Research Article Open Access
Admission CRP Level as an Indicator for the Need of Percutaneous Cholecystostomy in Acute Cholecystitis
Eran Nizri*, Lilach Epstein, Amir Ben-Yehuda and Ron Greenberg
Department of Surgery, Tel Aviv Sourasky Medical Center, Tel-Aviv University, Tel- Aviv, Israel
- Corresponding Author:
- Eran Nizri
Department of Surgery, Weizman 6
Tel Aviv Medical Center, Tel- Aviv
Tel: 972-52-4266107
Fax: 03-6947659
E-mail: erann@tlvmc.gov.il
Received Date: March 11, 2016; Accepted Date: April 03, 2016; Published Date: April 11, 2016
Citation: Nizri E, Epstein L, Ben-Yehuda A, Greenberg R (2016) Admission CRP Level as an Indicator for the Need of Percutaneous Cholecystostomy in Acute Cholecystitis. J Gastrointest Dig Syst 6:413. doi:10.4172/2161-069X.1000413
Copyright: © 2016 Nizri E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Percutaneous cholecystostomy (PC) and conservative treatment are alternatives to surgery in patients with moderate acute calculous cholecystitis. Failure or non-improvement after conservative treatment is an indication for PC.
Aim: To investigate whether C-reactive protein (CRP) level on admission is associated with percutaneous cholecystostomy (PC) in patients with acute cholecystitis.
Methods: A database of patients admitted due to acute calculous cholecystitis and treated conservatively was assembled. Diagnosis was established clinical presentation and appropriate findings in imaging studies. Patients who underwent PC at admission due to organ failure or patients operated on index admission were excluded. Overall, 161 patients were identified, of whom 106 were treated conservatively and 55 were treated with PC. Data regarding the clinical presentation, comorbidities, physical examination and various laboratory parameters were retrieved from medical files.
Results: Patients who underwent PC were older and with higher American Society of Anesthesiologists score. The mean CRP level was higher for patients treated by PC than those treated conservatively (112.8 ± 10.6 mg/ml and 45 ± 5.3 mg/ml, respectively, p < 0.001). Mean WBC count did not differ between these two groups of patients (13.8 ± 1 K/mm3 and 12.2 ± 0.5 K/mm3, respectively, p = 0.15). Patients who underwent PC had higher frequency of acute (31% vs. 5.7%) and chronic renal failure (20% vs. 4.7%, for PC and conservative treatment, respectively).
Conclusion: Increased CRP level and renal failure are associated with the need for PC. These markers prompt early PC.
Keywords
Acute cholecystitis; C-Reactive protein (CRP); Percutaneous cholecystostomy; Conservative treatment; Aspirin treatment
Introduction
Acute calculous cholecystitis is a relatively common complication of gallstone disease, attributed to cystic duct obstruction by gallstones [1]. Patients usually present with right upper quadrant pain and tenderness, positive Murphy sign and fever. Common laboratory findings are inflammation related, such as: leukocytosis and increased levels of C-reactive protein (CRP).
Treatment of cholecystitis depends on disease severity and patient comorbidities [2,3]. Mild cholecystitis in a low operative risk patient is treated by laparoscopic early cholecystectomy [4,5]. On the other hand, patients presenting with severe cholecystitis, accompanied by sepsis and organ dysfunction are treated by percutaneous cholecystostomy (PC). Patients with moderate cholecystitis (defined by severe local inflammation), or patients with increased operative risk due to significant comorbidities (even with mild local disease), are treated by I.V antibiotics (further referred as conservative treatment). Moreover, technical and organizational difficulties hamper the implementation of early cholecystectomy even in surgically fit patients [6-9]. Thus, many patients are not operated at the same admission, but are treated conservatively. Failure to respond to conservative treatment, will eventually lead to PC. Currently, it is difficult to determine if a given patient will respond to conservative treatment or whether a PC will be needed to achieve clinical improvement and many patients are referred to PC after failure of conservative treatment [10]. This delay in PC performance entails many medical and economical consequences.
CRP is an acute phase reactant produced by hepatocytes under the regulation of IL-6. CRP levels are up-regulated during various inflammatory conditions and may be affected by a myriad of factors, including liver disease and medications [11]. In a previous study, we showed that increased CRP levels are associated with complicated diverticulitis, and may serve as a marker for the need of abdominal imaging [12]. We also showed that CRP levels retain their predictability even in patients taking aspirin, which is known to downregulate CRP production [13,14]. In the current study, we investigated whether increased CRP levels, as determined at admission, are associated with the need for PC.
Materials and Methods
Patients
Medical data of patients diagnosed with acute cholecystitis in the Tel-Aviv Sourasky Medical Center between January 2007 and March 2014 were retrieved from hospital electronic files. Patients with acalculous cholecystitis or patients who did not have CRP taken at admission were excluded. Patients who were operated on at the index admission were also excluded. Cholecystitis was diagnosed according to the revised Tokyo guidelines [2], i.e., the clinical and laboratory findings needed to be supported by appropriate imaging, either abdominal ultra-sound (AUS) or computerized tomography (CT). Radiological findings compatible with acute cholecystitis were: gallbladder distention, wall thickening, pericholecystic fluid and gallbladder wall enhancement. Laboratory data, as described below, were also collected from patient files. The study was approved by the Institutional Ethics Board of the Tel-Aviv Sourasky Medical Center.
Cholecystostomy
Patients who did not improve upon antibiotic treatment during 48-72 hours, or patients whose clinical situation aggravated (increased abdominal tenderness, appearance of fever, or increased inflammatory markers), were referred to PC. PC was done trans-hepatically and a pig-tail drain was left in the gallbladder for all cases.
Determination of inflammatory markers and laboratory tests
For each patient, CRP levels were recorded at admission. Blood count was determined using the Coulter STKS (Beckman Coulter, Nyon, Switzerland), and the high sensitivity CRP levels were determined using the Boering BN Nephlometer (DADE Boering, Marburg, Germany).
Other laboratory tests were also derived from patient electronic files. Acute renal failure (ARF) was defined as a new creatinine value above 1.3 mg/ml or an increase of more than 0.3 mg/ml from baseline creatinine. Chronic renal failure (CRF) was defined as a baseline creatinine level > 1.3 mg/ml.
Statistical analysis
Statistical analysis and receiver operator curve (ROC) were done using SPSS for Windows (ver. 17). For comparisons of frequencies between groups, the Chi-square test was performed. For comparisons of CRP and length of hospital stay, the t-test was performed. As CRP failed normality tests, we used the root transformation, which showed normal distribution. However, statistical analyses did not differ, and hence, we present the results of the parametric tests. Multivariate logistic regression analysis was performed using the Cox regression model to analyze predictors of failure of conservative treatment. The odds ratio, as well as its 95% confidence interval, was calculated for each of the independent variables. P < 0.05 was considered statistically significant. The statistical analysis in this work was conducted by the Biostatistic Unit of our institution.
Results
A total of 161 patients were included in this study. Of them, 106 were treated conservatively with I.V. antibiotics, whereas 55 underwent PC. Table 1 compares various clinical parameters between these two groups.
| Conservative Treatment | Percutaneous Cholecystectomy | p | |
|---|---|---|---|
| Number of patients (%) | 106 (66) | 55 (34) | |
| Male (%) | 46 (43) | 26 (47) | 0.63# |
| Age (±S.D.) | 61.8 ±18.6 | 81.4±9.5 | <0.001* |
| Aspirin use (%) | 27 (25) | 25 (45) | 0.01# |
| Length of hospital stay (days, ±S.D.) | 6.4±3.8 | 17.5±16.1 | <0.001* |
| High grade ASA score (%)† | 42 (40) | 46 (84) | <0.001# |
| 30-day mortality (%) | 2 (1.8) | 5 (9) | 0.03# |
| Time to admission (days) ‡ | 2.4±2.6 | 2.6±2.8 | 0.6 |
| Body temperature (°C, ±S.D.) § | 37.1±0.6 | 37.6±0.9 | 0.003* |
| Number of patients with peritonitis (%) | 6 (5.6%) | 5 (9%) | 0.41# |
| Number of patients with palpable mass | 3 (2.8%) | 5 (9%) | 0.09# |
Table 1: Comparison of clinical characteristics between patients treated conservatively and patients who underwent PC. † ASA- American Society of Anesthesiologists score. High grade considered grades 3-5. ‡ Time since symptoms appearance to emergency room admission. § As recorded on admission. * Student t-test, # Chi-square test.
Patients treated with PC were, on the average, older, with higher American Society of Anesthesiologists (ASA) scores, implying increased comorbidities, and with longer hospital stay .
Male sex was not associated with the need for PC. Importantly, mortality was also higher in patients with PC. Time to admission did not differ between the groups. Proportion of RUQ peritonitis and palpable abdominal mass did not differ between the two groups. However patients who needed PC had higher body temperature.
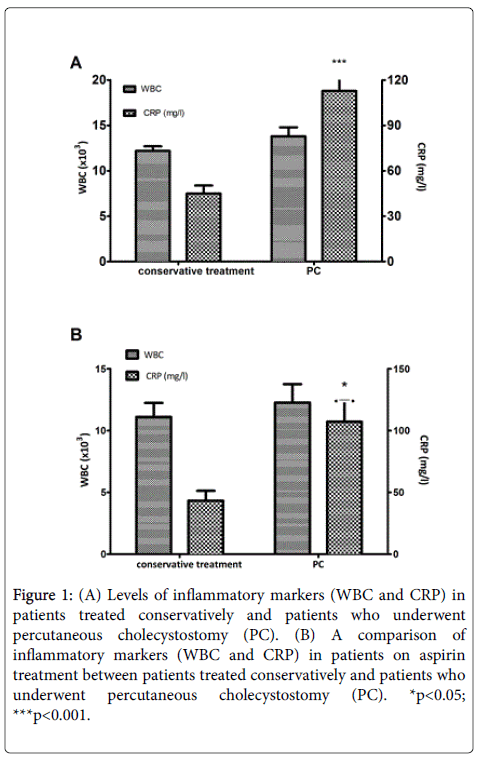
Mean levels of CRP were significantly higher among patients who underwent PC than among those who were treated conservatively (112.8 ± 10.6 mg/ml and 45 ± 5.3 mg/ml, respectively, p < 0.001) (Figure 1A). Mean WBC count did not differ between these two groups of patients (13.8 ± 1K/mm3 and 12.2 ± 0.5 K/mm3, respectively, p = 0.15). Overall aspirin usage was 32%. Even among patients taking aspirin, levels of CRP, but not WBCs were higher among those who underwent PC (107.2 ± 16.7 mg/ml and 43.3 ± 7.9 mg/ml, respectively, p = 0.04) (Figure 1B). Here, again, WBC count did not differ between these two groups of patients (p = 0.51).
Figure 1: (A) Levels of inflammatory markers (WBC and CRP) in patients treated conservatively and patients who underwent percutaneous cholecystostomy (PC). (B) A comparison of inflammatory markers (WBC and CRP) in patients on aspirin treatment between patients treated conservatively and patients who underwent percutaneous cholecystostomy (PC). *p<0.05; ***p<0.001.
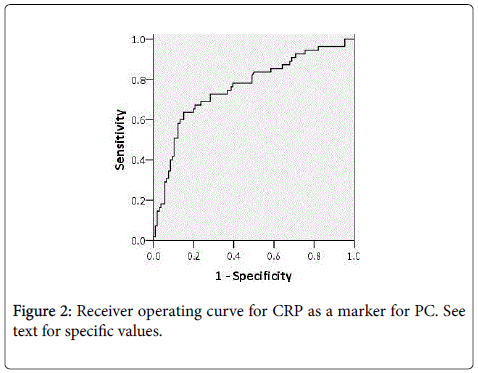
Using receiver operator curve (ROC) for determination of the CRP level with the highest sensitivity and specificity for PC, a CRP level of 47.6 mg/ml is associated with 73% sensitivity and specificity for PC (Figure 2). CRP value greater than 120 mg/ml had > 90% specificity to the need for PC. The area under the curve (AUC) for CRP is 0.76.
We examined whether other common laboratory tests that were previously reported to be abnormal in acute cholecystitis [15], differ between patients who underwent PC and those treated conservatively. Bilirubin levels were significantly increased (1.7 ± 1 .7 mg/dl vs. 1.15 ± 1.2 mg/dl, p=0.02) and albumin levels significantly decreased (35.5 ± 4.4 mg/dl vs. 39 ± 4.5 mg/dl, p<0.001), among patients who underwent PC. Alkaline phosphatase (ALP) (156.6 ± 176 u/l vs. 167.4 ± 183 u/l, for conservative treatment and PC, respectively, p=0.73) and INR ratios (1.1 ± 0.3 vs. 1.2 ± 0.3 for conservative treatment and PC, respectively, p=0.17) did not differ between the groups. Patients treated with PC had significantly higher creatinine levels (1.6 ± 1.1 mg/dl vs. 1.05 ± 0.3, p<0.001). However, creatinine levels at hospital admission can be either due to acute renal failure (ARF) or chronic renal failure (CRF). Hence, for each patient with increased blood creatinine, we distinguished ARF or CRF, as described above.
The proportion of patients with acute renal failure was higher in patients who underwent PC (n=17 (31%) vs. N=6 (5.7%), p<0.001). Similarly, the proportion of patients with chronic renal failure was also significantly higher (n=5 (4.7%) vs. N=11 (20%), p=0.002).
Table 2 shows a multivariate analysis for various risk factors associated with PC. Only age and CRP were significantly associated with PC. ASA score and ARF were almost statistically significant.
| Conservative Treatment | Percutaneous Cholecystectomy | P† | |
|---|---|---|---|
| Creatinine (mg/dl) | 1.05±0.3 | 1.6±1.1 | <0.001 |
| Bilirubin (mg/dl) | 1.15±1.2 | 1.7±1.7 | 0.02 |
| PT- INR | 1.1±0.3 | 1.2±0.3 | 0.17 |
| Albumin (mg/dl) | 39±4.5 | 35.5±4.4 | <0.001 |
| ALP (u/l) | 167.4±183 | 156.6±176 | 0.73 |
Table 2: Comparison of various laboratory tests between patients treated conservatively and patients treated with PC. † Student t-test. Results are presented ±S.D.
Discussion
In this study we demonstrated that increased CRP levels on admission are associated with the need for PC in patients with acute cholecystitis who are not candidates for cholecystectomy. The ability to predict the need for PC on admission can shorten patient suffering, save the time and costs of hospital admissions, and prevent complications resulting from treatment delay.
Similar to findings in other studies, patients who needed PC tended to be older and with higher ASA scores [16,17]. Accordingly, these patients had significantly longer hospital stay. In contrast to other reports [18-20], male sex was not a predictor of cholecystitis severity or of the need for PC in our patient cohort. Time to admission did not differ between groups, implicating that the need for PC is not due to neglected inflammatory process. However, others reported delayed treatment initiation as risk factor to severe cholecystitis [21].
Clinical presentation is also not predictive for the need for PC: although patients who underwent PC had elevated body temperature [17,20], the physical findings of localized RUQ peritonitis or palpable mass did not differ between groups. However, the retrospective design of our study which lacked standardized physical examination, prevent firm conclusions about this issue.
Here we report elevated CRP levels among patients who underwent PC, also among those taking aspirin (about 32% of the cohort). This is important, in light of the down-regulation of CRP production by aspirin previously reported [13]. Our group reported similar findings regarding the presence of complicated diverticulitis in patients taking aspirin [12]. Altogether, we can conclude that although aspirin downregulates CRP production, the pro-inflammatory stimulus exerted by the acute disease overcomes this effect. A CRP level of 47.6 provided the best discriminating value in terms of sensitivity and specificity (73%). The higher the CRP value, the more chance that patient will require PC, with CRP > 120 conferring > 90% for PC. White blood cell count did not differ between those who did and did not undergo PC.
Among other laboratory tests examined in patients referred for PC, bilirubin and albumin also significantly differed between groups. The rise in bilirubin levels was not associated with bile duct obstruction, as implied by the lack of bile duct dilation in imaging, in the majority of cases. Thus, this test seems to act as a marker for the severity of the inflammatory process, and not for a mechanical complication. Along the same line, the decrease in albumin, which was modest in absolute numbers, also represented the severity of inflammation and not malnutrition.
The incidence of both acute and chronic renal failure was increased in the PC group (Tables 3 and 4). This finding may represent the presence of two different patient populations among the PC group. Patients with fulminant local inflammation exert ARF as a systemic manifestation, and can be suspected to have severe cholecystitis. For patients with CRF, the creatinine level measured at admission has no relation to the severity of the inflammatory response, but either to their basic medical condition and comorbidities.
| Conservative treatment | Percutaneous Cholecystectomy | p† | |
|---|---|---|---|
| Number of patients with acute renal failure (%) | 6 (5.7%) | 17 (31%) | <0.001 |
| Number of patients with chronic renal failure (%) | 5 (4.7%) | 11 (20%) | 0.002 |
Table 3: Acute and chronic renal failure among patients treated with conservative treatment vs. patients treated with PC. † Chi-square test.
| OR | CI (95%) | p | |
|---|---|---|---|
| Age>75 | 4.8 | 2.21-6.52 | 0.001 |
| Acute renal failure | 3.55 | 0.97-13.03 | 0.056 |
| Palpated inflammatory mass | 3.43 | 0.52-22.53 | 0.199 |
| Sex | 0.947 | 0.39-2.28 | 0.904 |
| ASA score | 1.941 | 0.97-3.88 | 0.06 |
| CRP>50 mg/ml | 5.2 | 3.54-7.88 | 0.001 |
Table 4: Multivariate analysis (logistic regression) of various risk factors for PC.
This study has several limitations. First, due to its retrospective design, the criteria for PC referral were not determined prior to treatment decision, and were hence subject to individual clinical judgment. In addition, a significant number of patients were excluded from the study because of the absence of CRP levels on admission.
Our findings, of a higher mean CRP level among patients who needed PC should be interpreted cautiously. The complexity of clinical processes cannot be reduced to a single parameter to refer patients for a specific treatment. Thus, a careful use of any identified biomarker is advised. As observed in this study, a number of physical and laboratory parameters were found to be associated with PC. Hence, CRP levels should be used as an adjunct for clinical judgment and other clinical, imaging and laboratory parameters.
To conclude, we showed that the mean CRP level in patients who underwent PC was higher than among patients who underwent conservative treatment. We suggest that in the appropriate context, CRP can serve, as a biomarker for the need of PC and failure of conservative treatment. This is applicable also to patients taking aspirin. The use of biomarkers for treatment determination immediately at hospital admission merits further research for its presumed benefits for patients and caregivers.
References
- Duncan CB, Riall TS (2012) Evidence-based current surgical practice: calculous gallbladder disease.J Gastrointest Surg 16: 2011-2025.
- Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, et al. (2013) TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos).J Hepatobiliary Pancreat Sci 20: 35-46.
- Miura F, Takada T, Kawarada Y, Nimura Y, Wada K, et al. (2007) Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg 14: 27-34.
- Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR (2010) Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis.Br J Surg 97: 141-150.
- Gutt CN, Encke J, Köninger J, Harnoss JC, Weigand K, et al. (2013) Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304).Ann Surg 258: 385-393.
- Askew J (2005) A survey of the current surgical treatment of gallstones in Queensland.ANZ J Surg 75: 1086-1089.
- Cameron IC, Chadwick C, Phillips J, Johnson AG (2004) Management of acute cholecystitis in UK hospitals: time for a change.Postgrad Med J 80: 292-294.
- Pieniowski E, Popowicz A, Lundell L, Gerber P, Gustafsson U, et al. (2014) Early versus delayed surgery for acute cholecystitis as an applied treatment strategy when assessed in a population-based cohort.Dig Surg 31: 169-176.
- Yamashita Y, Takada T, Hirata K (2006) A survey of the timing and approach to the surgical management of patients with acute cholecystitis in Japanese hospitals.J Hepatobiliary Pancreat Surg 13: 409-415.
- Little MW, Briggs JH, Tapping CR, Bratby MJ, Anthony S, et al. (2007) Percutaneous cholecystostomy: the radiologist's role in treating acute cholecystitis. Clin Radiol 68: 654-660.
- Pepys MB, Hirschfield GM (2003) C-reactive protein: a critical update.J Clin Invest 111: 1805-1812.
- Nizri E, Spring S, Ben-Yehuda A, Khatib M, Klausner J, et al. (2014) C-reactive protein as a marker of complicated diverticulitis in patients on anti-inflammatory medications.Tech Coloproctol 18: 145-149.
- Benhamou M, Gossec L, Dougados M (2005) Clinical relevance of C-reactive protein in ankylosing spondylitis and evaluation of the NSAIDs/coxibs' treatment effect on C-reactive protein. Rheumatology (Oxford) 49: 536-541.
- Ho GY, Xue X, Cushman M, McKeown-Eyssen G, Sandler RS, et al. (2009) Antagonistic effects of aspirin and folic acid on inflammation markers and subsequent risk of recurrent colorectal adenomas.J Natl Cancer Inst 101: 1650-1654.
- Nguyen L, Fagan SP, Lee TC, Aoki N, Itani KM, et al. (2004) Use of a predictive equation for diagnosis of acute gangrenous cholecystitis.Am J Surg 188: 463-466.
- Abi-Haidar Y, Sanchez V, Williams SA, Itani KM (2012) Revisiting percutaneous cholecystostomy for acute cholecystitis based on a 10-year experience.Arch Surg 147: 416-422.
- Barak O, Elazary R, Appelbaum L, Rivkind A, Almogy G (2009) Conservative treatment for acute cholecystitis: clinical and radiographic predictors of failure.Isr Med Assoc J 11: 739-743.
- Fagan SP, Awad SS, Rahwan K, Hira K, Aoki N, et al. (2003) Prognostic factors for the development of gangrenous cholecystitis.Am J Surg 186: 481-485.
- Yacoub WN, Petrosyan M, Sehgal I, Ma Y, Chandrasoma P, et al. (2010) Prediction of patients with acute cholecystitis requiring emergent cholecystectomy: a simple score. Gastroenterol Res Pract 2010: 901739.
- Nikfarjam M, Shen L, Fink MA, Muralidharan V, Starkey G, et al. (2005) Percutaneous cholecystostomy for treatment of acute cholecystitis in the era of early laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 23: 474-480.
- Contini S, Corradi D, Busi N, Alessandri L, Pezzarossa A, et al. (2004) Can gangrenous cholecystitis be prevented?: a plea against a "wait and see" attitude.J Clin Gastroenterol 38: 710-716.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13650
- [From(publication date):
April-2016 - Aug 18, 2025] - Breakdown by view type
- HTML page views : 12703
- PDF downloads : 947