Case Report Open Access
Achalasia in Pediatric Population: Use of High-Resolution Manometry in Children, Achalasia in Pediatric Population
González-Rodríguez Rebeca1, Ortiz-Olvera Nayeli X2*, González Martínez Marina3 and Flores-Calderón Judith4
1Servicio de Gastroenterología Pediátrica, Hospital de Pediatría, Centro Médico Nacional SXXI. IMSS, México
2Departamento de Gastroenterología, Hospital de Especialidades, Centro Médico Nacional SXXI, IMSS, México
3Laboratorio de motilidad, Servicio de Endoscopia, Hospital de Especialidades, Centro Médico Nacional SXXI, IMSS, México
4Servicio de Gastroenterología Pediátrica, Hospital de Pediatría, Centro Médico Nacional SXXI. IMSS, México
- *Corresponding Author:
- Nayeli Xochiquetzal Ortiz Olvera, M.D
Gastroenterology Department, UMAE
Hospital de Especialidades“Dr. Bernardo Sepúlveda”, Centro
Médico Nacional siglo XXI IMSS. Av. Cuauhtémoc 330
Colonia Doctores, Delegación Cuauhtémoc, CP. 06725
Mexico City, Mexico
Tel: 0155 56 27 69 00
Fax: 21565-21566
E-mail: nayelixoortiz@yahoo.com.mx
Received date: April 14, 2015; Accepted date: May 11, 2015; Published date: May 18, 2015
Citation: Rebeca GR, Nayeli XOO, Marina GM, Judith FC (2015) Achalasia in Pediatric Population: Use of High-Resolution Manometry in Children, Achalasia in Pediatric Population. J Gastrointest Dig Syst 5:286. doi:10.4172/2161-069X.1000286
Copyright: © 2015 Rebeca GR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Achalasia is a rare esophageal motor disorder in the pediatric population, it is characterized by symptoms that mimic common diseases in children as gastroesophageal reflux disease (GERD), behavioral and eating disorders (ED). The clinical spectrum in children can range from typical symptoms such as progressive dysphagia, chest pain and weight loss, until nocturnal cough, recurrent pneumonia, asthma, stridor, aspiration, vomiting and feeding difficulties. Children may have delayed development and eating disorders. It is a disease that affects the physical, behavioral and psychosocial sphere. We report three cases of children with complex clinical presentation, an 11-year old boy with feeding difficulties initially diagnosed as eating disorder and behavioral disorder, a 14-year old girl with non-cardiac chest pain and a girl with Allgrove syndrome who presented dysphagia at 7 years old. In all three cases, the final diagnosis was established with esophageal manometry, with typical findings described in adults. The aim of the study is to describe the diagnosis and management of achalasia in pediatric populations.
Keywords
Achalasia; Primary motor disorder; Dysphagia; Chest pain; Pediatric population
Introduction
Achalasia is a rare primary motor disorder of the esophagus, characterized by aperistalsis of esophageal body and impaired relaxation of the lower esophageal sphincter [1,2]. It is a condition that affects 1/100,000 adults, and less than 5% of cases occur during childhood. The estimated incidence in children´s less than 0.1/100,000 child-year [3-5].
The pathogenesis remains poorly understood. The most common symptoms are dysphagia, regurgitation, heartburn, vomiting, chest pain and weight loss, all of which can be confused with other diseases such as gastroesophageal reflux disease [6]. The diagnosis is established by clinical and imaging studies, such as endoscopy and manometry. Esophageal manometry is the gold standard in diagnosing achalasia, but it is not convenient to perform in children.
Recently, the development of high-resolution manometry (HRM) is leading to the replacement of conventional manometry. However, the experience with using HRM in children is limited [5]. Treatment is aimed at palliation of symptoms and improve esophageal emptying, and includes various forms: pharmacological, endoscopic and surgical [7].
We report 3 cases of pediatric patients with achalasia.
Case 1: Male, 11 Years-old, began his illness with decreased food intake conditioning acute malnutrition with weight loss of 20 kg in 4 months, initially attributed to an alteration of family dynamics (separation from parents). Physical examination was normal. Oncological, infectious, endocrinological etiology were discarded, among others.
Psychiatric evaluation was performed with a diagnosis of depression and eating disorder; it was decided to start handling with antidepressants and behavioral therapy without improvement.
Subsequently, progressive dysphagia and vomiting of food content was added. Esophago-gastro-duodenal (EGD) serie was performed with findings of gastro-esophageal reflux and failure of the diaphragmatic hiatus, so medical therapy antireflux was initiated; however, dysphagia was accentuated and a panendoscopy was performed, finding dilated upper and middle esophagus, with erosions in lower third involving less than 50% of the esophageal lumen (esophagitis grade II Hetzel), hiatal hernia by sliding and duodenitis.
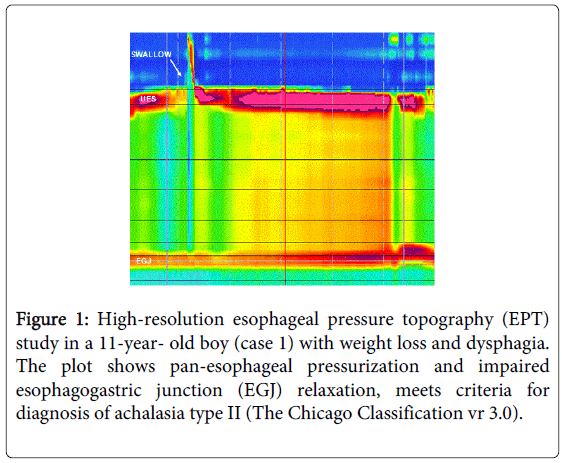
The histopathological report indicated esophagitis and chronic duodenitis. Suspecting motor impairment, high-resolution manometry (HRM) was performed, concluding with a diagnosis of type II achalasia (Figure 1).
Figure 1: High-resolution esophageal pressure topography (EPT) study in a 11-year- old boy (case 1) with weight loss and dysphagia. The plot shows pan-esophageal pressurization and impaired esophagogastric junction (EGJ) relaxation, meets criteria for diagnosis of achalasia type II (The Chicago Classification vr 3.0).
At age 12, he underwent Heller myotomy and partial fundoplication, both uncomplicated. The evolution after surgery was to clinical improvement, with gradual weight gain to recover nutritional status.
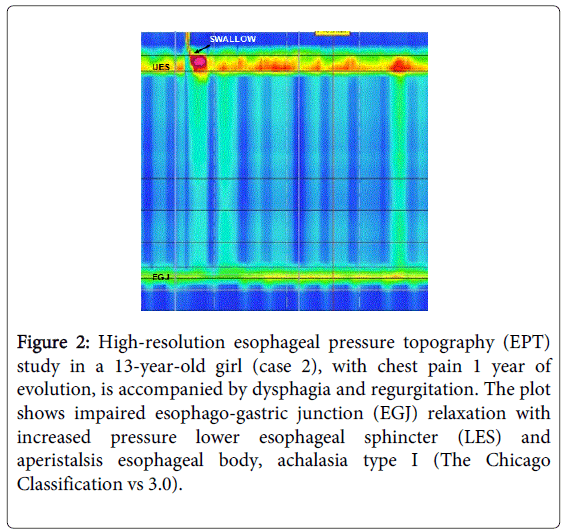
Case 2: Female 14 years with no history of importance. She began her illness at age 12 with retrosternal oppressive, intermittent, moderate chest pain without radiation. At 13, progressive dysphagia and vomiting of food content with weight loss of 8 kg were added. In the study protocol, EGD was performed, finding dilated esophagus picture with "bird´s beak sign" at the esophagogastric junction. Subsequently, we performed panendoscopy, documenting dilated esophagus with resistance to the passage of the endoscope at the esophagogastric junction. For suspected esophageal motor disorder, HRM was performed with diagnosis of achalasia type I (Classification of Chicago III) (Figure 2). Heller myotomy was performed, with a favorable clinical course, with weight recovery and improvement of nutritional status.
Figure 2: High-resolution esophageal pressure topography (EPT) study in a 13-year-old girl (case 2), with chest pain 1 year of evolution, is accompanied by dysphagia and regurgitation. The plot shows impaired esophago-gastric junction (EGJ) relaxation with increased pressure lower esophageal sphincter (LES) and aperistalsis esophageal body, achalasia type I (The Chicago Classification vs 3.0).
Case 3: Female, 8 years, with a history of older deceased brother at 3 years of age with symptoms of probable viral encephalitis, who clinically presented mucosal hyperpigmentation. At 18 months old corneal ulcers were detected and treated with topical steroid and eye lubricant, without clinical improvement. At age 4, she was referred to tertiary care for alacrima and non-queratocica hyperpigmentation of skin and mucous membranes in areas of flexion; skin biopsy detected nonspecific changes. In the boundary neuropsychological assessment (CI 74), for the 5th 4m she presented tonic-clonic seizures secondary to generalized hypoglycemia (glucose 30 mg/dl); determination of basal cortisol and cortisol stimulated with ACTH, was with given inferior to normal results, Cortisol 3.6 pc/ml, was initiated concluding failure adrenal; however renin, aldosterone and electrolytes were normal.
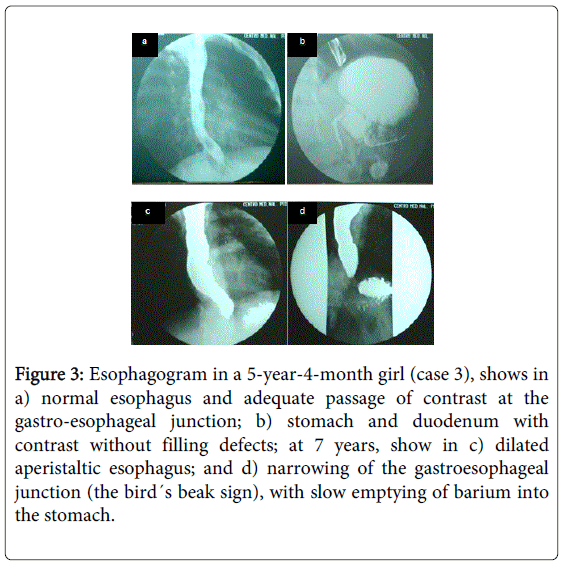
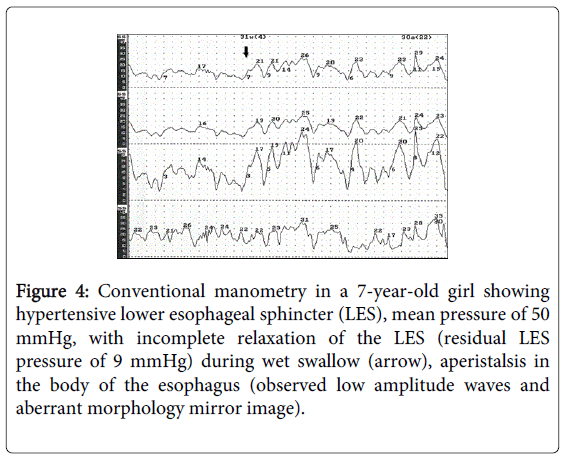
She had no postural drop in blood pressure. Also suspected was syndrome "AAA" EGD was made that was reported normal (Figure 3). At age 7, she presented dysphagia mainly to solids with poor weight gain that conditioned chronic malnutrition, new EGD was performed with new findings of dilated esophageal and narrowing of third distal with "the bird´s beak sign", (Figure 3) and conventional esophageal manometry ended in diagnosis of classical achalasia (Figure 4). At age 7 years 4 m laparoscopic Heller myotomy and partial anterior fundoplication was performed without complications. At present, the patient is 17 years old and continues management with steroid replacement, with good adherence to medical treatment, and denies digestive symptoms, with adequate nutritional status for age.
Figure 3: Esophagogram in a 5-year-4-month girl (case 3), shows in a) normal esophagus and adequate passage of contrast at the gastro-esophageal junction; b) stomach and duodenum with contrast without filling defects; at 7 years, show in c) dilated aperistaltic esophagus; and d) narrowing of the gastroesophageal junction (the bird´s beak sign), with slow emptying of barium into the stomach.
Figure 4: Conventional manometry in a 7-year-old girl showing hypertensive lower esophageal sphincter (LES), mean pressure of 50 mmHg, with incomplete relaxation of the LES (residual LES pressure of 9 mmHg) during wet swallow (arrow), aperistalsis in the body of the esophagus (observed low amplitude waves and aberrant morphology mirror image).
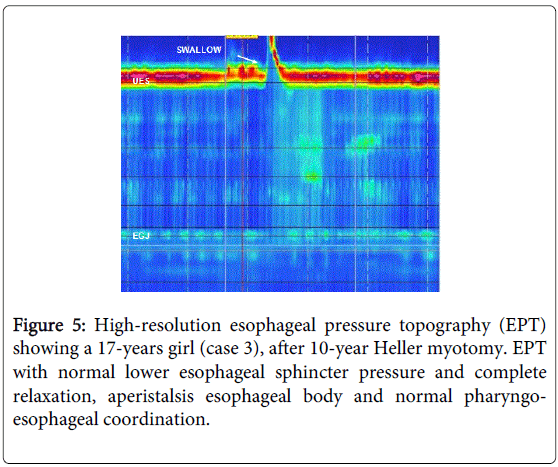
At 10 years of cardiomyotomy, panendoscopy control was performed with findings of dilated lower third esophagus, redundant esophageal folds, and fundoplication was competent; HRM with normal lower esophageal sphincter pressure and complete relaxation, aperistalsis of the esophageal body and normal pharyngoesophageal coordination (Figure 5). The patient met criteria of Allgrove syndrome.
Discussion
Achalasia is a rare neurodegenerative esophageal disorder in pediatric population. The disease is rarer in children under 5 years of age. The incidence in childhood is 0.11 / 100,000 children per year. Overall, fewer than 5% of patients with symptoms are under 15 years. The disease is more prevalent in males and is often idiopathic. Achalasia has been associated with trisomy 21, congenital hypoventilation syndrome, glucocorticoid insufficiency, eosinophilic esophagitis, familial dysautonomia, Chagas disease, and "AAA" syndrome (Achalasia, alacrima and insensitivity to ACTH), [1,3,8,9].
The pathophysiology is characterized by the selective loss of inhibitory neurons located in the myenteric plexus, resulting in alterations in relaxation of the lower esophageal sphincter (LES) and absence of peristalsis in the esophageal body. Loss or absence of myenteric ganglion cells, destruction or chronic inflammation, support the theory that abnormalities in the parasympathetic innervation of the esophagus result in disturbances of esophageal motility; however, the precise etiology of this disorder is still poorly understood [10]. In pediatric population, symptomatology is diverse, often having progressive dysphagia, which is the main reason for medical consultation, vomiting and weight loss [7], as reported in this series of cases. Young children and infants may present atypically as recurrent pneumonia, nocturnal cough, aspiration events, hoarseness and difficulty feeding; it is often misdiagnosed as GERD. Children may have delayed development, eating disorders or asthma, which in turn leads to a delay in diagnosis for a period of 6-10 years. Up to 50% of children are treated with antiacids or prokinetic before making the diagnosis of achalasia [9].
The diagnosis is based on clinical data, using the esophagogram (which typically shows a dilated esophagus with image of "bird´s beak" in distal esophagus), and confirmed with esophageal manometry [2,5,7]. Esophageal manometry is the gold standard in diagnosing achalasia, the high-resolution manometry (HRM) is leading to the replacement of conventional manometry; however, the experience with using HRM in children is limited. As with adult, achalasia can be classified into several subtypes according to manometric findings, as classified by Chicago: type I or classic is characterized by the failed relaxation of the lower esophageal sphincter but insignificant pressurization of the esophageal body is observed, unlike the esophageal Type II, which involves compression and pressurization. The type III or spastic achalasia, also associates with rapidly progressive pressurization; this is attributed to abnormal contraction obliterans of lumen [11]. However, the absence of these findings do not exclude the diagnosis of achalasia, because LES behavior in children is heterogeneous [12].
Different methods of the Achalasia treatment involve reducing LES pressure in order to facilitate esophageal emptying by: botulinum toxin injection, oral administration of calcium channel blockers (nifedipine), pneumatic dilation, or esophageal myotomy (Heller) with or without anti-reflux procedure. In children and adults, nifedipine is not the definitive treatment and only rarely should be used as a bridge to relieve symptoms, rather than to provide a definitive treatment [13].
Botulinum toxin is injected into the LES and acts on excitatory nerve terminals of the neuromuscular junction, which prevents the release of acetylcholine. The optimal dose and frequency of injection to relieve symptoms in children has not been well defined. After injection of botulinum toxin, duration of relief of symptoms is on average 4 months, often requiring multiple treatments for one year [14]. Pneumatic dilation (PD) or dilation of functionally obstructed esophagus has been used in children; we recommend using 35mm balls in children> 8 years. Multiple sessions of dilation is often required to achieve relief of symptoms with success, although the initial response predicts the success or failure of subsequent expansion.
Multiple studies indicate that in children older than 8 years, pneumatic dilation is the initial treatment of choice, recommended for its efficacy and safety. However, in pediatric population there are no follow-up studies to document the success rate of long-term PD. In patients with recurrence of symptoms, the treatment indicated is esophageal myotomy [15,16]. Laparoscopic Heller myotomy has been developed as the procedure of choice in the pediatric population [17]. Myotomy should be accompanied by an anti-reflux procedure as a prophylactic measure in all patients due to the high rate of complications from GERD (ulceration, stricture or Barrett's metaplasia). The Dor procedure has been described as effective as the Nissen, but with lower dysphagia rates (2.87 vs 15% respectively) [18].
Conclusions
Achalasia is a rare esophageal motility disorder associated with an insidious and progressive course, with several physical, behavioral and psychosocial features. It is estimated that up to 50% of achalasia patients are initially misdiagnosed, errors or delay in diagnosis unfortunately lead to delay in obtaining appropriate treatment. Clinicians should identify the wide spectrum of symptoms of pediatric achalasia for early treatment. The diagnosis requires esophageal manometry, as with adults, is characterized by lack of esophageal peristalsis, increased lower esophageal sphincter pressure, and partial or incomplete relaxation of the sphincter. The best treatment in children is controversial. Currently, the most effective treatment include cardiomyotomy with fundoplication and pneumatic dilatation; more recent treatment options for achalasia are promising, with the development of the novel minimally invasive endoscopic technique of peroral endoscopic myotomy.
References
- Richter JE (2010) Achalasia - an update. J Neurogastroenterol Motil 16: 232-242.
- Francis DL, Katzka DA (2010) Achalasia: update on the disease and its treatment. Gastroenterology 139: 369-374.
- Franklin AL, Petrosyan M1, Kane TD (2014) Childhood achalasia: A comprehensive review of disease, diagnosis and therapeutic management. World J Gastrointest Endosc 6: 105-111.
- Park W, Vaezi MF (2005) Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol 100: 1404-1414.
- Howard PJ, Maher L, Pryde A, Cameron EW, Heading RC (1992) Five year prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh. Gut 33: 1011-1015.
- Ambartsumyan L, Rodriguez L (2014) Gastrointestinal motility disorders in children. Gastroenterol Hepatol (N Y) 10: 16-26.
- Pohl D, Tutuian R (2007) Achalasia: an overview of diagnosis and treatment. J Gastrointestin Liver Dis 16: 297-303.
- Hallal C, Kieling CO, Nunes DL, Ferreira CT, Peterson G, et al. (2012) Diagnosis, misdiagnosis, and associated diseases of achalasia in children and adolescents: a twelve-year single center experience. Pediatr Surg Int 28: 1211-1217.
- Lee CW, Kays DW, Chen MK, Islam S (2010) Outcomes of treatment of childhood achalasia. J Pediatr Surg 45: 1173-1177.
- Francis DL, Katzka DA (2010) Achalasia: update on the disease and its treatment. Gastroenterology 139: 369-374.
- Bredenoord AJ, Fox M, Kahrilas PJ (2012) Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 1: 57-65.
- Morera C, Nurko S (2012) Heterogeneity of lower esophageal sphincter function in children with achalasia. J Pediatr Gastroenterol Nutr 54: 34-40.
- Chuah SK, Hsu PI, Wu KL, Wu DC, Tai WC, et al. (2012) 2011 update on esophageal achalasia. World J Gastroenterol 18: 1573-1578.
- Hurwitz M, Bahar RJ, Ament ME, Tolia V, Molleston J, et al. (2000) Evaluation of the use of botulinum toxin in children with achalasia. J Pediatr Gastroenterol Nutr 30: 509-514.
- Pastor AC, Mills J, Marcon MA, Himidan S, Kim PC (2009) A single center 26-year experience with treatment of esophageal achalasia: is there an optimal method? J Pediatr Surg 44: 1349-1354.
- Di Nardo G, Rossi P, Oliva S (2012) Pneumatic balloon dilation in pediatric achalasia: efficacy and factors predicting outcome at a single tertiary pediatric gastroenterology center. Gastrointest Endosc 76: 927-932.
- Gutschow CA, Töx U, Leers J, Schäfer H, Prenzel KL, et al. (2010) Botox, dilation, or myotomy? Clinical outcome of interventional and surgical therapies for achalasia. Langenbecks Arch Surg 395: 1093-1099.
- Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, et al. (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 240: 405-412.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 16937
- [From(publication date):
June-2015 - Aug 04, 2025] - Breakdown by view type
- HTML page views : 12185
- PDF downloads : 4752