Application of Using a Wearable Strain Sensor on Respiratory Evaluation in Physiotherapy-Changing with Aging in Breathing Pattern
Received: 10-Aug-2018 / Accepted Date: 20-Aug-2018 / Published Date: 21-Aug-2018 DOI: 10.4172/2165-7025.1000396
Keywords: Breathing pattern; Aging; Wearable strain sensor
Introduction
The year 2000 witnessed a turning point when China’s population started to be aging. In 2014 statistics showed that the elderly above 65 in China amounted to 138 million, that was 10.1% of the total population of the country. By 2020, the percentage would rise to 12.8% [1]. In the near future, some of the appeared “disease” state of an aged person may be regarded as a “normal” physiological state in clinic. Therefore, to redefine a clear-cut line between the two states is vitally important. When people get old, their respiratory system would change accordingly. Such structural changes as the chest wall and thoracic spine deformities are most apparent and the variations in the physiological structural indexes are also obvious. That is why it is not easy to redefine the criteria to distinguish between the “disease” state and “normal” state [2].
As the matter of fact, the respiratory muscle strength, chest expansion compliance, and lung functions of aged persons would all be degraded, thus their respiratory system functions would become weakening and their work of breathing rising, clearance of airway secretion narrowing and effective cough reducing. These changes can to some degree interpret some clinical manifestation and aberrant diagnostic cases of aged persons [3].
One’s breathing movement is concerned with the rib cage of the chest and the abdomen wall [2]. The chest compliance depends on the elastic load when breathing in. When a person gets aged, his or her chest wall compliance would reduce and aging-related problems such as osteoporosis, stiff calcification of the rib cage, and kyphosis would occur [3]. The most important respiratory muscle is diaphragm, which can drive the movement of the abdomen wall. The diaphragmatic muscle would atrophy, and all other muscle strength would reduce, thus causing lager residual volume, when people become old [4]. Briefly speaking, how to measure and evaluate the breathing pattern changes with aging in timely and effective methods is crucial.
Though some sophisticated instruments such as inductive or optoelectronic plethysmography, computed tomography or video systems have been applied in clinical assessment for breathing movement [5,6] these instruments are not available for general clinical studies because of their extremely-high cost. Therefore some new devices with low cost have been developed, such as the respiratory movement instrument (RMMI), breathing movement measuring device (BMMD) and 3D motion analysis system etc. [5-8], but these devices need a special experimental environment or need to be installed in a complex setting.
A simple and practical method with a measuring tape to assess the mobility of the chest-abdomen wall is developed [5,8,9] but this method is only suitable for the studies only with a limited sample size instead of those with a large sample size and those wanting repeated measurements, because in such a case, the measurement results would be affected due to the fatigue of those testers.
Therefore, the WSS has been newly developed to meet the special purpose of the study clarifying the changes of breathing pattern of aged people and ascertaining differences of the chest-abdomen movement of different age group, i.e. young people, middle-age people, and senior people. The study proves our hypothesis that human breathing pattern would change with aging.
Participants and Methods
This study was conducted at Physical Therapy Department, China Rehabilitation Research Center. Twenty-three students from The Capital Medical University served as the youth group, thirty staff from the PT Department of the research center as the middle-aged group, and twenty-nine senior citizens from the nearby Jiao Men residential community as the aged group, altogether eighty-two participants, all being healthy male, had been recruited to take part in the study. The physical criteria for selecting the participants were that they should have no history of respiratory, circulatory or neurological disorders.
All participants were informed to sign an agreement in their own will before taking part in the study. The Ethic Committees of International University of Health and Welfare (No.16-Io-177, and 238) and China Rehabilitation Research Center (CRRC-IEC-RFSC- 005-01) had jointly approved the study protocol.
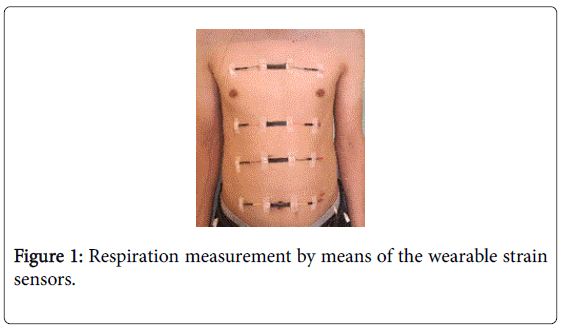
For conducting this study, a wearable strain sensor device (WSS) was used to detect the chest-abdominal breathing pattern and movements. It consists of four 3.5-cm-long sensors, which are connected with each other in parallel. The four sensors were stuck to the chest-abdomen wall of a participant with medical adhesive. The output signals detected by the sensors were sent to a circuit board that is also stuck to the chest-abdomen wall, which then send the signals to a smartphone via the blue-tooth [10]. The data thus produced were processed by application software (MATLAB Version 7.11.0.584 (R2010b), License Number: 161051). The appropriate strain ranges of the sensors were thus calculated by spreadsheet software (Microsoft Excel, USA) [11].
All of the four sensors were stuck to four spots of the chestabdomen wall, that is, the axilla, xiphoid process, the 10th rib and umbilicus of each of the participants in three groups, so as to monitor the chest-abdominal breathing pattern and its movements. During the process, the participants should be in standing position, with shirts off and pants loosen, and not move their torsos and shoulders as shown in Figure 1. The participants should breathe in and out to the maximum. The WSS device would record the maximum movement range of the deep chest-abdominal breathing.
The data of the breathing movement of each cycle were detected by the four sensors for five times and the average value of the five-time data of each sensor was calculated. It is required to have a break between the first and the second movement for all the participants in three groups to get a little rest, allowing each subject to feel fine and removing fatigue effects, to guarantee the quality of the second test.
The characteristics of all participants were described as means ± SD (standard deviation). The data to be studied include breathing movement values of the axilla, xiphoid process, the 10th rib and umbilicus on chest-abdomen wall, which were examined by the Twoway ANOVA so as to compare the four values detected by the WSS among different groups, the Bonferroni correction was done as a posthoc test to ascertain significant differences. All data were analyzed using the IBM SPSS statistics software version 24.0 for Windows, and the values of less than 0.05 were statistically significant level.
Results
The baseline characteristics of anthropometry of all participants were shown in Table 1. The raw data detected at the axilla, xiphoid process, the 10th rib and umbilicus respectively by the WSS were presented in Table 2 as the measurement of the breathing movement of the three groups. The result of the data analysis shows that all had significant differences at four spots between the senior group and the youth group (p<0.05); there are significant differences at the axilla, xiphoid process and the 10th rib (p<0.05) except the umbilicus between senior group and the middle-aged group (p>0.05); there are significant differences at the axilla, xiphoid process, 10th rib and the umbilicus between the middle-aged group and the youth group (p<0.05). Next the Bonferroni test as a post hoc analysis showed that F (2,79)=4.382 (p<0.05), i.e. the expansion range at the axilla, xiphoid process, and the 10th rib of the senior group was obviously smaller than the youth group and the middle-aged group, but the expansion range at the umbilicus had no much difference from the middle-aged group.
| Youth group (n=23) | Middle-age group (n=30) | Senior group (n=29) | |
|---|---|---|---|
| Age (yrs) | 24.0 ± 2.7 | 40.1 ± 4.3 | 75.5 ± 8.2 |
| Height (cm) | 173.8 ± 3.9 | 173.6 ± 3.6 | 169.9 ± 5.5 |
| Weight (kg) | 67.6 ± 7.5 | 77.0 ± 17.5 | 68.0 ± 11.1 |
| BMI (kg/m2) | 22.4 ± 2.6 | 26.3 ± 3.7 | 23.7 ± 3.8 |
All values were shown as mean ± SD (standard deviation).
BMI: Body Mass Index.
Table 1: The characteristics of all male participants in this study (Mean ± SD).
| Youth group | Middle-aged group | Senior group | p-value | |
|---|---|---|---|---|
| Axilla (cm) | 0.33 ± 0.20 | 0.31 ± 0.04 | 0.23 ± 0.02 | *1, *2 |
| Xiphoid process (cm) | 0.36 ± 0.20 | 0.33 ± 0.05 | 0.26± 0.02 | *1, *2 |
| 10th rib (cm) | 0.48 ± 0.24 | 0.43 ± 0.07 | 0.39 ± 0.06 | *1, *2 |
| Umbilicus (cm) | 0.42 ± 0.22 | 0.38 ± 0.05 | 0.39 ± 0.06 | *1, *3 |
WSS: wearable strain sensor
*1. p<0.05 Between youth group and senior group
*2. p<0.05 Between middle-aged group and senior group
*3. p>0.05 Between middle-aged group and senior group
Table 2: The raw data (Mean ± SD) of the WSS among three groups for measuring breathing movement at the four torso spots.
Discussion
The study finds that the respiratory function changes with aging remarkably. Aging would cause a decrease in the range of the chest and abdomen expansion, the scientific evidence of which is the difference of the breathing movement among youth, middle-aged, and senior group. Moreover, it is very essential that breathing pattern has been changed by aging.
This study also find that the maximum expansion range of the chest and abdomen in youth group is most noticeable among all three groups in terms of the chest-abdominal breathing pattern, and the expansion range of the chest wall is obviously smaller than the other two groups. For the in middle-aged and senior group, the expansion of the chest wall is smaller than that of the abdomen wall. This can be explained by the following two aspects: 1) due to the anatomical changes. There would be a reduction with aging in supporting tissue of the rib cage, which would result in premature closure of the small airway during normal breathing [12-14] or smaller chest wall expansion; 2) due to the morphological changes. The expansion of the chest wall would be affected by the capacity of thorax, which depends on the mobility of the skeletal muscles, the elasticity of surrounding soft tissues, and respiratory muscles intensity [15-17]. Therefore, the chest wall expansion would diminish with aging. Owing to diaphragmatic strength decrease with aging [2,18,19] the expansion ranges of the 10th rib on the abdomen wall of the senior group would become smaller than that of the middle-aged group. Only thing on the contrary is that the expansion range at umbilicus of the middle-aged group would become smaller than that of the senior group. And there was another explanation; breathing expansion reduction on abdomen wall would have more irregular breathing rhythm in the elderly [20], apart from external changes. In general, the five breathing movements from the maximal end of inspiration to the maximal end of expiration in this study were unable to be conducted at the same breathing rhythm.
In this study the WSS was used when measuring expansion of the chest wall and abdomen in clinical practice for detecting the changes in thoracoabdominal compliance. In fact, in the case of similar lung compliance, the chest wall expansion was lower for some of aged people [2], so it is difficult to discriminate the differential diagnosis if only the routine spirometer or other similar instruments are used in clinical practice. Therefore, the WSS with high sensitivity and accuracy was developed for measuring the expansion of the chest and abdomen wall of the aged people, which does not need special environment nor to be installed in sophisticated settings [21]. In addition, the WSS with lower cost is affordable for ordinary aged people, so WSS are used to monitor their respiratory conditions and expansion of chest-abdomen at home. The aged people usually have reduced respiratory space, weakened ventilator tissue that causes hypoxia and hypercapnia. All these could induce ventilator failure (if, heart failure, pneumonia, etc.) [2]. So compared to young people, the aged people have lower respiratory capability and should be paid more attention to their respiratory function [2]. Traditionally, breathing exercise in physical therapy was usually assessed only by observation or palpation of the experienced therapists during the physical examination, while now the WSS can replace the physical examination as an objective tool for measuring the respiratory movement in clinical practice [21]. Moreover, the clinical measurement done by the WSS is an effective approach for monitoring lung function, thus being able to reduce the probability of delay in medical treatment. Compared with our previous versions, the data collection terminal of the WSS was replaced by a smartphone as a technological innovation. However there are still some limitations in this study. First, the participants in the middleaged group were on the younger side, which resulted in the similar respiratory conditions with the youth group; secondly, BMI indexes of the middle-aged group and the senior group were on the higher side and some people in the two groups had abdominal distension, which more or less interfered with their breathing movement; thirdly, when the respiratory signals were collected by a smartphone via blue-tooth, the data transmission would be disturbed or sometimes even be interrupted by some unidentified external factors; fourthly, if there exists some perspiration on the skin of the detected spot, the sensitivity of the strain sensors would be affected during the respiratory data detecting process.
Chinese populations are increasingly aging. Our further studies in the near future would include the evaluation of the age-related changes of the respiratory system and providing scientific and valuable evidence for the clinical medical practice. The expansion ranges of the respiratory movement at the axilla, xiphoid process, and the 10th rib except the umbilicus detected by the WSS device were obviously weakened for the aged people. Thus, breathing pattern of the aged people would change. In conclusion, the results of this study also prove our initial hypothesis that people’s breathing pattern would gradually change with aging during their entire life span. Therefore, it is essential to call external medical attention and intervention.
Conflicts of Interest
There are no any conflicts of interest.
Funding
No financial contributions received.
References
- China Industry Information Network research on the market depth of China’s old-age industry and a report of its investment prospects (2015).
- Gulshan S, James G (2006) Effect of aging on respiratory system physiology and immunology. Clin Interv Aging 3: 253-260.
- Mittman C, Edelman NH, Norris AH, Shock NW (1965) Relationship between chest wall and pulmonary compliance and age. Journal of Applied Physiology 20: 1211-1216.
- McClaran SR, Babcock MA, Pagelow DF, Reddan WG, Dempsey JA (1995) Longitudinal effects of aging on lung function at rest and exercise in healthy active fit elderly adults. J Appl Physiol 78: 1957-1968.
- Fiamma MN, Samara Z, Baconnier P, Similowski T, Straus C (2007) Respiratory inductive plethysmography to assess respiratory variability and complexity in humans. Respir Physiol Neurobiol 156: 234-239.
- Ferringo G, Pedotti A (1985) A dedicated hardware system for movement analysis via real-time TV signal processing. IEEE Trans Biomed Eng 32: 943-950.
- Fagevik M, Romberg K (2010) Reliability of the respiratory movement measuring instrument, RMMI. Clin Physiol Funct Imag 30: 349-353.
- Shobo A, Kakizaki K (2015) Effects of two sitting positions on chest volume. Rignku ryohougaku 30: 499-502.
- Fregonezi G, Resqueti V, Guell R, Pradas J, Casan P (2005) Effects of 8-week, interval-based inspiratory muscle training and breathing re-training in patients with generalized myasthenia gravis. Chest 128: 1524-1530.
- Wei H, Chen S, Zhou B, Li Q, Wang R, et al. (2016) Highly sensitive and transparent strain sensor based on thin elastomer film. Electron Device Letters 37: 667-670.
- Wang C, Li X, Gao E, Jian M, Xia K, et al. (2016) Carbonized silk fabric for ultrastretchable, highly sensitive, and wearable strain sensors. Adv Mater 28: 6640-6648.
- Gila B (2000) Breathing pattern in humans: diversity and individuality. Respiration Physiology 122: 123-129.
- Gillooly M, Lamb D (1993) Airspace size in lungs of lifelong non-smokers; effect of age and sex. Thorax 48: 39-43.
- Knudson RJ (1981) How aging affects the normal lung. J Respir Dis 2: 74-84.
- Janssens JP, Pache JC, Nicod LP (1999) Physiological changes in respiratory function associated with aging. Eur Respir J 13: 197-205.
- Zeleznik J (2003) Normative aging of the respiratory system. Clin Geriatr Med 19: 1-18.
- Peterson DD, Pack AI, Silage DA, Fishman AP (1981) Effects of aging on ventilatory and occlusion pressure responses to hypoxia and hypercapnia. Am Rev Respir Dis 124: 387-391.
- Tolep K, Higgins N, Muza S, Criner G, Kelsen SG (1995) Comparison of diaphragm strength between healthy adult elderly and young men. Am J Respir Crit Care Med 152: 677-682.
- Polkey MI, Harris ML, Hughes PD, Hamnegärd CH, Lyons D, et al. (1997) The contractile properties of the elderly human diaphragm. Am J Respir Crit Care Med 155: 1560-1564.
- Tobin MJ, Chadha TS, Jenouri G, Birch SJ, Gazeroglu HB, et al. (1983) Breathing patterns. 1 Normal subjects. Chest 84: 202-205.
- Haijuan L, Shaopeng G, Kaipei Z, Guo X, Kuramoto-Ahuja T, et al. (2017) Reliability and validity of measuring respiration movement using a wearable strain sensor in healthy subjects. J Phys Ther Sci 29: 1543-1547.
Citation: Liu HJ, Shaopeng G, Chen S, Kuramoto-Ahuja T, Sato T, et al. (2018) Application of Using a Wearable Strain Sensor on Respiratory Evaluation in Physiotherapy-Changing with Aging in Breathing Pattern. J Nov Physiother 8: 396. DOI: 10.4172/2165-7025.1000396
Copyright: © 2018 Liu HJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4018
- [From(publication date): 0-2018 - Nov 06, 2025]
- Breakdown by view type
- HTML page views: 3114
- PDF downloads: 904