Acute Pancreatitis Complicated by a Splenic Vein Non-Occlusive Thrombus
Received: 12-Jul-2018 / Accepted Date: 27-Jul-2018 / Published Date: 03-Aug-2018 DOI: 10.4172/2161-069X.1000573
Keywords: Acute pancreatitis; Splenic thrombosis; Portal vein thrombosis; Anticoagulation; Recanalisation
Introduction
Acute pancreatitis is one of the most common reasons for hospital admissions. It accounts for $2.5 billion of health care costs annually and 275,000 admissions per year [1]. The incidence of vascular complications in AP is low, however, it is mainly seen in severe AP such as those with pancreatic necrosis and peripancreatic collections [1]. Venous complications generally involve the splenic vein and less commonly the portal or superior mesenteric vein [2]. AP accounts for 60% of SVT diagnosis [3].
Of those patients who have developed a history of AP, they are immediately at 20% risk of developing SVT [3]. The other etiologies of SVT include malignancies, cirrhosis, pancreatic pseudocysts, and peptic ulcer disease. These listed can cause inflammation and inflict damage to the splenic vein wall making it more susceptible for thrombus formation [3]. Although elevated lipase and abdominal pain is sufficient to meet the diagnostic criteria for pancreatitis, imaging also plays a pivotal role to diagnose underlying complications including splenic vein thrombosis [4,5].
Contrast-enhanced computerized tomography (CECT) remains the imaging of choice as it is widely available and provides quick results [6]. Magnetic resonance imaging (MRI) is an alternative choice, which better characterizes the vascular complications compared to CECT [5]. The concerns of missing this diagnosis is detrimental as patients can develop life-threatening hemorrhage either through a splenic rupture or development of a pseudoaneurysm rupture [5]. Other complications include; subscapular hematoma, pseudocyst rupture, and splenic infarct [5]. The mortality rates of with vascular complications range from 0.8% to 3.5% [5]. Therefore, in AP we should have SVT in the differential when a patient presents with an acute on chronic attack of pancreatitis and underlying splenomegaly. This case report describes a female who developed a splenic thrombosis in the setting of an acute attack of pancreatitis.
Case Report
A 53-year-old female alcoholic abuser presented with complaints of epigastric abdominal pain radiating to the left shoulder. The patient had associated nausea and biliary non-bloody vomit. She denied ever having similar symptoms in the past but did report drinking four shots of vodka to “help her sleep” the night prior to her presentation. Her medical history was significant for anxiety, bipolar, and depression.
On presentation she was ill appearing with an abnormal pulse rate of 122/min, blood pressure of 97/65, WBC: 15.8/cmm with neutrophilic predominance (94%), Hg of 8.4g/dL, Hct 30.8%, ALT: 19 U/L, AST: 102 U/L, PLT: 374 K/μL, glucose: 138mg/dL, urea: 4 mg/dL, creatinine: 0.6 mg/dL, albumin: 3.4 g/dL, calcium: 8.8 mg/dL, triglycerides: 283 mg/dL, and lipase: 767 U/L. The rest of her laboratory parameters were unremarkable.
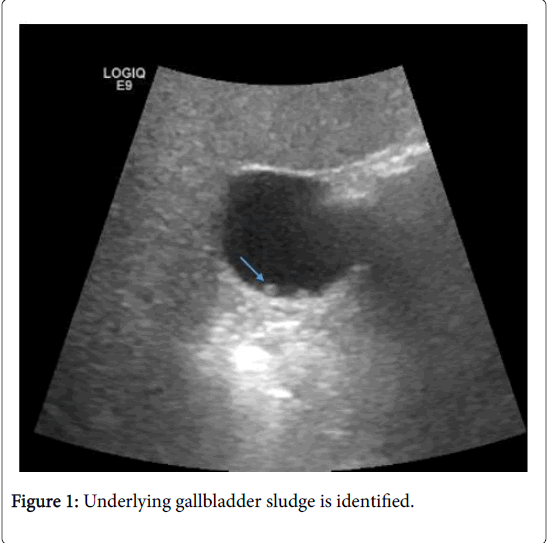
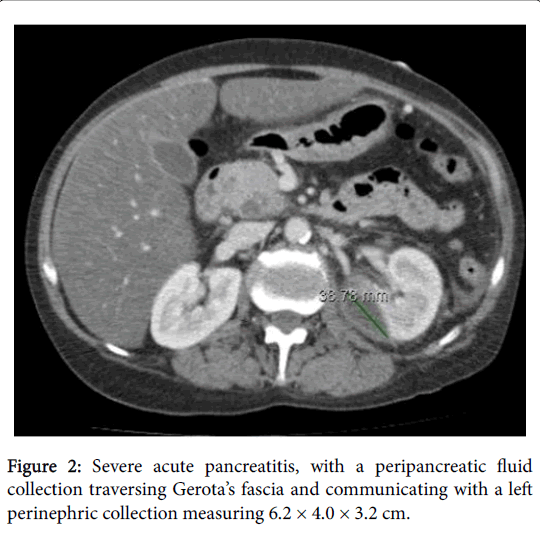
The abdominal ultrasonography was interpreted as having underlying gallbladder sludge, mildly dilated pancreatic duct, hepatic steatosis, and hepatomegaly (Figure 1). In the abdominopelvic contrast-enhanced computed tomography (CT), there was evidence of severe acute pancreatitis, with a peripancreatic fluid collection traversing Gerota’s fascia and communicating with a left perinephric collection measuring 6.2 × 4.0 × 3.2 cm representing pancreatic pseudocyst (Figure 2).
Septic thrombophlebitis of splenic vein, without complete occlusion was also identified. Associated abdominal and pelvic wall ascites were present. The patient was admitted and treated with supportive management for her acute pancreatitis and gastroenterology was consulted given the non-occlusive thrombus seen in the splenic vein.
The patient’s hemoglobin continued to drop reaching 6.2 mg/dL level. She initially refused work-up with an endoscopy; however, she was admitted within one week after leaving against medical advice. Her hospitalization the second time showed significantly worsening ascites. She agreed to get an endoscopy at that time which was remarkable for an acquired deformity of the gastric Cardia and noted red blood in the cardia without varices. This was thought to be secondary to the compressive effects of the pseudocyst.
The patient was also noted to have decompensated cirrhosis with coagulopathy during her second admission so she was not started on anticoagulation for non-occlusive splenic vein thrombosis. Subsequently, a stable splenic vein thrombosis was seen two weeks on a repeat CECT scan. There was however, a new finding of a splenic artery aneurysm which was embolized by interventional radiology.
Discussion
Splenic vein thrombosis is a rare complication of acute pancreatitis; however, early diagnosis is crucial to the management course [5]. Retrospective studies have demonstrated that CECT is useful to identify pancreatic necrosis and of those diagnosed, 53% of the patients are found to have SVT [6,7]. Thus far, it has been reported that patients with inflammation and compression by a peripancreatic collection or pancreatic necrosis should have imaging if the patient starts to deteriorate [8]. This will allow management change by diagnosing underlying hemorrhage which may have been missed due to severe pancreatitis. These patients will need to have multiple transfusion and embolization to be stabilized with close monitoring in the intensive care and intermediate level of care [9,10].
The incidence of vascular complications is commonly seen with a necrotic pancreatitis. However, even acute pancreatitis has shown to cause thrombosis likely due to the peripancreatic inflammation. Splenic vein thrombosis can increase the venous pressure giving rise to portal hypertension which manifests as further complication such as variceal bleeding [11]. This imposes a challenge in managing patients with portal vein thrombosis and weather to anti-coagulate them or not depends on the risk of gastrointestinal bleeding.
The treatment of vascular complications such as portal vein and splenic vein thrombosis remains controversial. The strategies have ranged from conservative management such as treating the acute pancreatitis, to bowel rest, anticoagulation, thrombolytic, and even surgery [7]. There have been case studies indicating that several patients achieved recanalisation in 40% of the time when they were anticoagulated [7]. More important, starting anticoagulation within one week demonstrated recanalisation in 60% of patients [7]. If the anticoagulation was delayed more than a week, the recanalisation rate would fall drastically to 25% [7]. European Associations for the Study of the Liver clinical practice guidelines recommended initiating anticoagulation early [10]. Reassuring enough, recanalisation was obtained more with early anticoagulation in splenic thrombosis (80% recanalized) when compared to portal vein thrombosis and superior mesenteric vein (39% and 73% recanalization respectively) [10]. Bleeding was seen in 9% of patients, while mortality occurred in 2% of patients with vascular complications.
Conclusion
Splenic vein thrombosis can be potentially a life-threatening complication of acute pancreatitis. There are limited data when it comes to anticoagulation of vascular complications from acute pancreatitis, however early diagnosis is crucial to help determine caseby- case who would benefit the most from anticoagulation. Furthermore, understanding the complication of vascular involvement from acute pancreatitis can help delay diagnosis of life threatening complications such as pseudoaneurysm rupture leading to hemorrhage.
American Association for the Study of Liver Disease acknowledges that the guidelines for anticoagulation of SVT or PVT are challenging [11]. There are observational studies which show that anticoagulation is associated with achieving recanalisation and lower the risk of recurrence. Nonetheless, it imposes an increased risk of gastrointestinal bleeding which should be kept in mind when treating these complicated patients [11]. Of those with gastrointestinal bleeding, 25% are found to have SVT [12]. Moreover, 55% of patients do not achieve recanalization. Therefore, anticoagulation should be used with caution with SVT especially if they are at high risk of bleeding. Strong evidence is scarce and there is a further need of randomized controlled trials. Decision should be made on a case-by case basis. The patient above was having an acute non-varcieal gastrointestinal bleeding evidenced by drop in hemoglobin and endoscopy findings. The patient was ultimately deemed high risk and not started on anticoagulation given the bleeding and the history of hepatic cirrhosis.
References
- Forsmark CE, Vege SS, Wilcox CM (2017) NEJM: Acute pancreatitis. N Engl J Med 375: 1972-1981.
- Park WS, Kim HI, Jeon BJ, Kim SH, Lee SO (2012) Should anticoagulants be administered for portal vein thrombosis associated with acute pancreatitis? World J Gastroenterol 18: 6168-6171.
- Heider TR, Azeem S, Galanko JA, Behrns KE (2004) The natural history of pancreatitis-induced splenic vein thrombosis. Ann Surg 239: 876-880.
- Ahmed M, Aziz MU, Mansoor MA, Anwar S (2016) Vascular complications in cases of acute pancreatitis-CT scan based study. J Pak Med Assoc 66: 977-989.
- Hernani BL, Silva PC, Nishio RT (2015) Acute pancreatitis complicated with splenic rupture: A case report. World J Gastrointest Surg 7: 219-222.
- Jiang W, Zhou J, Ke L (2014) Splanchnic vein thrombosis in necrotizing acute pancreatitis: Detection by computed tomographic venography. World J Gastroenterol 20: 16698-16701.
- Kikuchi M, Nishizaki Y, Tsuruya K (2014) Acute portal vein thrombosis due to chronic relapsing pancreatitis: A fistula between a pancreatic pseudocyst and the splenic vein. Clin J Gastroenterol 7: 52-57.
- Xie CL, Zhang M, Chen Y (2018) Spleen and splenic vascular involvement in acute pancreatitis: An MRI study. Quant Imaging Med Surg 8: 291-300.
- Riva N, Ageno W (2018) Timing of anticoagulation for portal vein thrombosis in liver cirrhosis: An Italian internist’s perspective. J Transl Int Med 6: 6-10.
- European Association for the Study of the Liver (2016) EASL clinical practice guidelines: Vascular diseases of the liver. J Hepatol 64: 179-202.
- Thatipelli MR, McBane RD, Hodge DO, Wysokinski WE (2010) Survival and recurrence in patients with splanchnic vein thromboses. Clin Gastroenterol Hepatol 8: 200-205.
- Senzolo M, Cholongitas EC, Patch D, Burroughs AK (2005) Update on the classification, assessment of prognosis and therapy of Budd-Chiari syndrome. Nat Clin Pract Gastroenterol Hepatol 2: 182-190.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5979
- [From(publication date): 0-2018 - Jul 16, 2025]
- Breakdown by view type
- HTML page views: 5126
- PDF downloads: 853