Antenatal Depression and Risk of Complications in the Mother and the Newborn: A Retrospective Cohort Study
Received: 29-Jan-2024 / Manuscript No. JPCH-24-126274 / Editor assigned: 31-Jan-2024 / PreQC No. JPCH-24-126274 (PQ) / Reviewed: 14-Feb-2024 / QC No. JPCH-24-126274 / Revised: 08-Jan-2025 / Manuscript No. JPCH-24-126274 (R) / Published Date: 15-Jan-2024
Abstract
Objective: To analyse the relationship between depression and complications of pregnancy and the newborn in the Lleida health region.
Materials and methods: Retrospective observational cohort study in pregnant women between 2012-2018 in the Lleida health region. Variables included age, Body Mass Index (BMI), caesarean section, pre eclampsia, birth weight and Apgar score. We performed multivariate analysis, with linear regression coefficients and 95% Confidence Intervals (CI).
Results: Depression was diagnosed in 2.54% pregnant women from a total sample of 17,177. Depression is significantly associated with a miscarriage (OR 1.64), higher risk pregnancy (OR 4.9) and low birth weight (OR 2.2). Pre-eclampsia, 1-minute Apgar score and caesarean section were not significantly associated with depression.
Conclusion: Pregnancies in women with depression were more often classified as high-risk. In addition, depression in the mother increases the probability of miscarriage and low birth weight.
Keywords: Pregnancy; Depression; Preterm birth; Low birth weight
Introduction
Depression is one of the main causes of disability which affects approximately 280 million people globally [1].
Antenatal depression occurs during pregnancy, and can have consequences for both the mother and the newborn. It is estimated that the prevalence in Spain and neighbouring countries is around 10-15% [2-5], and that approximately 1.8-8% of pregnant women with depression use antidepressants [6-8].
Mental health problems impact pregnancy and childbirth and might also correlate with adverse outcomes for the newborn and the baby’s development (HOWAR). One study, correlated depression in pregnant mothers under 35 years of age with hyperemesis, abortion, foetal malposition, caesarean section, and even intrauterine death [9]. Although they do not fully specify pathophysiological mechanisms, Aldane and colleagues concluded that maternal antenatal mental health disorders might be associated with a moderate increase in stillbirth and infant mortality [10].
In a systematic review comparing 20 cohort studies, Jahan, et al. conclude that untreated depression during pregnancy is associated with abortion, prematurity, Low Birth Weight (LBW, birth weight <2500 g), Small for Gestational Age (SGA), complications during delivery and postpartum depression [11].
Low birth weight is a predictor of short and long-term health. During the neonatal period, low birth weight is associated with a higher risk of infection, respiratory distress and mortality [12,13]. Later in life, it is associated with developmental delay, cardiovascular disease, and diabetes [14,15].
The aim of this study is to verify if antenatal depression has any deleterious effect on maternal and neonatal outcomes.
Materials And Methods
Study design and data collection
Retrospective, observational cohort study in pregnant women between 2012-2018 in the health region of Lleida.
Data were obtained from patients who had given birth at the Arnau de Vilanova Hospital between January 1, 2012 and December 31, 2018. The Arnau de Vilanova hospital is the only referral hospital in the region. Data were obtained from the CMBD database (Catalan acronym for minimum data set) in the E-CAP electronic medical records database, and from the Catalan health service database, which contains the electronic prescriptions made by Catalan health service professionals.
This study is part of the ILERPREGNANT project, which aims to analyse the population prevalence of diseases, drug prescription and pharmacological adherence during pregnancy [16].
Participants
Women who had delivered between January 1, 2012 and December 31, 2018. Data from the date of the last period to the date of delivery were included. This means that data from 2011 were included for women with a last period date in 2011 and a delivery date in 2012. Women from health regions other than Lleida were excluded. To evaluate the representativeness of the sample, the percentage of births studied (births registered in the Arnau de Vilanova University Hospital in Lleida) was calculated with respect to the total number of births in the health region of Lleida according to the Statistics Institute of Catalonia (Idescat) (Table 1).
| Year | Deliveries in Lleida sample | Deliveries from Idescat | Sample/Idescat |
|---|---|---|---|
| 2012 | 3635 | 3788 | 96% |
| 2013 | 3370 | 3535 | 95% |
| 2014 | 3308 | 3592 | 92% |
| 2015 | 3162 | 3426 | 92% |
| 2016 | 3180 | 3283 | 97% |
| 2017 | 3034 | 3197 | 95% |
| 2018 | 3001 | 3029 | 99% |
Table 1: Number of births registered in Lleida sample in comparison to the Lleida health region per year
The variables recorded were as follows: Depression (yes/no), which includes a diagnostic for depression according to the International Classification of Diseases, 9th revision (ICD-9) with codes 296.20 to 296.25, 296.30 to 296.35, 300.4, or 311, and in the 10th revision (ICD-10) with codes F32.0 to F32.9, F33.0 to F33.3, F33.8, F33.9, F34.1, or F41.2; age; Body Mass Index (BMI); diabetes mellitus (ICD-10 O24.9); risk of the pregnancy; duration of the pregnancy (miscarriage, preterm, term, prolonged); caesarean section; birth weight (<2500 g=underweight, between 2500 g and 3999 g=normal weight, and ≥ 4000 g=macrosomia), 1-minute and 5-minute Apgar score; and preeclampsia. Data were also collected on prescribed antidepressant drug, dispensation date, dose and amount. Antidepressants were classified into four classes following the Anatomical Therapeutic Chemical (ATC) classification system.
Data analysis
A descriptive analysis was performed, with numerical variables described by mean and standard deviation, and categorical variables by absolute and relative frequencies. To evaluate differences between groups, we used Student's t-test or Chi-square test for numerical and categorical variables, respectively. The association of the different variables with depression was evaluated with a multivariate linear model, using percentage of depression as the response variable, and the rest of the variables as predictors. Regression coefficients and odds rations and their 95% confidence interval were calculated.
Ethics
This study was approved by the Clinical Research Ethics Committee (CREC) of the Institut d’Investigació IDIAP Jordi Gol (code 19/196-P). The study follows the tenets of the Declaration of Helsinki. The information was extracted from centralized medical files in the E-CAP database by the department of research management and health evaluation. Informed consent from participants was not required. The variables in the E-CAP database were de-identified and processed following confidentiality guarantees established by the National Law and Regulation 2016/679 of the European Parliament and of the Council on personal data protection.
Results
Participants
Participants include a sample of 21,375 pregnant women who had given birth at the Arnau de Vilanova Hospital in Lleida between 2012 and 2018 (both included). Women who did not have a health card (n=1625) were excluded. Women with missing data in their medical records were also excluded (n=2573). The final sample consisted of 17,177 patients (Figure 1).
The average age of pregnant women during the study period was 30.5 years. A total of 436 women (2.54%) suffered from depression. In 20 women (0.13%), depression was considered gestational (Tables 2-4).
Figure 1: Sample of pregnant women.
| Year of delivery | 17177 |
|---|---|
| 2011 | 43 (0.25%) |
| 2012 | 2740 (16.0%) |
| 2013 | 2525 (14.7%) |
| 2014 | 2491 (14.5%) |
| 2015 | 2419 (14.1%) |
| 2016 | 2418 (14.1%) |
| 2017 | 2317 (13.5%) |
| 2018 | 2224 (12.9%) |
| Age at pregnancy | 17177 |
| <30 | 6981 (40.6%) |
| >35 | 5733 (33.4%) |
| 30-35 | 4463 (26.0%) |
| Body mass index | 16803 |
| ≤ 25 | 11117 (66.2%) |
| >30 | 1986 (11.8%) |
| 26-30 | 3700 (22.0%) |
| Number of pregnancies | 17177 |
| 1 | 9009 (52.4%) |
| 2 | 5181 (30.2%) |
| 3 | 1870 (10.9%) |
| 4 | 646 (3.76%) |
| >4 | 471 (2.74%) |
| Multiple pregnancy | 17177 |
| No | 17145 (99.8%) |
| Yes | 32 (0.19%) |
| Pre-eclampsia | 17177 |
| No | 17018 (99.1%) |
| Yes | 159 (0.93%) |
| Pregnancy risk | 15333 |
| Very high | 316 (2.06%) |
| High | 2912 (19.0%) |
| Intermediate | 4527 (29.5%) |
| No risk | 7578 (49.4%) |
| Birth weight | 15133 |
| Low birth weight | 910 (6.01%) |
| Macrosomia | 1020 (6.74%) |
| Normal birth weight | 13203 (87.2%) |
| Apgar 1’ | 15085 |
| High | 14706 (97.5%) |
| Low | 379 (2.51%) |
| Apgar 5’ | 15087 |
| High | 14970 (99.2%) |
| Low | 117 (0.78%) |
| Caesarean section | 17177 |
| No | 14201 (82.7%) |
| Yes | 2976 (17.3%) |
Table 2: General characteristics of the sample.
|
|
No (N=16741) |
Yes (N=436) |
|---|---|---|
|
Year of delivery |
||
|
2012 |
2682 (97.9%) |
58 (2.12%) |
|
2013 |
2473 (97.9%) |
52 (2.06%) |
|
2014 |
2430 (97.6%) |
61 (2.45%) |
|
2015 |
2355 (97.4%) |
64 (2.65%) |
|
2016 |
2348 (97.1%) |
70 (2.89%) |
|
2017 |
2243 (96.8%) |
74 (3.19%) |
|
2018 |
2167 (97.4%) |
57 (2.56%) |
Table 3: Depression diagnosis in pregnant women for each study year.
| Depression | No (N=16741) | Yes (N=436) |
|
|---|---|---|---|
| Age at pregnancy (years) | 30.5 | 32.2 |
p <0.001 |
| <30 | 6850 (40.9%) | 131 (30.0%) | |
| >35 | 5558 (33.2%) | 175 (40.1%) | |
| 30-35 | 4333 (25.9%) | 130 (29.8%) | |
| Body mass index | 24.8 (4.91) | 25.6 (5.54) |
p: 0.150 |
| ≤ 25 | 10851 (66.3%) | 266 (62.6%) | |
| >30 | 1924 (11.7%) | 62 (14.6%) | |
| 26-30 | 3603 (22.0%) | 97 (22.8%) | |
| Number of pregnancies | |||
| 1 | 8790 (52.5%) | 219 (50.2%) |
p: 0.413
|
| 2 | 5053 (30.2%) | 128 (29.4%) | |
| 3 | 1815 (10.8%) | 55 (12.6%) | |
| 4 | 629 (3.76%) | 17 (3.90%) | |
| >4 | 454 (2.71%) | 17 (3.90 %) | |
| Multiple pregnancy | |||
| No | 16709 (99.8%) | 436 (100%) |
p: 1,000 |
| Yes | 32 (0.19%) | 0 (0.00%) | |
| Caesarean section | |||
| No | 13854 (97.6%) | 347 (2.44%) |
0.097 |
| Yes | 2887 (97.0%) | 89 (2.99%) | |
| Duration of pregnancy (qualitative) | |||
| Miscarriage | 545 (95.8%) | 24 (4.22%) |
0.004 |
| Post-term | 325 (99.1%) | 3 (0.91%) | |
| Preterm | 743 (96.6%) | 26 (3.38%) | |
| Term | 11024 (97.6%) | 272 (2.41%) | |
| Pre-eclampsia | |||
| No | 16587 (99.1%) | 431 (98.9%) |
p: 0.606 |
| Yes | 154 (0.92%) | 5 (1.15%) | |
| Pregnancy risk | |||
| Very high | 293 (1.96%) | 23 (6.01%) |
p<0.001
|
| High | 2820 (18.9%) | 92 (24.0%) | |
| Intermediate | 4399 (29.4%) | 128 (33.4%) | |
| No risk | 7438 (49.8%) | 140 (36.6%) | |
| Birth weight | |||
| Low birth weight | 866 (5.87%) | 44 (11.8%) |
p<0.001 |
| Macrosomia | 993 (6.73%) | 27 (7.24%) | |
| Normal birth weight | 12901 (87.4%) | 302 (81.0%) | |
| Apgar 1’ | |||
| High | 14347 (97.5%) | 359 (96.2%) |
p: 0.167 |
| Low | 365 (2.48%) | 14 (3.75%) | |
| Apgar 5’ | |||
| High | 14600 (99.2%) | 370 (99.2%) |
p: 0.767 |
| Low | 114 (0.77%) | 3 (0.80%) | |
| Caesarean section | |||
| No | 13854 (82.8%) | 347 (79.6%) |
p: 0.097 |
| Yes | 2887 (17.2%) | 89 (20.4%) |
|
Table 4: Depression prevalence and relationship with other factors.
Table 3 shows percentage of depression for each year of study. The average prevalence of depression was 2.5%. Patients with depression have a higher average age, a higher body mass index, and are more often classified as high-risk pregnancy. The difference in prevalence of low birth weight is statistically significant, with 5.85% in children of patients without depression versus 11.7% of babies born to mothers with depression. No differences were found in relation to pre eclampsia, Apgar score and number of caesarean sections.
Regarding pharmacological treatment, 14.9% of patients with depression received treatment, 71.3% drugs are selective serotonin reuptake inhibitors, followed by 12.1% serotonin-norepinephrine reuptake inhibitors, 7.89% non-selective monoamine oxidase inhibitors, and 6.58% atypical antidepressants. The most commonly prescribed drugs were paroxetine, followed by sertraline, citalopram and escitalopram. All patients diagnosed with depression received pharmacological treatment.
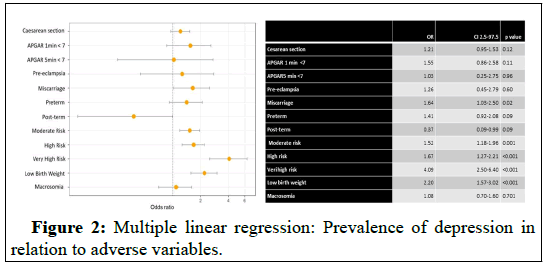
The regression model shows that pregnant women with depression have a significantly higher risk pregnancy, in particular in relation to low birth weight. In contrast, no significant differences were found regarding the 1-minute Apgar score, pre-eclampsia and number of caesarean sections (Figure 2).
Figure 2: Multiple linear regression: Prevalence of depression in relation to adverse variables.
Discussion
This study shows a prevalence of antenatal depression of 2.54%, 14.9% patients taking one or more antidepressant. Pregnancy of women with depression was more frequently classified as very high risk (4.9) and show more risk of miscarriage (1.64). For the new born, low birth weight (OR 2.2) was significantly more common in infant from women with depression (11.8%) compared to infant from women without depression (5.87%).
Results of adverse consequences vary in the studies on antenatal depression. A meta-analysis carried out by Ghimire, et al. found an increased risk of preterm birth (RR=1.35, 95% CI 1.19–1.52), low birth weight (RR=1.86, 95% CI 1.32–2.62) and intrauterine growth retardation (RR=4.39, 95% CI 2.45–7.86) [17,18]. Lang, et al. and Nasren, et al. also reported an increased risk of low birth weight [19,20]. However, other studies have not reported this association. The systematic review and meta-analysis by Fekadu Dadi, et al. attribute the higher prevalence of depression to the economic and psycho-social situation of pregnant women. This psycho-social situation might influence the relationship observed between anxiety/depression and prematurity. Women living in disadvantaged neighbourhoods have less access to quality food and health services, fewer leisure opportunities and more social and financial stress, which might determine the adverse effects on pregnancy.
In a systematic review of 20 studies on untreated antenatal depression published in 2021, Jahan, et al. underscored the relationship with low birth weight, and also with preterm delivery, death of the newborn (in addition to other perinatal complications), and postpartum depression.
Other studies point at the causative effect of antidepressant treatment rather than depression on birth weight. Specifically, in 2016 Nezvalová-Henriksen, et al. studied the effect of exposure to SSRIs during the 2nd and 3rd trimester pregnancy, concluding that it was associated with an average decrease of 4.9 days of pregnancy and of 205 g of birth weight.
In 2017, Mitchell, et al. conducted a systematic review to compare women who had taken antidepressants during their pregnancy with women diagnosed with depression and not treated. Regarding the average weight of the newborn, 6 of 9 studies did not find significant differences, two observed a higher risk of small for gestational age due to antidepressant treatment, and one study concluded that untreated depression was a risk factor for low birth weight. Only one study analysed abortion, and it was inconclusive. Another study found that children born to mothers who adhered to antidepressants weighed 71.9 g less than children of mothers who discontinued treatment (95% Confidence Interval (CI): −115.5, −28.3 g), with a larger difference for girls (−106.4 g, 95% CI: -164.6, −48.1) than boys (−48.5 g, 95% CI: −107.2, 10.3).
Among the limitations, we should consider that in this study, 14.9% patients diagnosed with depression receive antidepressant treatment. Therefore, we have not analysed the influence of the treatment on the outcomes of the study or the adherence to it, which may condition different results. Importantly, this study has not stratified by socio-demographic variables that might affect pregnancy, but it is a population study conducted with data from a referral hospital that covers a high percentage of the population.
Conclusion
Antenatal depression is a risk factor for infant morbidity and mortality. In this study, maternal depression was associated with an increased risk of low birth weight, miscarriage and categorization of risk pregnancy. We underscore the relevance of early detection and treatment of depression in pregnancy. Further research is needed to evaluate the impact of depression on mother and child, taking into account severity, antidepressant treatment and other associated factors, in order to improve the management of pregnant women with depression.
Acknowledgements
The authors would like to thank Dr. Miquel Buti for his valuable contribution and help in the design and creation of the database, and Laura Azlor for her contribution in the statistical analysis. All authors have read and approved the final version of the manuscript.
Author Contributions
All authors (M.O., M.L., J.S., D.P., M.C.S. and B.S.R.) contributed to the study conception and design. Material preparation, data collection and analysis were performed by M.O., M.L., J.S., D.P. and M.C.S. The first draft of the manuscript was written by B.S.R., M.L. and M.O.; and all authors commented on previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
There was no funding to carry out this study. This research didn’t receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
This study was approved by the ethics and clinical research committee of the “Institute for Primary Health Care Research Jordi Gol i Gurina (IDIAPJGol)” under the code 19/196-P. The study was conducted in accordance with the principles of the Declaration of Helsinki. Pseudonymized retrospective descriptive cross-sectional study adheres to Additional Provision 17.2.d LOPD-GDD for research purposes, without the need to obtain the consent of the data holders. There is a technical and functional separation between the research team and the performer pseudonymization, the data is only accessible to the research team, and technical measures have been taken to prevent such re-identification and access by third parties through the CMBD database (“Conjunt Minim de Base de Dades”), the E-CAP computerized medical history database and the Catalan Health Service database.
Data Availability Statement
Available upon request to corresponding author (dperejon.lleida.ics@gencat.cat).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Institute of Health Metrics and Evaluation (2021). Global health data exchange (GHDx).
- Pereira PK, Lovisi GM, Lima LA, Legay LF, de Cintra Santos JF, et al. (2011) Depression during pregnancy: review of epidemiological and clinical aspects in developed and developing countries. Psychiatr Disord Trends Dev 10: 267-290.
- Howard LM, Khalifeh H (2020) Perinatal mental health: a review of progress and challenges. World Psychiatry 19: 313-327.
[Crossref] [Google Scholar] [PubMed]
- Marcos-Najera R, Rodriguez-Munoz MF, Lara MA, Navarrete L, Le HN (2021) A Cross-Cultural Analysis of the Prevalence and Risk Factors for Prenatal Depression in Spain and Mexico. Cult Med Psychiatry 45: 599–612.
[Crossref] [Google Scholar] [PubMed]
- Rodriguez-Munoz M, Le HN, de la Cruz IV, Crespo MEO, Mendez NI (2017) Feasibility of screening and prevalence of prenatal depression in an obstetric setting in Spain. Eur J Obstet Gynecol Reprod Biol 215: 101–105.
[Crossref] [Google Scholar] [PubMed]
- Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG (2017) A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord 219: 86-92.
[Crossref] [Google Scholar] [PubMed]
- Benard‐Laribiere A, Pambrun E, Sutter‐Dallay AL, Gautier S, Hurault‐Delarue C, et al. (2018) Patterns of antidepressant use during pregnancy: a nationwide population‐based cohort study. Br J Clin Pharmacol 84: 1764-1775.
[Crossref] [Google Scholar] [PubMed]
- Zoega H, Kieler H, Norgaard M, Furu K, Valdimarsdottir U, et al. (2015) Use of SSRI and SNRI antidepressants during pregnancy: a population-based study from Denmark, Iceland, Norway and Sweden. PloS One 10: e0144474.
[Crossref] [Google Scholar] [PubMed]
- Huang HC, Sung FC, Chen PC, Chang CY, Muo CH, et al. (2017) Obstetric outcomes in pregnant women with and without depression: population-based comparison. Sci Rep 7: 13937.
[Crossref] [Google Scholar] [PubMed]
- Adane AA, Bailey HD, Morgan VA, Galbally M, Farrant BM, et al. (2021) The impact of maternal prenatal mental health disorders on stillbirth and infant mortality: a systematic review and meta-analysis. Arch Womens Ment Health 24: 543-555.
[Crossref] [Google Scholar] [PubMed]
- Jahan N, Went TR, Sultan W, Sapkota A, Khurshid H, et al. (2021) Qureshi IA, Alfonso M. Untreated depression during pregnancy and its effect on pregnancy outcomes: a systematic review. Cureus 13: e17251.
[Crossref] [Google Scholar] [PubMed]
- Conley D, Strully KW, Bennett NG (2003) The Starting Gate: Birth Weight and Life Chances. Berkeley, CA: University of California Press.
- Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, et al. (2002) Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 110: 285-291.
[Crossref] [Google Scholar] [PubMed]
- Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, et al. (2000) Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics 105: 1216-1226.
[Crossref] [Google Scholar] [PubMed]
- Alexander BT, Dasinger JH, Intapad S (2014) Effect of low birth weight on women’s health. Clin Ther 36: 1913-1923.
[Crossref] [Google Scholar] [PubMed]
- Siscart J, Oros M, Serna MC, Perejon D, Galvan L, et al. (2022) Adherence to treatment for hypothyroidism in pregnancy and relationship with thyrotropin control: a retrospective observational cohort study. BMC Pregnancy Childbirth 22: 168.
[Crossref] [Google Scholar] [PubMed]
- Ghimire U, Papabathini SS, Kawuki J, Obore N, Musa TH (2021) Depression during pregnancy and the risk of low birth weight, preterm birth and intrauterine growth restriction-an updated meta-analysis. Early Human Development 152: 105243.
[Crossref] [Google Scholar] [PubMed]
- Fekadu Dadi A, Miller ER, Mwanri L (2020) Antenatal depression and its association with adverse birth outcomes in low and middle-income countries: A systematic review and meta-analysis. PloS One 15: e0227323.
[Crossref] [Google Scholar] [PubMed]
- Lang J, Zhang B, Meng Y, Du Y, Cui L, et al. (2019) First trimester depression and/or anxiety disorders increase the risk of low birthweight in IVF offspring: a prospective cohort study. Reprod Biomed Online 39: 947-954.
[Crossref] [Google Scholar] [PubMed]
- Nasreen HE, Pasi HB, Rifin SM, Aris MA, Ab Rahman J, et al. (2019) Impact of maternal antepartum depressive and anxiety symptoms on birth outcomes and mode of delivery: a prospective cohort study in east and west coasts of Malaysia. BMC Pregnancy Childbirth 19: 201.
[Crossref] [Google Scholar] [PubMed]
Citation: Lopez DP, Serna LG, Arnaiz MCS, Ruiz MO, Viladegut JS, et al. (2025) Antenatal Depression and Risk of Complications in the Mother and the Newborn. A Retrospective Cohort Study. J Preg Child Health 11: 680.
Copyright: © 2025 Lopez DP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 466
- [From(publication date): 0-0 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 239
- PDF downloads: 227