A Review of Clinical Approach to a Patient with Tremor Disorder
Received: 02-Oct-2017 / Accepted Date: 09-Oct-2017 / Published Date: 16-Oct-2017 DOI: 10.4172/2161-0460.1000386
Abstract
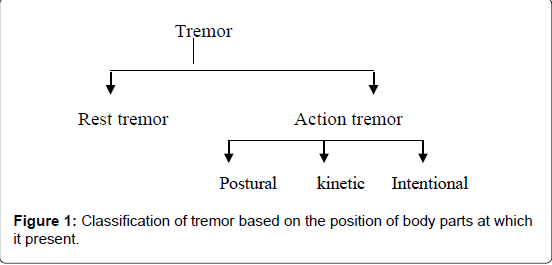
Tremor disorder is the most common movement disorder encountered in neurology and general practitioner’s clinic. The misdiagnosis of a tremor syndrome is prevalent, leading to erroneous reporting and treatment of this condition. This is our endeavor to give a simplified approach to outline Tremor disorders by reviewing the published literature on it. We searched Electronic databases MEDLINE/PubMed, Google Scholar, Cochrane library and ScopeMed with Mesh (Medical Subject Headings) terms “Tremor”, “Clinical features”, “Pathophysiology” and “treatment” from earliest possible date. Articles in any language especially those published in recent years were given preference. Tremor is classified into rest tremor and action tremor based on its presence on a different position of body parts. Action tremor is further categorized into postural, kinetic and intentional tremor. Resting tremor is classically seen in Parkinson’s disease. Essential tremor is the most common cause of postural tremor. Electromyography and accelerometer though helpful are complex tools to diagnose the tremor disorder. Tremor disorders should be approached systematically. We should proceed from the classification of tremor based on its presence in a different position of body parts. We need to corroborate clinical history, examination findings, and appropriate investigation report to reach the final etiological diagnosis of the tremor disorder.
Keywords: Tremor; Clinical features; Approach; Rest tremor; Action tremor
Introduction
Tremor is a rhythmical, involuntary oscillatory movement of a body part produced mostly by alternating contractions of reciprocally innervated muscles [1]. It is the most common type of movement disorder encountered in the movement disorder clinic [2]. The tremor syndrome may vary from an enhanced normal physiological response to the presenting manifestation of an underlying severe neurological disorder, like Parkinson’s disease, stroke and others - the list of which is exhaustive.
Tremor disorder may result in diverse and disparate effects on patients. It impacts on several domains of quality of life, from physical to psychosocial, in a large proportion of patients [3]. Thus, we should have sound knowledge on tremor syndrome and lower threshold to offer treatment to decrease an under-recognized impact of tremor on the quality of life [4].
The misdiagnosis of tremor syndromes is common and often underestimated problem which can cause misleading results in clinical trials trials [5]. At the level of clinical practice, misdiagnosis may lead to suboptimal treatment, poor response to treatment and dissatisfaction to the patient. The contributing factors of this problem are limited literature, confusing approach and inadequate diagnostic tools to distinguish different tremor syndromes and find out its etiologies [6]. This review is our endeavor to outline the simplified approach to tremor disorders.
Methods
We extensively searched Electronic databases MEDLINE/Pub Med, Google Scholar, IMSEAR(Index Medicus for South-East Asia Region) and ScopeMed searched with Mesh (Medical Subject Headings) terms “tremor”, “clinical features”, “path physiology” and “treatment” from earliest possible date. Articles in any language especially those published in recent years were given preference.
Epidemiology
Essential tremor (ET) is the most prevalent movement disorders, which present as an abnormal tremor in humans [7]. The incidence of ET rises with age [8,9]. The prevalence of essential tremor was 14% whereas Parkinson’s disease was 3% among elderly population of the community [10]. Wenning et al. in a Bruneck study cohort reported the prevalence of tremor among the population of 50-89 years age group was 14.5% [11]. Literature regarding the prevalence of other types of tremor syndromes is limited.
Classification
Tremor is a manifestation of the various diseases. We should have sound knowledge on clinical features and examination findings to diagnose the exact etiology of the tremor. A simplified approach to Tremor disorders is shown in Figure 1, where Tremor is classified on the basis of the position of the body parts at which it is present [1,12].
Phenomenological classification of tremor syndrome
Resting tremor: Resting tremor is evident when our body parts are relaxed and completely supported against gravity (e.g. with the hands in the lap). It is present during sitting, lying down, and relaxed position. It attenuates when the body part is in the movement while doing activities. Classically it is seen in the Parkinson’s disease; however, it may be a manifestation of a severe essential tremor, Wilson’s disease and rubral tremor.
Postural tremor: Postural tremor is conspicuous when limbs are voluntary maintained in an anti-gravity position (e.g. arms outstretched). It decreases when the body parts are supported. The various conditions associated with Postural tremor are listed in Table 1.
| Enhanced Physiologic Tremor |
| Essential Tremor |
| Endocrine:Hypoglycemia, thyrotoxicosis, pheochromocytoma |
| Anxiety, Stress |
| Toxins: Alcohol withdrawal, mercury lead, arsenic |
| Dystonia |
Table 1: Causes of postural tremor.
Kinetic tremor: Kinetic tremor appears while making a voluntary movement. It is appreciated during activities like eating, writing etc. This tremor is of special concern as it can hamper the daily activities of the patient. Essential tremor, Cerebellar tremor, dystonic tremor and primary writing tremor are the common conditions where kinetic tremor is seen. Kinetic tremor is further classified into a simple, intentional and task-specific tremor.
Intention tremor: Intentional tremor commonly known as cerebellar tremor is coarse tremor with a frequency of below 5 Hz, appears when precision is required to touch a target [1]. It progressively worsens during the movement and reaches its maximal intensity near the target. The limb shakes side-to-side perpendicular to the line of travel. Classically it is seen in Cerebellar disease of any etiology, where it is associated with other cerebellar symptoms. However, one-third of essential tremor had also intentional tremor [13].
Etiological classification of tremor syndrome
Essential tremor: Essential tremor is a bilateral, largely symmetric postural or kinetic tremor involving hands and forearms that are visible and persistent, and in which there is no other explanation for the tremor. (1) About half of essential tremor patients had a positive family history [14]. It may involve the voice, head and rarely the legs. The usual frequency of Essential tremor usually is 5-10 Hz and it has no latency to onset. Symptom severity often increases over time, but the progression is very slow [15]. The majority of patients do not show accompanying neurologic signs or symptoms, but occasionally instability or more distinct cerebellar signs may be found during the examination, especially in long-standing tremor [16]. This tremor aggravated with stress and attenuated with intake of alcohol.
Parkinson’s disease tremor: In Parkinson’s disease, Hughes et al. reported that seventy-five percent patient had rest tremor during the course of the disease [17]. Parkinsonian rest tremor is characterized by distal predominant, asymmetrical in onset, gradually progressive, supination-pronation, pill rolling type of tremor [18]. It attenuates during activities and sleep. It is associated with the tremor of lips, jaw and lower limbs. Resting tremor of Parkinson’s disease is usually combined with postural and kinetic tremor [1].
Drug-induced tremor: Drug-induced tremor is usually symmetrical. It follows the temporal pattern with the initiation of drugs and decreases with the cessation of culprit drug. It is the diagnosis of exclusion and other causes of tremor should be ruled out [19]. Risk factors for drug-induced tremor are advancing age, Poly-pharmacy, underlying structural brain disease, anxious state and renal failure.
The etiology of tremor in a certain subset of cases could be attributed to medications the individuals have been administered for certain underlying medical disorders as well. Hereby, in Table 2, we present a list of a number of drugs notorious for causing tremors [12,20,21].
| Class of medication | Examples |
|---|---|
| Beta-adrenergic agonists | Terbutaline, adrenaline, salbutamol |
| Antidepressants | Bupropion, lithium, tricyclic antidepressants, |
| Neuroleptics | Haloperidol |
| Anticonvulsants | Sodium valproate, carbamazepine |
| Dopamine agonists | Amphetamine |
| Heavy metals | Mercury, lead, arsenic, bismuth |
| Xanthines or derivatives | Coffee, tea, theophylline, cyclosporine |
| Anti-arrhythmics | Amiodarone, verapamil |
| Endocrinologic agents | Throxine, Corticosteroids |
| Dopamine antagonist | Metoclopramide |
Table 2: Drugs causing tremor.
Neuropathic tremor: Neuropathic tremor is also known as Essential Tremor-like. It is characterized by the postural or kinetic distal predominant symmetrical tremor of [22]. It is manifested in inherited or acquired large fiber predominant peripheral neuropathies. Its frequency ranges from 2.8 Hz to 5.5 Hz [23]. Chronic inflammatory demyelinating polyneuropathy may be associated with this tremor, where it is associated with the IgG4 NF155 antibody [24]. The development of these tremors occurs sub-acutely within weeks to months. On neurologic examination, other signs of peripheral neuropathy may be present. Serum electrophoresis, electrophysiological studies, cerebrospinal fluid analysis and sometimes nerve biopsy, can help us come to a diagnosis [25].
Dystonic tremor
Tremor is part and parcel of primary dystonia [26]. Dystonic tremor is a focal, postural or kinetic tremor in an individual with dystonia. This tremor may occur in the exact same part of the body as the dystonia or in a different area altogether [27]. Both the frequency and amplitude are often irregular and variable. Subtle symptoms, in terms of mild blepharospasm, voice change of spasmodic dysphonia, or slight torticollis, may be seen as important clues by the clinician. Responsiveness to sensory tricks (gestures antagonistic ques) and exhibition of null point (position of the body with no tremor) indicates a dystonic tremor [28]. Task-specific tremor, such as tremor that only occurs when writing (primary writing tremor) or when performing other specific tasks, may be a form of dystonic tremor [29]. Botulinum toxin injections can ameliorate dystonia and dystonic tremor and are accepted as the treatment of choice [30].
Psychogenic tremor
Psychogenic tremor is characterized by its sudden onset and its association with a stressful life event. It may manifest as a combination of resting, postural, or intention tremors. It begins with the involvement of arms which is followed by involvement of the head and the legs. It shows a continuous or intermittent pattern with fluctuating frequency and amplitude. The majority of the patients have a maximal disability (46%) at its onset [31]. Although various criteria are proposed, the diagnosis can be obvious in patients with abrupt onset generalized shaking [32,33]. Entrainment sign and the co-activation sign are hallmarks to diagnose the psychogenic tremor [34]. Entrainment sign requires the patient to maintain a tapping rhythm in an uninvolved body part at a different frequency than the suspicious tremor which automatically changes the frequency of involved part to the tapping enforced frequency. Co-activation sign is the presence the increased tone of the involved limb during its passive movement and decrease of the tremor with the decrease in muscle tone. This tremor has unpredictable course and usually attenuate with sedatives.
Orthostatic tremor
Orthostatic tremor is characterized by high frequency (13-18 Hz) tremor occurring in the legs of a person when erect and causes postural instability. Women are affected slightly more frequently, than men [35]. The mean age of onset of orthostatic tremor is the sixth decade. Most cases are sporadic. The syndrome can be primary or secondary and may be associated with a variety of disorders, most commonly Parkinsonism. Postural and kinetic tremor is most common, characterized by unsteadiness on standing. The symptoms improve markedly on sitting or walking. At times, the urge to sit down or to move can be so strong that patients often avoid situations where they have to stand still for a period of time, such as when queuing.
The high tremor frequency leads to a partial fusion of the single muscle contractions, and it can be easier to listen to the contractions through a stethoscope applied to thigh or calf muscles. The sound has been compared with that of a helicopter [36]. Treatment options include clonazepam, primidone [37], gabapentin and benzodiazepines.
Clinical examination
We should perform a thorough clinical examination of the patients with tremor disorder to find the subtle associated neurological findings. Resting tremor should be observed when the patient’s affected body parts aren’t voluntarily activated and when they are supported against gravity. The most appropriate time is when the patient is concentrating on other tasks, e.g. walking or during a conversation. The postural tremor is examined asking the patient to hold the upper extremities in an outstretched position. The amplitude of postural tremor can be appreciated by putting a piece of paper on the outstretched hands [1]. Intention tremor, which is evident on “Goal-Directed Movements” which increased in amplitude when the subject approaches a goal. It can be elicited in goal-directed activities, such as finger-to-nose, heel to shin, and toe-to-finger movements.
Observing a patient while drawing (e.g. Archimedes spirals) or writing is often helpful: Action tremor is increased during writing or drawing, and a task-specific tremor may become obvious. In Parkinson’s disease, there is usually no tremor during writing, but other signs can be seen, such as increasing micrographia and slow movements. Archimedes spiral drawing is helpful to differentiate the essential tremor from Parkinson’s disease tremor [37,38]. Pouring water from one cup into other shows the degree of disability due to kinetic tremor in a practical situation [21].
The important clues about an underlying neurologic disorder in patients presenting with a tremor can be found during the examination of the cranial nerves, speech, gait, balance, and muscle tone. On ocular examination, the presence of nystagmus may suggest cerebellar disease and Kayser-Fleischer rings are specific for impaired copper homeostasis. Several movement disorders affect the fine-tuned movements of the tongue, where possible abnormal findings include fasciculation or slowness of tongue movements can be observed. Slow and irregular speech with increased separation of syllables or explosive sounds may indicate cerebellar dysarthria. Voice tremor can be appreciated in Essential tremor [39]. On Gait examination, typical Parkinsonian slow shuffling or wide-based ataxic cerebellar gait may be noted. Muscular rigidity in combination with a tremor at rest is typical for Parkinson’s disease, whereas spasticity may develop in Multiple sclerosis.
Electromyography
Electromyography (EMG) is a simple tool that can be useful for the diagnosis of tremor syndrome [40]. Electromyography provides additional useful information about the activity of muscles involved in the generation of tremor. EMG activity may be recorded using needle, wire electrodes, or more typically surface electrodes overlying active muscles [41]. The EMG can provide information about motor unit recruitment and synchronization [42,43]. It can also elucidate the relationship between involved muscles and tremulous movements, revealing whether antagonist muscles (such as flexors and extensors of the wrist) are working at the same time or alternately to produce tremor, which helps to differentiate dystonic tremor from other types of tremor. To utilize the EMG most appropriately in tremor analysis, the signal has to be processed by rectification and integration or smoothing to place its frequency profile into the tremor range [42].
The objective and detailed findings of a tremor analysis test are most helpful when the clinical picture is complicated or when clinical signs are subtle [44]. EMG analysis may be required to differentiate Parkinsonian tremor from essential tremor where than treatment of the two entity is distinct. EMG analyze side-to-side frequency relationship, EMG topography, reflex responses, tremor amplitude ratios during different clinical tasks.
Accelerometer
It is the most common and gold standard method used to electronically evaluate a tremor. A linear tri-axial accelerometer measures frequency and magnitude of the oscillatory cycles of the tremor. Its frequency represents the dominant frequency of the tremor. The findings of accelerometer help us to differentiate Parkinson’s disease tremor from essential tremor. The tremor frequency of below 5.5 Hz suggests Parkinson’s disease whereas the tremor frequency above 6 Hz suggest Essential tremor [45]. Though it is an objective measure of frequency and amplitude of tremor, it is expensive, complex and time-consuming. Most importantly, it does not measure the functional disability resulting from the tremor. Joundi et al. [45] reported that iPhone accelerometer is comparable to sophisticated EMG analysis and may be useful in day to day clinical practice.
Future direction
This review highlight the need of future research to determine utility of Archimedes spiral and the effectiveness of different mobile based application, which is more practical even for resource limited settings in diagnosis tremor syndrome.
Conclusion
Tremor disorders should be approached systematically. The tremor should be initially classified into rest or action tremor. Reversible and benign condition like enhanced physiological tremor should be ruled out first by taking detail history regarding the stress, caffeine use, drugs intake etc. Though the essential tremor is the most common movement disorder in general population, other organic cause of tremors like Parkinson’s disease, Wilson disease, or vascular disease should be excluded first before reaching to diagnosis of essential tremor. We should perform detail neurological examination to find out the subtle associated findings. Drawing Archimedes spiral is a cost-effective and can differentiate the different tremor syndrome. Accelerometer and Electromyography are complex, time-consuming and expensive thus relying on their report for tremor diagnosis seems impracticable in day to day clinical practice.
References
- Deuschl G, Bain P, Brin M (1998) Consensus statement of the movement disorder society on tremor. ad hoc scientific committee. Mov Disord 13: 2-23.
- Wenning GK, Kiechl S, Seppi K, Miller J, Hugl B, et al. (2005) Prevalence of movement disorders in men and women aged 50-89 years (Bruneck Study cohort): A population-based study. Lancet Neurol 4: 815-820.
- Louis ED, Cosentino S, Huey ED (2016) Depressive symptoms can amplify embarrassment in essential tremor. J Clin Mov Disord 3: 11.
- Louis ED, Machado DG (2015) Tremor-related quality of life: A comparison of essential tremor vs. Parkinson’s disease patients. Parkinsonism Relat Disord 21: 729-735.
- Rizzo G, Copetti M, Arcuti S, Martino D, Fontana A, et al. (2016) Accuracy of clinical diagnosis of Parkinson disease. Neurology 86: 566-576.
- di Biase L, Brittain JS, Shah SA, Pedrosa DJ, Cagnan H, et al. (2017) Tremor stability index: A new tool for differential diagnosis in tremor syndromes. Brain 140: 1977-1986.
- Louis ED, Ferreira JJ (2010) How common is the most common adult movement disorder? Update on the worldwide prevalence of essential tremor. Mov Disord 25: 534-541.
- Benito-Leon J, Bermejo-Pareja F, Louis ED (2005) Neurological disorders in central spain (NEDICES) study group. Incidence of essential tremor in three elderly populations of central Spain. Neurology 64: 1721-1725.
- Rajput AH, Offord KP, Beard CM, Kurland LT (1984) Essential tremor in Rochester, Minnesota: a 45-year study. J Neurol Neurosurg Psychiatry 47: 466-470.
- Moghal S, Rajput AH, D'Arcy C, Rajput R (1994) Prevalence of movement disorders in elderly community residents. Neuroepidemiology 13: 175-178.
- Leehey MA (2001) Tremor: Diagnosis and treatment. Prim Care Case Rev 4: 9.
- Louis ED, Frucht SJ, Rios E (2009) Intention tremor in essential tremor: Prevalence and association with disease duration. Mov Disord 24: 626-627.
- Whaley NR, Putzke JD, Baba Y, Wszolek ZK, Uitti RJ (2007) Essential tremor: Phenotypic expression in a clinical cohort. Parkinsonism Relat Disord 13: 333-339.
- Putzke JD, Whaley NR, Baba Y, Wszolek ZK, Uitti RJ (2006) Essential tremor: Predictors of disease progression in a clinical cohort. J Neurol Neurosurg Psychiatry 77: 1235-1237.
- Singer C, Sanchez-Ramos J, Weiner WJ (1994) Gait abnormality in essential tremor. Mov Disord 9: 193-196.
- Hughes AJ, Daniel SE, Blankson S, Lees AJ (1993) A clinicopathologic study of 100 cases of Parkinson's disease. Arch Neurol 50: 140-148.
- Jankovic J (2008) Parkinson's disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry 79: 368-376.
- Morgan JC, Sethi KD (2005) Drug-induced tremors. Lancet Neurol 4: 866-876.
- Bhidayasiri R (2005) Differential diagnosis of common tremor syndromes. Postgrad Med J 81: 756-762.
- Puschmann A, Wszolek ZK (2011) Diagnosis and treatment of common forms of tremor. Semin Neurol 31: 65-77.
- Morini A, Malaguti MC, Marangoni S, Espay AJ (2016) Neuropathic tremor in chronic inflammatory demyelinating polyneuropathy: The acquired equivalent of the Roussy-Levy syndrome. Mov Disord Clin Pract 3: 173-175.
- Bain PG, Britton TC, Jenkins IH, Thompson PD, Rothwell JC, et al. (1996) Tremor associated with benign IgM paraproteinaemic neuropathy. Brain 119: 789-799.
- Querol L, Nogales-Gadea G, Rojas-Garcia R, Diaz-Manera J, Pardo J, et al. (2014) Neurofascin IgG4 antibodies in CIDP associate with disabling tremor and poor response to IV Ig. Neurology 82: 879-886.
- Köller H, Kieseier BC, Jander S, Hartung HP (2005) Chronic inflammatory demyelinating polyneuropathy. N Engl J Med 352: 1343-1356.
- Evatt ML, Freeman A, Factor S (2011) Adult-onset dystonia. Handb Clin Neurol 100: 481-511.
- Quinn NP, Schneider SA, Schwingenschuh P, Bhatia KP (2011) Tremor--some controversial aspects. Mov Disord 26: 18-23.
- Bain PG, Findley LJ, Britton TC, Rothwell JC, Gresty MA, et al. (1995) Primary writing tremor. Brain 118: 1461-1472.
- Zesiewicz TA, Elble R, Louis ED, Hauser RA, Sullivan KL, et al. (2005) Practice parameter: Therapies for essential tremor: Report of the quality standards subcommittee of the American Academy of Neurology. Neurology 64: 2008-2020.
- Kim YJ, Pakiam AS, Lang AE (1999) Historical and clinical features of psychogenic tremor: A review of 70 cases. Can J Neurol Sci 26: 190-195.
- Deuschl G, Köster B, Lücking CH, Scheidt C (1998) Diagnostic and pathophysiological aspects of psychogenic tremors. Mov Disord 13: 294-302.
- Koller W, Lang A, Vetere-Overfield B, Findley L, Cleeves L, et al. (1989) Psychogenic tremors. Neurology 39: 1094-1099.
- Bhatia KP, Schneider SA (2007) Psychogenic tremor and related disorders. J Neurol 254: 569-574.
- Gerschlager W, Münchau A, Katzenschlager R, Brown P, Rothwell JC, et al. (2004) Natural history and syndromic associations of orthostatic tremor: A review of 41 patients. Mov Disord 19: 788-795.
- Brown P (1995) New clinical sign for orthostatic tremor. Lancet 346: 306-307.
- Britton TC, Thompson PD, Kamp W, Rothwell JC, Day BL, et al. (1992) Primary orthostatic tremor: Further observations in six cases. J Neurol 239: 209-217.
- Badalà F, Nouri-mahdavi K, Raoof (2008) The spiral axis as a clinical tool to distinguish essential tremor from dystonia cases. Park Relat Disord 144: 724-732.
- Louis ED, Ford B, Barnes LF (2000) Clinical subtypes of essential tremor. Arch Neurol 57: 1194-1198.
- Benaderette S, Fregonara PZ, Apartis E, Nguyen C, Trocello JM, et al. (2006) Psychogenic parkinsonism: A combination of clinical, electrophysiological and [123 I]-FP-CIT SPECT scan explorations improves diagnostic accuracy. Mov Disord 21: 310-317.
- Pullman SL, Goodin DS, Marquinez AI, Tabbal S, Rubin M (2000) Clinical utility of surface EMG: report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology. Neurology 55: 171-177.
- Elble RJ, Wc K (1990) Unusual forms of tremor. Tremor, The Johns Hopkins University Press, Baltimore 1990: 154-157.
- Elble RJ (1986) Physiologic and essential tremor. Neurology 36: 225-231.
- Louis ED, Ford B, Pullman S, Baron K (1998) How normal is 'normal'? Mild tremor in a multiethnic cohort of normal subjects. Arch Neurol 55: 222-227.
- Burne JA, Hayes MW, Fung VSC, Yiannikas C, Boljevac D (2002) The contribution of tremor studies to diagnosis of Parkinsonian and essential tremor: A statistical evaluation. J Clin Neurosci 9: 237-242.
- Joundi RA, Brittain JS, Jenkinson N, Green AL, Aziz T (2011) Rapid tremor frequency assessment with the iPhone accelerometer. Parkinsonism Relat Disord 17: 288-290.
Citation: Shah B, Mall S, Chhetri R, Yadav B, Dahal P, et al. (2017) A Review of Clinical Approach to a Patient with Tremor Disorder. J Alzheimers Dis Parkinsonism 7: 386. DOI: 10.4172/2161-0460.1000386
Copyright: © 2017 Shah B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7248
- [From(publication date): 0-2017 - Nov 13, 2025]
- Breakdown by view type
- HTML page views: 6211
- PDF downloads: 1037