Analysis for the Success Rate of Patients after Laparoscopic Sleeve Gastrectomy
Received: 12-Oct-2017 / Accepted Date: 31-Oct-2017 / Published Date: 06-Nov-2017 DOI: 10.4172/2165-7904.1000355
Abstract
Background: Success rate of laparoscopic sleeve gastrectomy (SG) depends on disease and patient characteristics that are yet to be fully established.
Objectives: To evaluate which patient characteristics influence the success of SG.
Setting: National bariatric reference centre at a Public Hospital.
Methods: A retrospective study was performed based on prospectively collected data of patients who had bariatric surgery at our institution, during a 5 year period. Patients with 12 or more months of follow-up were included. We analyzed data from 133 SG. Seventy-nine percent of the patients were female with a median age of 46 years, a median baseline Body Mass Index (BMI) of 41 kg/m2 and a mean of 2.5 out of 7 comorbidities.
Results: After the first year, the mean percentage Excess Weight Loss (%EWL) was 69.3%, the mean change in BMI was -11.8 kg/m2 and the mean % total body weight loss was 27.4%. Surgical success (%EWL ≥ 50%) was achieved in 82% of the patients, with significant improvement or resolution of comorbidities (follow-up rate 76%-88%). We found statistical significant differences with baseline BMI (p<0.0001), with OSA (p<0.0001), with age (p=0.04) and with the number of comorbidities (p=0.05). Higher baseline characteristics implicated less %EWL. The presence of HTN or arthropathy and being a volume eater or a sweet eater did not influence surgical success (χ2 ≤ 0.01).
Conclusions: SG is an effective surgical treatment for obesity. After one year the majority of patients had surgical success and major comorbidities were mitigated or resolved. Success was influenced by specific patient and disease characteristics.
Keywords: Obesity; Morbidity; Bariatric surgery; Gastrectomy; Laparoscopy; Treatment outcome
Introduction
Obesity keeps on growing as a global epidemic. In 2014, the World Health Organization (WHO) reported over 600 million obese adults, this number has more than doubled since 1980. This means that 13% of the world’s population has a Body Index Mass (BMI) ≥ 30 kg/m2 [1]. In 2008, in Portugal about 24% of the population had obesity and 59% was overweight [2]. Bariatric surgery is an effective treatment for severe obesity that leads to the improvement and remission of many obesity-related comorbidities, sustained weight loss over time, improvement in quality of life and prolonged survival [3,4].
Sleeve Gastrectomy (SG) was first described as the initial step in a proposed two-stage approach to Duodenal Switch (DS), in an effort to reduce the morbidity and mortality of performing DS in high-risk patients with extreme obesity (specifically, patients with BMI >60 kg/m2) [5]. However, data began to show that SG is an effective primary bariatric operation without the need for a second-stage conversion to DS [6]. By late 2000s, the SG had established itself as another primary bariatric operation. The most commonly performed procedure worldwide is the Roux-en-Y Gastric Bypass (RYGB), 45%, followed by the SG, 37%, whereas the most common bariatric procedure in the USA is the SG and this probably shows the world’s trend [7,8].
The aim of our study was to bring more evidence to the scientific community, evaluating SG outcomes, concerning efficiency and safety and researching which patient’s characteristics influenced surgical success. We hope to aid procedure choice, help to better manage patient’s expectations and support adequate contextualization of the results obtained.
Materials and Methods
At our institution, data from patients treated for severe obesity are regularly registered in a prospective longitudinal Microsoft Access 2010® database. An observational study was designed, including a 5 year period, from January 2009 to December 2013, and a retrospective analysis was performed. Our group performed 142 SG, of which 133 had more than 12 month follow-up. For the calibration of the SG, an endoluminal 36F bougie was used. Gastric transection was performed using an Endo GIA™ Universal Loading Unit 45-60 mm (green 4.8 mm or blue 3.5 mm reloads) and a reinforcement suture, using 2/0 polypropylene, was always performed.
Twenty-two variables were statistically analyzed: age, gender, number of comorbidities, presence or absence of seven specific comorbidities (hypertension, dyslipidemia, obstructive sleep apnea, arthropathy, type 2 diabetes mellitus, coronary artery disease and infertility), baseline BMI, weight and excess weight, number of meals per day, duration of obesity, four types of eating behavior, previous obesity treatments, interference with everyday life activities and obesity-related depression. Statistical tests were applied when appropriate, using IBM SPSS Statistics 22®, namely χ2 (chi-square), tstudent and Pearson’s correlation.
Results
Baseline patients’ demographics are presented in Table 1. The cohort had a median age of 46 years and a male-to-female ratio of 1:3:8, 46% had between 8 to 12 years of school education, 53% had nonspecialized job or were unemployed and 57% earned a fixed wage.
| Statistics | Results |
|---|---|
| Age (median, years) | 46 [min 20, max 65] |
| Gender | Male 21% (n=28); Female 79% (n=105) |
| Comorbidities | |
| HTN | 57% (n=76) |
| Dyslipidemia | 56% (n=75) |
| OSA | 56% (n=75) |
| Arthropathy (related to obesity) | 50% (n=66) |
| DM2 | 24% (n=32) |
| CAD | 6% (n=8) |
| Infertility | 1% (n=1) |
| Obesity (median) | |
| Weight (kg) | 112.0 [min 84, max 167] |
| Excess weight (kg) | 44.3 [min 20, max 92] |
| BMI (kg/m2) | 41.4 [min 32, max 62] |
Table 1: Baseline population analysis (n=133); [HTN: Hypertension, OSA: Obstructive Sleep Apnea, DM2: Type 2 Diabetes Mellitus, CAD: Coronary Artery Disease, BMI: Body Mass Index].
They had a median baseline BMI of 41.4 kg/m2 (minimum 32 and maximum 62 kg/m2), had 3.1 meals per day, 59% showed an eating pattern of volume eater (big volumes of food intake in few meals), 21% of sweet eater (preference for sugar based foods) and 20% were craving eaters (permanent eating compulsion). Mean duration of the disease was 22 years, 70% had already enrolled in non-surgical obesity treatments before, 71% mentioned that obesity interfered with their everyday life activities and 30% had obesity related depression.
Patients were asked explicitly about seven comorbidities and registered a mean of 2.5 comorbidities (Table 1). Median hospital stay was 4 days. At the period of the study, patients were admitted on the day before surgery and some of them had also secondary procedures performed (i.e. complementary cholecystectomy).
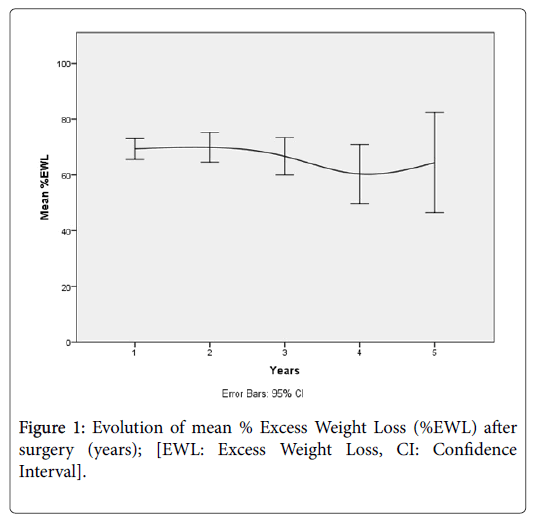
The weight loss results and the surgical success (defined as %EWL ≥ 50%) are displayed in Table 2 and Figure 1.
| Time (years) | n | TWL (%) | ΔBMI (kg/m2) | EWL (%) | Surgical Success(%EWL ≥ 50%) |
|---|---|---|---|---|---|
| 1 | 133 | 27.4 [26, 29] | -11.8 [-12, -11] | 69.3 [66,73] | 82% |
| 2 | 68 | 28.3 [26, 30] | -12.3 [-13, -11] | 69.9 [65,75] | 79% |
| 3 | 51 | 27.7 [25, 31] | -12.4 [-14, -11] | 66.7 [60,73] | 73% |
| 4 | 18 | 25.6 [20, 31] | -11.3 [-14, -8] | 60.3 [50,71] | 72% |
| 5 | 6 | 29.2 [18, 40] | -13.5 [-20, -7] | 64.4 [47,82] | 83% |
Table 2: Weight loss after surgery (mean); [95% confidence interval, TWL: Total Body Weight Loss, ΔBMI: Change in Body Mass Index, EWL: Excess Weight Loss].
Twelve months after surgery, more than 90% of the patients had a partial or total resolution of obstructive sleep apnea (OSA), Type 2 diabetes mellitus (DM2) and hypertension (HTN), Table 3.
| Comorbidity | Totally Resolved | Partial or Totally Resolved |
|---|---|---|
| OSA (n=57) | 84% | 95% |
| DM2 (n=28) | 68% | 93% |
| HTN (n=64) | 64% | 92% |
| CAD (n=5) | 40% | 60% |
| Arthropathy (n=34) | 32% | 70% |
| Dyslipidemia (n=57) | 23% | 46% |
Table 3: Evolution of comorbidities after surgery (12 months).
Eighty-seven percent (n=115) of patients were complication free. We analysed early and late complications separately.
We used the Clavien-Dindo classification to stratify early complications and registered nine grade I complications, two grade II, six grade III, one grade IV and no mortality [9]. We registered four (3.0%) gastric fistulas.
Grade I complications include two incision bleedings, two seromas, two superficial surgical wounds infections, one skin dehiscence, one acute kidney failure and one low flow biliary fistula (after cholecystectomy).
Grade II include one traumatic ulcer of the cornea and one superficial wound infection that was treated with antibiotic therapy.
Grade III included the four gastric fistulas already mentioned, one gastric stenosis and one biliary fistula.
The Grade IV complication was a bilateral nosocomial pulmonary infection.
Only three patients had late complications: two (1.5%) developed gastro-esophageal reflux, refractory to medical treatment, and one had primary surgical failure (insufficient weight loss). All three were reoperated and a Roux-en-Y gastric bypass was performed.
Predictors of success
One year after surgery, we found that surgical success (%EWL ≥ 50%) presented statistically significant differences depending on baseline BMI (p<0.0001), age (p<0.05) and the number of comorbidities (p<0.05), especially in the presence of OSA (p=0.01), Table 4 and 5.
| Statistics | Surgical Success (%EWL ≥ 50%) | Δ | t-student | |
|---|---|---|---|---|
| With | Without | |||
| BMI (kg/m2) | 43.5 | 49.1 | -5.6 | p<0.0001 |
| Age (years) | 43.8 | 48.7 | -4.9 | p=0.040 |
| Number comorbidities | 2.4 (of 7) | 3.1 (of 7) | -0.7 | p=0.045 |
Table 4: Baseline characteristics of patients with or without surgical success; [BMI: Body Mass Index before surgery].
| Comorbidity | Present | Not Present | Δ | χ2 |
|---|---|---|---|---|
| HTN | 81.6% | 82.5% | -0.9 | p=0.896, χ2=0.017 |
| Dyslipidemia | 77.3% | 87.9% | -10.6 | p=0.115 |
| OSA | 74.7% | 91.4% | -16.7 | p=0.013 |
| Arthropathy | 81.8% | 82.1% | -0.3 | p=0.968, χ2=0.002 |
| DM2 | 71.9% | 85.1% | -13.2 | p=0.089 |
| CAD | 62.5% | 83.2% | -20.7 | p=0.140 |
| Infertility | 100% | 81.8% | +18.2 | p=0.638 |
Table 5: Surgical success with baseline comorbidity (n=133); [OSA: Obstructive Sleep Apnea, HTN: Hypertension, DM2: Type 2 Diabetes Mellitus, CAD: Coronary Artery Disease].
Looking into the relationship between baseline BMI and %EWL, we observed a moderate negative correlation (r=-0.445), and also a weak negative correlation between age and number of comorbidities and %EWL (r=-0.201 and -0.251 respectively). We observed further, that patients with OSA had a smaller %EWL (64% vs. 77%, p<0.0001).
We also noted differences in the surgical success rate of patients with type 2 diabetes mellitus (DM2) or dyslipidemia, but these differences did not reach statistical significance (p=0.089 and p=0.115 respectively). The presence of HTN or arthropathy did not change surgical success (χ2 ≤ 0.02), Table 5. Enrollment in previous obesity treatment programs seemed to positively influence surgical success (85% vs. 75%), but this difference did not have statistical significance (p=0.171). We also found differences, although with no statistical significance, with gender, number of meals per day and duration of obesity.
The eating patterns of volume eater or sweet eater did not influence surgical success (χ2=0.001). Being a craving eater did influence surgical results, but with no statistical significance (p=0.336). Obesity related depression did not alter surgical success (χ2=0.005).
Discussion
The expected %EWL at twelve months after SG lies between 51 and 70% [10,11]. Our cohort had a mean of 69% EWL after one year, maintaining this weight loss in the second year, but showing a minor tendency of weight regain after that. Nevertheless, the big majority of patients maintained surgical success (72%) during the study’s timeframe. We collected data up to five years after surgery, but the follow-up is notoriously small at five years (n=6), representing only 4.5% of the patients initially included. The dropout rate is 49% at 2 years, 62% at 3 years and 86% at 4 years, limiting midterm conclusions.
Besides surgical procedure, baseline BMI and age seem to be the most important predictors of a greater %EWL and consequent surgical success. This relation was observed in our analyses with clear statistical significance (p<0.0001 and p=0.04 respectively). In some studies, type-2 diabetes appears to have influence in the success [12-17]. In our data we found a slight difference with diabetes, but it did not reach statistical significance (p=0.089). Other predictors of success sometimes found in literature are HTN, dyslipidemia and gender [13-16]. There were small differences with dyslipidemia and gender, again without reaching statistical significance, but there was no difference with HTN.
A greater number of comorbidities seems to worsen results (p=0.045), mainly OSA, DM2 and dyslipidemia, OSA being the one that had the strongest statistical significance (p<0.0001). Patients with one or more of these three comorbidities sometimes also have Metabolic Syndrome which could help explain the worse results of these patients after SG. This group of patients should eventually be proposed for other bariatric procedure, rather than SG.
In our study’s data we registered four gastric fistulas (3.0%) that were treated with no sequels. However, our surgical unit has a global incidence of fistulas of 1.9% (n=4) after 215 SGs performed, below the typical values of this complication (2.2%) [18]. The incidence of complications was 13.5%, but only 5.2% (n=7) were severe complications (grade III and IV) and we registered no mortality [9]. The main limitations of this study are its retrospective nature, based on prospectively collected data, and to only include 133 SGs with a large dropout rate after de first year.
Conclusion
Our data on SG shows that it can significantly promote weight loss and resolve or mitigate important comorbidities, contributing to the improvement of the patient’s quality of life.
Treatment success depends on disease severity, patient’s characteristics like age and comorbidities and these should be taken into account when choosing the best fitting procedure for the patient and his disease. There are still lacking long-term studies to settle SG’s efficiency over time and to continue establishing the predictors of this efficiency.
Conflicts of interest
We declare no conflicts of interest.
References
- World Health Organization (2013) Portugal: Nutrition, Physical Activity and Obesity.
- G. Mingrone (2015) Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single center, randomized controlled trial. Lancet 386: 964-973.
- NIH Conference (1991) Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med 114: 956-961.
- J P Regan, W B Inabnet, M Gagner, A Pomp (2003) Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg 13: 861-864.
- American Society for Metabolic and Bariatric Surgery (2012) Updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis 8: 21-26.
- J Ponce, N T Nguyen, M Hunter, R Sudan, J M Morton (2015) American Society for Metabolic and Bariatric Surgery estimation of bariatric surgery procedures in the United States, 2011-2014. Surg Obes Relat Dis 11: 1199-2000
- L. Angrisani (2015) Bariatric surgery worldwide 2013. Obes Surg 25: 1822-1832.
- P Clavien, J Barkun, M Oliveira, J Vauthey, D Dindo (2009) The Clavien-Dindo classification of surgical complications: Five-year experience. Ann Surg 250: 187-196.
- M Parikh, R Issa, A McCrillis, J Saunders, A Ude-Welcome, et al. (2013) Surgical strategies that may decrease leak after laparoscopic sleeve gastrectomy: A systematic review and meta-analysis of 9991 cases. Ann Surg 257: 231-237.
- S H Chang (2014) The effectiveness and risks of bariatric surgery: An updated systematic review and meta-analysis, 2003–2012. JAMA Surg 149: 275-287.
- S Benoit, T Hunter, D Francis, N De La Cruz-Munoz (2014) Use of bariatric outcomes longitudinal database (BOLD) to study variability in patient success after bariatric surgery. Obes Surg 24: 936-943.
- D Martin, C Lee, G Rigas, C Tam (2015) Predictors of weight loss 2 years after laparoscopic sleeve gastrectomy. Asian J Endosc Surg 8: 328-332.
- J Andersen, E Aadland, R Nilsen, V Vage (2014) Predictors of weight loss are different in men and women after sleeve gastrectomy. Obes Surg 24: 594-598.
- A Parri, D Benaiges, H Schroder, M Isquierdo-Pulido, J Ramon (2015) Preoperative predictors of weight loss at 4 years following bariatric surgery. Nutr Clin Pract 30: 420-424.
- E Ortega, R Morinigo, L Flores, V Moize, M Rios, et al. (2012) Predictive factors of excess body weight loss 1 year after laparoscopic bariatric surgery. Surg Endosc 26: 1744-1750.
- A de Hollanda, T Ruiz, A Jimenez, L Flores, A Lacy, et al. (2014) Patterns of weight loss response following gastric bypass and sleeve gastrectomy. Obes Surg 25: 1177-1183.
- Brethauer A, Hammel J, Schauer P (2009) Systematic review of sleeve gastrectomy as staging and primary. Surg Obes Relat Dis 5: 469-475.
Citation: Baptista J, Praxedes V, Andre A, Rosa E, Trindade C, et al. (2017) Analysis for the Success Rate of Patients after Laparoscopic Sleeve Gastrectomy. J Obes Weight Loss Ther 7:355. DOI: 10.4172/2165-7904.1000355
Copyright: © 2017 Baptista J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5397
- [From(publication date): 0-2017 - Dec 22, 2025]
- Breakdown by view type
- HTML page views: 4471
- PDF downloads: 926