanguis bacteremia. Am J Gastroenterol 90: 1343-1345.
- Robbins N, Wisoff HS, Klein RS (1986) Vertebral osteomyelitis caused by Streptococcus bovis. Am J Med Sci 291: 128-129.
- Spadafora PF, Qadir MT, Cunha BA (1996) Streptococcus bovis endocarditis and vertebral osteomyelitis. Heart Lung 25: 165-168.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4306
- [From(publication date): 0-2018 - Dec 23, 2025]
- Breakdown by view type
- HTML page views: 3405
- PDF downloads: 901