Case Report Open Access
Acute Superior Mesenteric Vein Thrombosis in a Patient with Primary Antiphospholipid Syndrome: A Case Report and Brief Review of the Literature
Steve Egwuonwu*
Department of Internal Medicine, Southwestern Medical Center, 5604 SW Lee Blvd, Suite 245, Lawton, Oklahoma, 73505, USA
- *Corresponding Author:
- Steve Egwuonwu
Department of Internal Medicine
Southwestern Medical Center
5604 SW Lee Blvd, Suite 245
Lawton, Oklahoma, 73505, USA
Tel: 580 531 4845
Fax: 580 531 6468
E-mail: steveoge76@yahoo.com
Received date: November 13, 2015, Accepted date: December 7, 2015, Published date: December 15, 2015
Citation: Egwuonwu S (2015) Acute Superior Mesenteric Vein Thrombosis in a Patient with Primary Antiphospholipid Syndrome: A Case Report and Brief Review of the Literature. J Gastrointest Dig Syst 5:360. doi:10.4172/2161-069X.1000360
Copyright:© 2015 Egwuonwu S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Acute superior mesenteric vein thrombosis is an uncommon but life threatening disease condition. In the setting of antiphospholipid syndrome, it is rare. This is a case of a 49 year old male who presented with a 2 day history of nausea, vomiting and abdominal pain. He had a previous history of deep vein thrombosis and pulmonary embolism about a year ago. Triple phase computed tomography confirmed superior mesenteric vein thrombosis. Lupus anticoagulant antibody was positive. He was initiated on heparin and then transitioned to warfarin. Given the finding of primary antiphospholipid syndrome, he is currently on lifelong anticoagulant therapy. Surgical resection, site directed thrombolysis and thrombectomy are other options of treatment for acute superior mesenteric vein thrombosis. With the diagnosis of acute superior mesenteric venous thrombosis, with or without any identifiable triggering factor, a search for hypercoagulable state is indicated. This will help determine the duration of anticoagulation therapy and prevent recurrent thrombosis. Acute Superior Mesenteric Vein Thrombosis in a Patient with Primary Antiphospholipid Syndrome: A Case Report and Brief Review of the Literature.
Keywords
Thrombosis; Antiphospholipid syndrome
Introduction
Acute superior mesenteric vein thrombosis is uncommon but lethal. In the setting of antiphospholipid syndrome, it is very rare. Antiphospholipid syndrome is defined by vascular thrombosis, pregnancy morbidity and persistent laboratory finding of one of the antiphospholipid antibodies. These antibodies include lupus anticoagulant, anticardiolipin and anti-B2 glycoprotein1 antibodies [1]. Antiphospholipid syndrome can be classified as primary or secondary. Primary antiphospholipid syndrome occurs without any associated systemic disease while secondary antiphospholipid syndrome coexists with an underlying disease such as systemic lupus erythematosus. This is the first case report of acute superior mesenteric vein thrombosis associated with primary antiphospholipid syndrome with positive lupus anticoagulant antibody.
Case Report
A 49-year-old male presented with two weeks history of left sided cramping abdominal pain and one day of vomiting. Abdominal pain worsened with eating. He denied any fever or chills. He had one episode of bloody stool a day before presentation to the hospital. Past medical history is significant for deep vein thrombosis and pulmonary embolism one year earlier. Family history is notable for a brother that died at age 35 years from a massive myocardial infarction. The patient
smoked one pack of cigarettes daily and had smoked for 20 years. He reported being told; he had a blood clotting disorder during his admission a year ago. He took warfarin for a couple of months and then stopped warfarin.
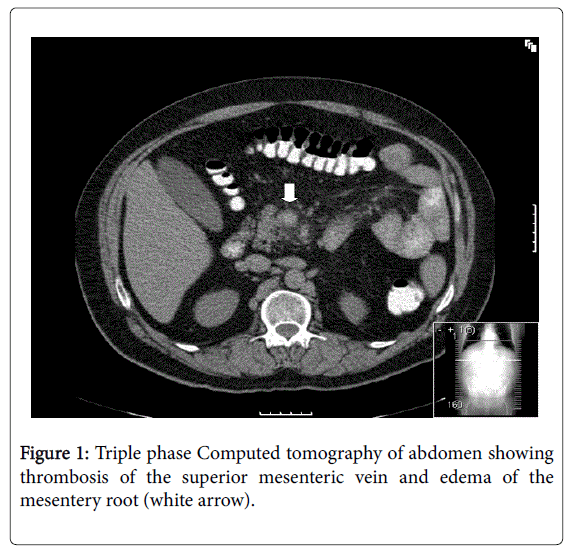
Chest and Cardiovascular examinations were within normal limits. Abdomen was soft, tender on palpation in epigastric and left hypochondrial area. Rectal exam revealed guaiac positive stool. Complete blood count, complete metabolic panel, lipase and amylase were all within normal limits. Triple phase computerized tomography of the abdomen showed thrombosis of the superior mesenteric vein (Figure 1).
Protein C, protein S, antithrombin III, and factor V Leiden were all normal. Prothrombin gene mutation was negative. Antinuclear Antibody, Anti-Double Stranded DNA and Anti-smith antibodies were negative. Rheumatoid factor, Anti CCP antibodies, Hepatitis C, HIV and Rapid plasma reagin (RPR) tests were all negative. Prothrombin time was 14 seconds.
Activated partial thromboplastin Time was 50 seconds. The Dilute Russell Viper Venom Time (DRVVT) was prolonged at 67 seconds. The prolonged DRVVT did not correct with mixing study. Hexagonal phase neutralization assay test was positive confirming lupus anticoagulant positivity in this patient.
The patient was started on heparin and eventually switched to warfarin on reaching therapeutic international normalized ratio (INR). He responded well to warfarin and did not require surgical exploration. Medical records from his previous admission were retrieved, and it did confirm lupus anticoagulant antibody. Given recurrent thrombosis and his family history as well as positive lupus anticoagulant antibody and absent underlying connective tissue disease, he was diagnosed with primary antiphospholipid syndrome. The patient is currently on lifelong warfarin therapy.
The patient was started on heparin and eventually switched to warfarin on reaching therapeutic international normalized ratio (INR). He responded well to warfarin and did not require surgical exploration. Medical records from his previous admission were retrieved, and it did confirm lupus anticoagulant antibody. Given recurrent thrombosis and his family history as well as positive lupus anticoagulant antibody and absent underlying connective tissue disease, he was diagnosed with primary antiphospholipid syndrome. The patient is currently on lifelong warfarin therapy.
Discussion
In 1952, Conley and Hartmann described venous thrombosis associated with lupus anticoagulant antibody [2]. Antiphospholipid Syndrome is characterized by arterial, venous or small vessel thrombosis, pregnancy complications and positive antiphospholipid antibodies which are present on 2 or more occasions, twelve weeks apart [1]. The commonest area of thrombosis in antiphospholipid syndrome is the deep veins of the calf. Superior mesenteric vein thrombosis may occur but is very rare in Antiphospholipid Syndrome. A review of the English Literature revealed only 5 case reports of acute superior mesenteric vein thrombosis in the setting of primary antiphospholipid syndrome [3-7]. This case is unique, in that it is the only case of acute mesenteric vein thrombosis with lupus anticoagulant positive primary antiphospholipid syndrome reported so far. Venous thrombosis is due to stagnant blood flow, vascular damage and a hypercoagulable state (Virchow’s triad) [8,9]. In this case report, smoking and discontinuation of warfarin in this patient with lupus anticoagulant antiphospholipid syndrome contributed to the development of superior mesenteric venous thrombosis. Acute superior mesenteric vein thrombosis has an incidence of 5-6% with a slight male to female preponderance [10,11]. The ileum is the most common site involved by superior mesenteric vein thrombosis (64-83%) followed by jejunum (50-81%), colon 14% and duodenum 4-8% [10,11].
Clinical features of acute superior mesenteric thrombosis include nausea and vomiting, anorexia, abdominal pain, fever, diarrhea, and bloody stools [3,4]. Bloody stools portend bowel ischemia or infarction. Hematemesis from esophageal varices may develop in chronic mesenteric venous thrombosis. Acute superior mesenteric vein thrombosis most frequently presented as abdominal pain (83%), anorexia (53%), nausea and vomiting (50%) and diarrhea (43%) [10]. Imaging studies reveal thrombosis in the mesenteric veins, establishing a definitive diagnosis of mesenteric venous thrombosis. Computed Tomography with contrast is the initial test of choice and is diagnostic in up to 90% of cases [12]. If this fails to make a diagnosis, and there is high clinical suspicion of thrombosis, CT angiography with delayed imaging or Magnetic resonance angiography may be done. Computed tomography findings of acute mesenteric venous thrombosis include a venous filling defect, bowel wall edema, mesenteric stranding and lack of flow in the mesenteric veins. CT findings of bowel wall thickening >3 mm and intestinal pneumatosis suggest intestinal infarction [13].
After diagnosis of acute superior mesenteric vein thrombosis without any identifiable predisposing or triggering factor, a search for hypercoagulable state is indicated to help determine the duration of therapy. This will help prevent recurrent thrombosis. Treatment of Acute mesenteric vein thrombosis involves bowel rest, anticoagulation to limit the extension of thrombosis and monitoring for any clinical deterioration. Surgical exploration is indicated for those with features of bowel infarction or peritonitis. Site directed thrombolysis with streptokinase, urokinase or tissue plasminogen activator (TPA) may be employed at specialized centers in severe thrombosis with poor response to anticoagulation and no signs of bowel infarction. Mechanical thrombectomy may be used when there is a contraindication to the use of anticoagulation. Duration of anticoagulation may vary from 6 months to lifelong.
Lifelong anticoagulation with warfarin is warranted in patients with hypercoagulable states.
Long term treatment with low molecular weight heparin can be a safe and effective alternative to warfarin in refractory thrombotic antiphospholipid syndrome [14,15]. The role of the new oral anticoagulants (rivaroxaban, apixaban, edoxaban, dabigatran etexilate) in the treatment of recurrent thrombosis in antiphospholipid syndrome is currently under study in ongoing controlled clinical trials.
Conclusion
Acute superior mesenteric vein thrombosis is a rare, but life threatening complication of antiphospholipid syndrome .Treatment of superior mesenteric vein thrombosis includes anticoagulation or surgical resection with bowel infarction. Lifelong anticoagulation is warranted when acute superior mesenteric vein thrombosis occurs in the setting of primary antiphospholipid syndrome.
References
- Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, et al. (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J ThrombHaemost. 4: 295-306
- Conley CL, Hartmann RC (1952) A hemorrhagic disorder caused by circulating anticoagulant in patients with disseminated lupus erythematosus. J Clin Invest 31: 621-2
- Resat O, Birgul M, Elif H, Ali M, Fehmi T (2003) Primary antiphospholipid syndrome: a cause of fever of unknown origin. Intern Med. 42: 358-361.
- Fried M, Van GW, Van A (2002) S.Mesenteric vein thrombosis triggered by blunt abdominal trauma in a patient with the primary antiphospholipid syndrome. Eur J. GastroenterolHepatol. 14: 697-700.
- Hwan WK, Tae HH, Mi HM, Keon H J (2010) Postoperative acute superior mesenteric venous thrombosis after cardiac surgery in a patient with anti-phospholipid syndrome. European Journal of Cardio-thoracic Surgery 37: 1230.
- Vacca A, Garau P, Cauli A, Mameli A, Mathieu A (2007) Primary antiphospholipid syndrome with mesenteric venous thrombosis presenting with intestinal infarction: a case description. Lupus 16: 455-456.
- Wan AW, Mohd SM, Hussein H (2011) Antiphospholipid Syndrome Presenting as Mesenteric Vein Thrombosis and Gangrenous Small Bowel. International Medical Journal Malaysia 10: 45-47.
- Dickson, BC (2004) Venous thrombosis: on the history of Virchow's triad.Univ Toronto Med J. 81: 166.
- Bagot CN, Arya R (2008) Virchow and his triad: a question of attribution. Br J Haematol 143: 180-190.
- Rhee RY, Gloviczki P, Mendonca CT, Petterson TM, Serry RD, et al. (1994) Mesenteric venous thrombosis: still a lethal disease in the 1990s. J VascSurg 20: 688.
- Abu-Daff S, Abu-Daff N, Al-Shahed M (2009) Mesenteric venous thrombosis and factors associated with mortality: a statistical analysis with five-year follow-up. J GastrointestSurg 13: 1245-1250.
- Taourel PG, Deneuville M, Pradel JA, Regent D, and Bruel JM (1996) Acute Mesenteric Ischemia: diagnosis with contrast enhanced CT. Radiology 199: 632.
- Lee SS, Ha HK, Park SH, Choi EK, Kim AY, et al. (2008) Usefulness of computed tomography in differentiating transmural infarction from nontransmural ischemia of the small intestine in patients with acute mesenteric venous thrombosis. J Comput Assist Tomogr 32: 730-737.
- Bick RL, Rice J (1999) Long-term outpatient dalteparin (fragmin) therapy for arterial and venous thrombosis: efficacy and safety- a preliminary report. ClinApplThrombHemost 5: S67- S71.
- Vargas-Hitos JA, Ateka-Barrutia O, Sangle S, Khamashta MA (2011) Efficacy and safety of long- term low molecular weight heparin in patients with antiphospholipid syndrome. Ann Rheum Dis 70: 1652-1654.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13315
- [From(publication date):
December-2015 - Sep 03, 2025] - Breakdown by view type
- HTML page views : 12361
- PDF downloads : 954