Assessment of Knowledge, Attitude and Practice Towards Colostrum Feeding Among Antenatal Care Attendant Pregnant Mothers in Mizan Tepi University Teaching Hospital, Bench Maji Zone, SNNPR, South West Ethiopia, 2016/2017 G.C
Received: 04-Aug-2017 / Accepted Date: 21-Sep-2017 / Published Date: 26-Sep-2017 DOI: 10.4172/2376-127X.1000348
Abstract
Background: United Nation children’s fund and world health organization recommend colostrums as newborns perfect food that should be initiated within the first hour after birth. Breastfeeding is a common practice in Ethiopia, importance of colostrums feeding is still poorly understood. Objective: To assess knowledge, attitude and practice towards colostrums feeding among ANC attendant pregnant mothers in MTUTH, Bench-Maji, SNNPR and South West Ethiopia 2016/2017. Methods: The data was collected by using semi-structured questionnaire which contain variables as well as both open and close-ended questions in face to face interview for a total of 207 women who follow ANC were included in the study. Results: This study showed that 65.2% of mothers had information about colostrums feeding during pregnancy from various source. 138 (66.66%) of mothers have knowledge about advantage of colostrums feeding. Most mothers had positive attitude (69.4%) about colostrums feeding and 72.46% agreed that colostrums is good milk for body growth and mental development for newborn. Conclusion and recommendation: Many women had good knowledge, positive attitude and practice about colostrums feeding but the data still indicates further effort are required to improve knowledge, attitude and practice of colostrums feeding. so, there should be clear policy guideline to promote colostrums feeding as well as EBF. Its practicability should monitor by concerning body.
Keywords: Attitude; Knowledge; Practice; Colostrum; Antenatal; Ethiopia
Background
Colostrums is the first milk produced by the mammary glands of mammals in late pregnancy just prior to giving birth and continuing through the early days of breastfeeding [1]. This special milk is yellow to orange in color and thick and sticky. It is very rich in proteins, carbohydrates, vitamin A and sodium chloride, but contains lower amounts of lipids, fat and potassium than normal milk [2]. Newborns have premature digestive system which suits the low-volume concentrated form of nutrient supply system of colostrums. The laxative effect of colostrums encourages passage of baby’s first stool, meconium. This helps to clear excess bilirubin which is produced in large quantities at birth and helps prevent jaundice [3]. It contains various immunoglobulin’s like IgA (reactive to Escherichia coli virulence associated proteins) IgG and IgM [4,5]. Other immune components of colostrums are lactoferrin, lysozyme, lacto peroxides, complement and praline-rich peptide (PRP). It also contains various cytokines and growth factors. PRP helps fight against various viral infections like herpes viruses and HIV, bacterial and viral infections which are difficult to treat, various cancer, asthma, allergies and autoimmune diseases. It helps to reduce one of the leading causes of death in our country like diarrhea [6]. Breast feeding should be initiated within the first half an hour after birth. The first milk is the most suitable food for the newborn. It is the thick and yellow colored, the Shasta’s call it “peeyusha” (equal to amrita, the ‘liquor of life’) and western science uses the word “COLOSTRUM”. For most of the children breastfeeding makes the difference between life and death and it is the infants “PASSPORT TO LIFE”. It can be also considered as the first vaccine which needs a “warm chain” made by mother-infant contact. It is secreted in very less amount (30-100 ml), so the mothers need to be explained that this small amount of colostrums is adequate for infant and must not be denied [7]. Colostrums is universally acknowledged as the perfect first food for infants. A review of the custom of expressing antenatal by all women is followed by the maternal and infant medical reasons for expressing and storing colostrums. A suggested regime for expressing and storing of colostrums during pregnancy is included with advice about skin-to-skin contact in the first 24 h to maximize breast milk output in the long term [8].
Statement of the Problem
Globally, it estimated that every day, as many as 4,000 infants and young children die worldwide because they do not get colostrums within the first hour after birth. Many of the world’s infants are given liquids other than mother’s milk in the first few days after birth [9]. Mother and children constitute one fourth of the total national population. They are the most vulnerable group to ill health.
One of the main causes of neonatal mortality and morbidity is inadequate breastfeeding, following faulty breastfeeding technique, ignorance of mother regarding feeding practices, lack of health education given by the health care providers [7]. Many cultural belief and practices all prevalent in postpartum period that some mothers may not feed the baby immediately after birth. They neglect “COLOSTRUM” instead of it they will give sugar water, plain water, honey, etc., all these practices lead to suppression of lactation as prolactin gradually ceases and the breast stops secreting milk [9,10].
Women are recognized as the “keepers of the culture” or the main people who transmit costumes to the next generation. Chief among these costumes is the method for feeding newborns. The rate of breastfeeding varies in communities from almost 70% to a low of 13% as this is culturally influenced [11]. If a woman comes from a family where no one has ever breastfed, she may be very interested in being a “pioneer” in her family. On the other hand, she may be more interested in following her family’s tradition of formula feeding. How soon woman wants to begin breastfeeding after birth is also culturally determined. Although it is the usual practice in hospitals to begin immediately after birth. So initiation of breast feeding while colostrum is still being produced is thought to decrease infant mortality, especially in non-industrialized populations, by the risk of gastroenteritis, diarrheal diseases, respiratory infections, ear infections and influenza [12,13]. So the nursing professionals should motivate the community peoples towards colostrum feeding practice [10].
Some mothers in developing countries avoid colostrum feeding on the basis of traditional or cultural beliefs that range from viewing it as having no nutritional value, seeing it as harmful to the infant’s health (making the baby sick or even causing death) or seeing it as ‘bad luck’ for the family [14-17]. Some women may specify no reason for avoiding colostrum other than tradition [18,19].
Ethiopia has one of the highest infant mortality rates in the world and inappropriate neonatal feeding is a primary factor [20- 26]. Although breast-feeding is almost universal across Ethiopian ethnic groups and geographical areas, it does not always meet WHO/ UNICEF recommendations [27-32]. Data from the 2005 Ethiopian Demographic and Health Survey show that this is true for groups living in the Amhara region that includes the village that was the subject of the present study [33]. Among all births in Ethiopia’s eleven major regions between 2001 and 2005, Amhara mothers had the second lowest percentage of breast-feeding in the first hour after birth (62.6%) and breast-feeding within one day of birth. Less than half of Amhara infants (44.8%) received colostrum, placing it the fourth lowest among eleven regions. A recent study compared breast-feeding practices in the Gondar province (an urban Amhara town) with those in the northern most province of Tigray [34]. New mothers in Tigray were almost twice as likely as mothers in Gondar to initiate breastfeeding within the first hour of birth (Tigray 59% and Gondar 34.2%). A recent UNICEF press release on Ethiopian breastfeeding notes, ‘Often, infants are not fed with colostrum as it is considered unclean’ [31].
The Ethiopian linkages breast-feeding educational programme reports that mothers ‘often discard colostrum’s [35]. A report from the Amhara region quotes a traditional birth attendant who describes her former belief that breast milk should not be used until the placenta is passed, which could take as long as 3 day in difficult births [36]. Before the programme, the birth attendant endorsed the belief that the ‘first milk’ was ‘bad’ for the baby. Amhara mothers interviewed by Almedom noted a positive correlation between valuing colostrum and early breast-feeding initiation and reported a delay in breast-feeding ‘when colostrum was considered ‘‘heavy’’ [37]. He also reported prelacteal feeding for all ethnic groups represented (Gurage, Oromo, Amhara, Sidama, Wolaita and Dorze) with one exception (Tigray) [37].
The fact that only a few mothers deliver in Ethiopia hospital means that the majority deliver from their homes often with the help of unskilled birth attendants. These newborns are often subjected to colostrums avoidance and unhygienic delivery practices arising from traditional beliefs that put their survival at risk in mizan-teferi and Ethiopia Country in general [38].
The 2011 EDHS collected data on the types of foods given on the day and night preceding the survey to the youngest child under age 2 living with the mothers. In Ethiopia, among breastfeeding children under age two, very few (2%) consume infant formula. However, a much higher proportion (18%) receives other milk or other liquids [39]. The introduction of other liquids, such as water, juice and formula, takes place earlier than the recommended introduction at age six months. Among the youngest breastfeeding children (0-1 month), 6% consume other milk and 3% consume other liquids. Consumption of other milk increases gradually with age until age 6-8 months, when 24% of breastfeeding children consume milk. Consumption of other liquids also shows increasing trends with age through age 12-17 months, when 26% of breastfeeding children consume other liquids [40].
Significance of Study
The study is significant because, it is anticipated to identify the gaps on colostrums feeding and recommend ways of bridging on the identified gaps to improve neonatal survival. Also this study will help to know the concept of colostrums among general population [41-44]. It also decrease poor interaction of health personnel with the pregnant women for promoting and supporting colostrums is still unsatisfactory as only few percentages of women received antenatal advice regarding colostrums feeding. Huge gaps may exist in colostrums feeding behaviors, mostly due to lack of awareness.
So, it helps the community to create awareness about the importance of colostrums feeding and advice mothers to practice it in every delivery. Appreciate and initiate Counseling methods to reinforce specific, priority messages by health facility staff and community-based workers at all contact points with pregnant women. It also provides base line information for further study [45-48]. The study about colostrums was not conducted in bench Maji zone southern Ethiopia. So, this study therefore will explore the knowledge, attitude and practice that influence colostrums feeding among mothers in Mizan town.
Objectives
General objective
To assess knowledge, attitude and practice towards colostrums feeding among ANC attendant pregnant mothers in MTUTH, Benchi- Maji Zone, SNNPR, South West Ethiopia, 2017.
Specific objective
1. To identify the knowledge towards colostrums feeding among ANC attendant pregnant mothers.
2. To determine the attitude towards colostrums feeding among ANC attendant pregnant mothers.
3. To determine the practice of colostrums feeding among ANC attendant pregnant mothers.
Study Area
Mizan Aman town is located in SNNP regional state and 568 Km from Addis Ababa capital city of Ethiopia and 839 Km from its regional state Hawassa. Mizan teferi has a latitude and longitude of 7°0’N 35°35’E/7.000°N 35.583°E with an altitude of 1451 m above sea level [49]. Administratively, the town is structured in to five Keble’s (smallest administrative units) and two sub cities. The Town is bordered by Republic of Kenya in the south, the Republic of south Sudan in the southwest, the western Gambella region and Oromiya region in the northeastern Ethiopia. Mizan town is the administrative and trading center of Bench-Maji zone. The average annual rainfall of the town is 1290 mm/year and the temperature of the town ranges between 14°C and 30.5°C. There are one governmental health centers and one hospital in the town. The hospital is under governmental health institution and it provides various services with its departments of Surgery, Gynecology, Pediatrics, Obstetrics, Emergency services, Laboratory, Pharmacy, ART clinic, ANC and EPI. It is also a location of three higher education institutions, Aman Health Science College, Aman Polytechnic College and Mizan Tepi University [50].
Study Design and Period
Institutional based cross-sectional study was used to assess the KAP of colostrum feeding among ANC attendant pregnant mothers, which was conducted between April 10-30 in MTUTH, Mizan Aman town, Ethiopia.
Population
Source population
The source population was all pregnant mothers who have been attending ANC clinic in MTUTH.
Study population
The study population was selected pregnant mothers who was attending ANC clinic during data collection period in MTUTH.
Inclusion and Exclusion Criteria
Inclusion criteria
• All pregnant mothers who have ANC follow up in MTUTH antenatal clinic.
Exclusion criteria
• Mothers who are primigravida.
• Those unable to speak or/and hear.
• Pregnant mother who will be appointed for second visit within data collection period after interview of those mothers.
Sample Size Determination
The sample size (n) required for the study was calculated using the formula to estimate a single population proportion by considering the following assumptions.
Zα/2=critical value for normal distribution at 95% confidence level which equals to 1.96 (Z value at alpha=0.05).
P=(58%) According to study conducted in Raya Kobo district of Amahara region, 2014. d=margin of error of 0.05 with 95% confidence level.
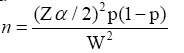
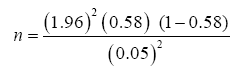
n=374 Individuals
Since the source population is less than 10.000, an adjustment formula (FPC), nf=n/1+n/N is used, where, N=Source population-all estimated pregnant mothers.
nf=Required Sample Size, n=calculated sample size. Hence, the sample size was calculated at total of source population N=378 and n=374 and nf=188. Non-response rate of 10% is 18.8, so the total sample size was 207 pregnant mothers.
Sampling Technique
Simple random sampling technique was employed to draw ANC mothers who are going to be included in the study and direct interview technique using prepared questionnaire during exit from ANC was used. The average number ANC per day was 21 and the service were given in all working days.
Study Variables
• Knowledge of colostrums feeding.
• Attitude of colostrums feeding.
• Practice of colostrums feeding.
Obstetric and medical variables
• Mode of delivery
• Birth order
• Parity
• Birth interval
Maternal sociodemographic variable
• Age
• Marital status
• Residence
• Occupation
• Educational status
• Monthly income
• Information access
Utilization of maternal health service related variables
• Attendance of ANC
• Number of ANC visit
• Provision of advice on breastfeeding by health care staff during ANC
• Attendance of PNC
• Place of delivery
• Birth attendance
Operational Definition
Antenatal care: Care given to pregnant women so that they have safe pregnancy and healthy baby [51].
Knowledge: In this study refers to awareness about colostrums feedings of pregnant woman during breast feeding period. It will be evaluated by the mothers answer to the questions [52].
Good knowledge: Those answers greater than or equal to 60% questions out of total knowledge related questions.
Poor knowledge: Those answers less than 60% questions out of total knowledge related questions.
Attitude: The way that you think and feel [52].
Positive attitude: Those who answer positively > 60% of attitude related questions.
Negative attitude: Those who answer positively to less than 60% of attitude related questions.
Practice: The overt behavior habit or custom of women [52].
Good practice: Score > 60% on the overall practice questions.
Poor practice: Those who answer <60% of practice related questions.
Data Collection Tools
The data was collected by using semi-structured questionnaire which contain variables as well as both open and close-ended questions in face to face interview [53]. The information was collected from each selected ANC attendant pregnant mothers and the questionnaire was delivered to assess KAP of colostrums feeding among ANC attendant pregnant mothers in MTUTH. Responses for open ended questions were written as statement while for close ended ones; there were choices to be selected from.
Data Processing and Analysis
The data was checked for its completeness and any incomplete information were excluded from entry after data collection. Data was processed using tally system for each item and processing carried out by investigators using related methods. The statistical procedure for analysis consists of simple frequency distribution, percentage and composition. Additionally, tables and figures were used to present the findings.
Pre-test
The questionnaire was pre-tested on 5% of the calculated sample size in Mizan health center which is not selected in the study before the actual data collection period. The questionnaire will be modified based on information obtained from pre-test results.
Data Quality Assurance
To maintain the quality of data, semi-structured and pre tested questionnaire was used to collect information on colostrums feeding. The questionnaires was prepared in English language and then translated to local language, i.e., Amharic. Then the questionnaires will be checked for completeness by principal investigators [54].
Ethical Consideration
A formal letter was obtained from college of health science, department of nursing of Mizan-Tepi University. The purpose of study was explained to the study subject at the time of data collection verbal consent will be taken from participants to conform whether they are willing to participate [54]. Those not willing to participate were given the right to do so. Confidentiality of respondents was also ensured throughout the research process.
Dissemination of Results
The findings of this study was presented to college of health science department of nursing and distributed to MTUTH office managers and to other organizations, such as health center working on related area.
Results
Socio-demographic characteristics
Two hundred seven mothers participated in study, of which 201 (97.10%) respond to our study without any rejection. Among mothers interviewed 85 (41.06%) were between 26-30 years of age followed by 52 (25.12%) were in between 31-35 years of age, 5 (2.4%) between 15- 20 years and the rest were above 30 years. Most mothers 122 (58.9%) residence was rural and remaining (41.06% n=85) was urban. Among respondents 177 (85.5%) mothers were multi-gravid and 30 (14.49%) were grand multi-Para (Table 1).
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Age | 15-20 21-25 26-30 31-35 36-40 41-45 Total |
5 48 85 52 17 0 207 |
2.4 23.18 41.06 25.12 8.2 0 100 |
| Ethnicity | Bench Kaffa Amahara Oromo Others Total |
120 33 27 3 24 207 |
57.97 15.94 13 1.44 11.59 100 |
| Level of education | Cannot read and write | 80 | 38.6 |
| Can read and write only | 25 | 12.07 | |
| Complete elementary school | 37 | 17.87 | |
| Complete secondary school | 20 | 9.66 | |
| Diploma and above | 45 | 21.73 | |
| Total | 207 | 100 | |
| Occupation of respondents | House wife NGO employee Government employee Self Others Total |
85 0 53 26 43 207 |
41.06 0 25.6 12.56 20.77 100 |
| Marital status | In marital union Divorced Single Widowed Total |
187 10 0 10 207 |
90.33 4.83 0 4.83 100 |
| Residence | Urban Rural Total |
85 122 207 |
41.06 58.9 100 |
| Parity | Multi-gravid Grand multi-Para Total |
177 30 207 |
85.5 14.49 100 |
Table 1: Socio-demographic characters of mothers attending ANC follow up in MTUTH Mizan Aman town, Ethiopia, 2017.
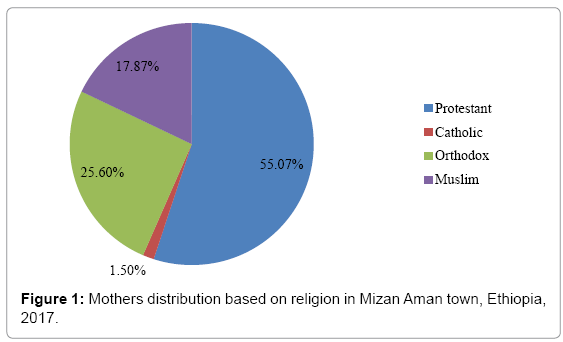
The dominant religion of study population were found to be protestant 114 (55.07%) followed by orthodox 53 (25.6%) and the rest were shown in Pie-chart 1. Most of the respondents 120 (57.97%) were Bench followed by Kaffa 33 (15.94%) . The analysis’ of educational level of mothers showed that 25 (12.07%) can read and write only, 80 (38.6%) cannot read and write, 37 (17.87%) complete elementary school, 20 (9.66% ) complete secondary school and the rest (21.73% n=45) were diploma and above. Most mothers 187 (90.33%,) were in marital union followed by divorced mothers 10 (4.83%) and 10(4.83%) were widowed mothers. Most mothers’ 85 (41.06%) responsibility was house wife and next 53 (25.6%) was governmental employee (Table 1 and Figure 1).
Maternal experience
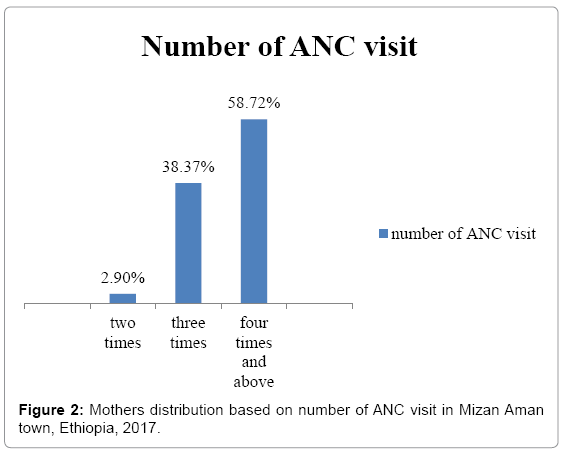
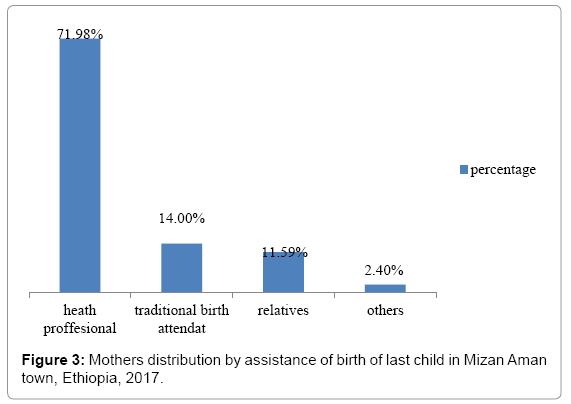
Out of interviewed mothers 93 (44.92%) had only one children in number. Most mothers 172 (83%) had ANC follow up for previous pregnancy but the remaining 35 (17%) had not. Among of those mothers 101 (58.72%) visit four times and 66 (38.37%) visit three times. Among 207 mothers 58 (28.01%) were delivered at home, 34 (16.42%) at health center, 112 (69.55%) at hospital and 3 (1.44%) were at private clinic. At the time of delivery most mothers 149 (71.98%) were attained by health professionals but others were attained by relatives 24 (11.59%) and traditional birth attendant 29 (14%). During delivery of baby 149 (71.98%) were counseled about colostrums feeding in addition to breast feeding but the remaining 58 (28.01%,) did not. About 116 (56%) had post natal follow up but the remaining 91(44%) did not. Among 116 mothers, 96 (82.75%) were counseled about colostrums feeding in addition to breast feeding during post natal care but 20 (17.25) did not. Among 207, 135 (65.2%) had got information about advantage of colostrums feeding, while the rest 72 (34.78%) had not. Concerning the source indicates that health professionals were main sources 95 (70.37%) followed by relatives 19 (14.07%), television 14 (10.37%), while rest 7 (5.18%) were from radio (Figures 2 and 3 and Tables 2 and 3).
| Number of children | Frequency | Percentage |
|---|---|---|
| Only one | 93 | 44.92 |
| 2-3 | 53 | 25.6 |
| 4-5 | 35 | 16.9 |
| >5 | 26 | 12.56 |
| Total | 207 | 100 |
Table 2: Mothers distribution by number of children they have in Mizan Aman town, Ethiopia, 2017.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Get information | Yes No Total |
135 72 207 |
65.2 34.78 100 |
| Source of information | Television Radio Health profession Relatives Total |
14 7 95 19 135 |
10.37 5.18 70.37 14.07 100 |
Table 3: Mothers distribution by get source information about advantages of colostrum feeding at Mizan Aman town Ethiopia, 2017.
Knowledge of respondents about colostrums feeding
According to the set criteria for colostrums feeding knowledge 153 (73.81%) were found to be knowledgeable, 54 (26.19%) fairly knowledgeable (Table 4).
| Level of knowledge | Frequency | Percentage |
|---|---|---|
| Good knowledge | 153 | 73.8 |
| Poor knowledge | 54 | 26.19 |
| Total | 207 | 100 |
Table 4: Mothers distribution by level of colostrums feeding knowledge at Mizan Aman town, Ethiopia, 2017.
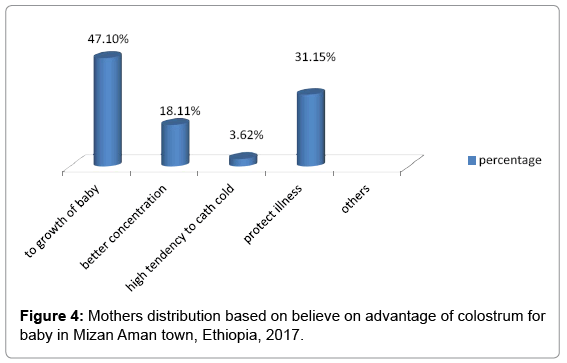
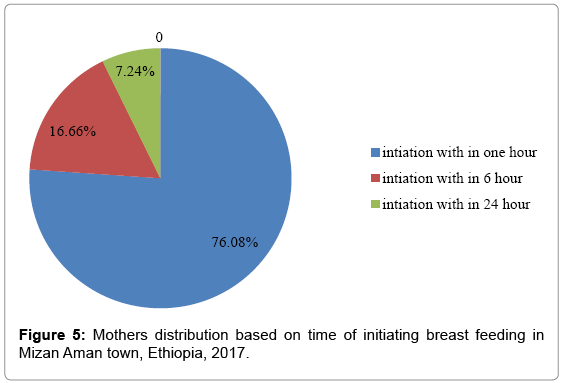
According to the response of mothers’on knowledge measuring questions the majority 138 (66.66%) believed that colostrums has advantage for baby. And most 105 (76.06%) respondent also believed that starting breast feeding within one hour after delivery is important. And 65 (47.10%) believed that colostrums is important for growth of baby and 119 (57.48%) fed colostrums when they were sick (Figures 4 and 5 and Tables 5 and 6).
| Should child feed colostrums when you are sick | Frequency | Percentage |
|---|---|---|
| Yes | 119 | 57.48 |
| No | 88 | 42.5 |
| total | 207 | 100 |
| Should child feed colostrums when he/she sick | ||
| Yes | 135 | 65.2 |
| No | 72 | 34.78 |
| Total | 207 | 100 |
Table 5: Mothers distribution who fed colostrums when they are sick in, Mizan Aman town, Ethiopia, 2017.
| If no, above two questions | Frequency | Percentage |
|---|---|---|
| It harms me | 20 | 26.3 |
| Baby unable to suck | 10 | 13.15 |
| Both it harms me and baby unable to suck | 46 | 60.5 |
| Total | 76 | 100 |
Table 6: Mother distribution who cannot feed colostrums when they are sick and baby is sick in Mizan Aman town, Ethiopia, 2017.
Attitude of respondent towards colostrums feeding
According to set of criteria for colostrums feeding attitude, this study indicated that the majority 144 (69.4%) of mothers have positive attitude towards colostrums feeding. But the remaining 63 (30.6%) have negative attitude. Almost all mothers (72.46%) agree that colostrums is important for growth and mental development (Tables 7 and 8).
| Level of attitude | Frequency | Percentage |
|---|---|---|
| Positive attitude | 144 | 69.4 |
| Negative attitude | 63 | 30.6 |
| Total | 207 | 100 |
Table 7: Mothers distribution by level of colostrum feeding attitude at Mizan Aman town, Ethiopia, 2017.
| Attitude towards colostrums | Response | Frequency | Percentage |
|---|---|---|---|
| Do you believe that the first milk (colostrum) should discarded | I agree | 40 | 19.3 |
| I do not agree | 149 | 71.98 | |
| Neutral | 18 | 8.69 | |
| total | 207 | 100 | |
| Colostrums is important for baby growth and development | I agree | 150 | 72.46 |
| I do not agree | 36 | 17.39 | |
| Neutral | 21 | 10.14 | |
| total | 207 | 100 | |
| Colostrums cause abdominal cramp and diarrhea | I agree | 29 | 14 |
| I do not agree | 149 | 71.98 | |
| Neutral | 29 | 14 | |
| total | 207 | 100 | |
| Colostrums is forbidden in culture | I agree | 55 | 26.51 |
| I do not agree | 112 | 54.10 | |
| Neutral Total |
40 207 |
19.32 100 |
|
| Colostrums is dirty part of milk | I agree | 42 | 20.28 |
| I do not agree | 148 | 71.49 | |
| Neutral | 17 | 8.21 | |
| Total | 207 | 100 | |
| Fathers support is important to give colostrums for baby | I agree | 154 | 74.39 |
| I do not agree | 35 | 16.9 | |
| Neutral | 18 | 8.69 | |
| Total | 207 | 100 |
Table 8: Mothers distribution based on attitude towards colostrum feeding in Mizan Aman town, Ethiopia, 2017.
Practice of respondents towards colostrums feeding
Among the mothers studied, higher proportion 158 (76.22%) gave colostrums for their baby, while the remaining 49 (23.67% ) did not. From those gave colostrums for their baby 101 (63.9%) start colostrums feeding within 1 h after delivery (Tables 9 and 10).
| Level of practice | Frequency | Percentage |
|---|---|---|
| Good practice | 126 | 60.88 |
| Poor practice | 81 | 39.14 |
| Total | 207 | 100 |
Table 9: Mothers distribution by level of colostrums feeding practice at Mizan Aman town, Ethiopia, 2017.
| Colostrum feeding practice | Frequency | Percentage |
|---|---|---|
| Yes | 161 | 77.77 |
| No | 46 | 22.22 |
| Total | 207 | 100 |
Table 10: Practices of mothers feeding colostrums their last child at Mizan Aman town, Ethiopia, 2017.
The reason for not giving colostrums was mothers believed that It is forbidden in culture 55 (26.57%), cause abdominal cramp and diarrhea 29 (14%) and it is dirty part of breast milk 42 (20.28%) (Table 11).
| If yes, how soon do you start to feed breast with colostrums after birth to your baby | Frequency | Percentage |
|---|---|---|
| Within 1 h after delivery | 102 | 63.35 |
| Within 6 h after delivery | 43 | 26.70 |
| Within 24 h after delivery | 16 | 9.93 |
| Total | 161 | 100 |
Table 11: Mothers distribution that start colostrums feeding within 1 h.
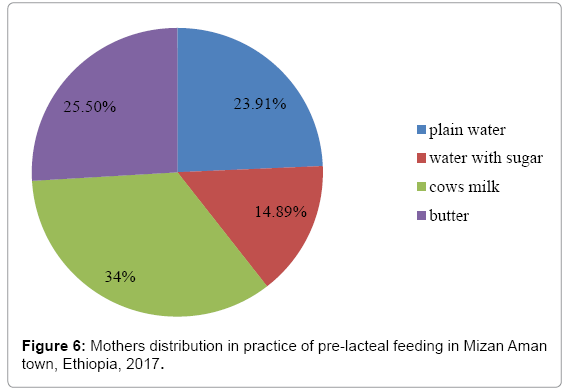
Concerning pre-lacteal feeding from 161 mothers 46 (28.57%) gave additional food before starting breast milk. Among those most (23.91% n=11) mothers have given plain water and 7 (14.89%) have gave water with sugar. The remaining 111 (71.42%) did not give any additional food before starting breast feeding (Figure 6).
Discussion
This study examined mothers Knowledge, Attitude and Practice towards colostrums feeding at Mizan Aman town, Ethiopia. Among mothers studied the majority 135 (65.2%) have had information on colostrums feeding during pregnancy from different source which means above half mothers have information but it is lower as compare to Nepal (74%). The variation may be because of socio- cultural difference between study areas. And also the variation may be due to sample size and study. Most respondents 95 (70.37%) received information on colostrums feeding from health professionals and it is greater than previous finding of EDHS2016 that was 62.7%. The gap may be due to small sample size in our study. This also shows that other sources of information such as television 14 (10.37%), radio 7 (5.18%) and relatives 19 (14.07%) did not have expected role in advertising colostrums feeding information for mothers,
Concerning about mother’s knowledge towards colostrums feeding 153 women (73.81%) has had knowledge. It is very higher than previous study in Dhahran (25%) has had knowledge about advantage of colostrums. The difference may be as result of socio cultural difference between Ethiopia and Dhahran or may be good awareness was created on advantage of colostrums feeding through health extension worker in Ethiopia and study period difference.
Regarding initiation of colostrums feeding 105 (76.06% ) of study population start colostrums within one hour but it is lower than colostrums feeding initiation in Nepal (92%). It is due to lack education during antenatal, delivery and postnatal period of pregnant mothers in our study area.
Our study shows that studied population believed that colostrums should discarded 40 (19.3%), it is dirty part of milk 42 (20.28%), forbidden in culture 55 (26.57%) and causing diarrhea and abdominal cramp 29 (14%) but this study gate different ideas, by which majority of mothers indicated that they offered colostrums for their baby immediately after birth 105 (76.08%) and verbalized as it is important for growth of body and mental development (47.10%), protect from illness (31.15%), high tendency to catch cold (3.62%) and have better nutrients concentration (18.11%). This indicates that better understanding about colostrums feeding among mothers, which is higher than pervious study (Raya kobo district, northern -east Ethiopia 2014) shows that studied believed that it colostrums is dirty part of milk (25.9%), have tradition (23.5%) and 58% not awarded. The reason behind variation may be cultural difference between Mizan Aman and Raya kobo.
The finding of this study indicates that 144 (69.4%) had a positive attitude which is higher than previous finding in Dhahran (20.6%). The reason behind variation may be our study concern on institutional based or small sample size and also may be it is due to lack awareness regarding colostrums feeding in Dhahran community.
In this study the prevalence of colostrums feeding practice was 126 (60.88%), which is lower than the prevalence of colostrums feeding practice reported from Bhaktapur, (80%). In consistent prevalence in colostrums feeding practice could be because the culture in Mizan Aman community is different to Bhaktapur. And also colostrums feeding practice is higher in our study area as compare to India (23%). The variation may be sociocultural difference between India and Mizan Aman (Ethiopia).
According to our study, 28.57% had practice pre-lacteal feeding, among those 25.5%were giving butter, which is lower than study report in Raya Kobo district that shows 37.8% of mothers were feed pre-lacteal feeding. The reason for variation is may be due to lack of awareness about colostrums and also it is due to cultural difference between Raya Kobo district and Mizan Aman town Ethiopia.
Conclusion
This study concludes that most of mothers had good knowledge and attitude on importance of colostrums feeding. Colostrums feeding practice was more common among mothers who gave birth at institution. Due to education promoting institutional delivery and creating awareness on advantage of colostrums feeding, increase colostrums-feeding practice.
Many pregnant women have awareness about colostrums feeding but the results study still indicate that further awareness are necessary to improve KAP of colostrums feeding in Mizan Aman town. And also this study shows most mothers have positive attitude towards colostrums feeding but some mother need further advice on colostrums feeding because they think colostrums case diarrhea and abdominal cramp, it is forbidden in culture and it is dirty part of milk.
References
- Ghai OP, Paul VK, Bagga A (2009) Textbook of Paediatrics. 7th edition. New Delhi: CBC Publisher and Distributors.
- Heather Fisher Senior Thesis Project (2007) Colostrum: Properties, functions and importance. The relationship between the immunoglobulin concentration in Holstein colostrum and the total senlm protein in Holstein heifer calves.
- Loureiro I, Frankel G, Adu-Bobie J, Dougan G, Trabulsi LR, et al. (2008) Human colostrum contains IgA antibodies reactive to enteropathogenic Escherichia coli virulence-associated proteins: Intimin, BfpA, EspA and EspB. J Pediatr Gastroenterol Nutr 27: 166-171.
- Arifeen S, Black RE, Antelman G, Baqui A, Caulfield L, et al. (2009) Exclusive breastfeeding reduces acute respiratory infection and diarrhoea deaths among infants in Dhaka slums. Pediatrics 108: e67.
- Rind J (2008) Knowledge, attitude and practice of employed mothers about breast feeding. Nurs J India 177: 17-19.
- Kumari S, Saili A, Jain S, Bhargava U, Gandhi G, et al. (2004) Maternal attitude and practices in initiation of newborn feeding. Indian J Paediatric 55: 905-911.
- Millikan K (2010) Cultural beliefs and practices of breast feeding. Nurs J India 8: 20-22.
- Snape WJ Jr, Carlson GM, Cohen S (1976) Colonic myoelectric activity in the irritable bowel syndrome. Gastroenterology 70: 326-330.
- Goldstein DJ, Barr RJ, Santa Cruz DJ (1982) Microcystic adnexal carcinoma: A distinct clinicopathologic entity. Cancer 50: 566-572.
- Morse JM, Jehle C, Gamble D (2008) Initiating breastfeeding: A world survey of the timing of postpartum breastfeeding. Int J Nurs Stud 27: 303-313.
- Bhale P, Jain S (1999) Is colostrum really discarded by Indian mothers? Indian Pediatric 36: 1069-1070.
- Goyle A, Jain P, Vyas S, Saraf H, Shekhawat, et al. (2004) Colostrum and prelacteal feeding practices followed by families of pavement and roadside squatter settlements. Indian J Prev Soc Med 25: 58-62.
- Duong DV, Binns CW, Lee AH (2004) Breast-feeding initiation and exclusive breast-feeding in rural Vietnam. Public Health Nutr 7: 795-799.
- Littler C (1997) Beliefs about colostrum among women from Bangladesh and their reasons for not giving it to the newborn. Midwives 110: 3-7.
- Derewicz M (2007) Mother’s Golden Milk. Chapel Hill, NC: University of North Carolina Global.
- Agrawal D, Agrawal K, Khare B (2013) Study on current status of infant and childhood feeding practices. Indian Pediatric.
- Galhotra A, Abrol A, Agarwal N, Goel N, Swami H (2008) Impact of community based awareness campaign on breast-feeding among lactating women in Chandigarh. Internet J Health.
- Osrin D, Tumbahangphe K, Shrestha D, Mesko N, Shrestha BP, et al. (2002) Cross sectional, community based study of care of newborn infants in Nepal. BMJ 325: 1063-1066.
- Wiryo H, Hakimi M (2005) Implementation of health education, based on ethnographic study, to increase the colostrum and decrease early solid food feeding. Health Educ Behav 32: 102-112.
- Utomo B, Fitria L, Sulacha E, Dachija D, Supeni K (2000) Feeding patterns, nutrient intake and nutritional status among children 0-23 months of age in Indramayu, West Java, 1997. Mal J Nutr 6: 147-170.
- Adair L, Popkin B (2012) Low birth weight reduces the likelihood of breast-feeding among Filipino infants. J Nutr 126: 103-112.
- Kaewsarn P, Moyle W, Creedy D (2009) Traditional postpartum practices among Thai women. J Adv Nurs 41: 358-366.
- Ludvigsson JF (2003) Breastfeeding intentions, patterns and determinants in infants visiting hospitals in La Paz, Bolivia. BMC Pediatric 3: 5-16.
- Gunnlaugsson G, Einarsdottir J (2013) Colostrum and ideas about bad milk: A case study from Guinea-Bissau. Soc Sci Med 36: 283-288.
- Okolo SN, Adewunmi YB, Okonji MC (2010) Current breastfeeding knowledge, attitude and practices of mothers in five rural communities in the savannah region of Nigeria. J Trop Pediatric 45: 323-326.
- Hussein A (2005) Breastfeeding and complementary feeding practices in Tanzania. East Afr J Public Health 2: 27-31.
- Bansal RK, Sitaraman S (2008) Colostrum deprivation: A misconception. Indian Pediatric 25: 396-397.
- Rizvi N (2007) Issues surrounding the promotion of colostrum feeding in rural Bangladesh. Ecol Food Nutr 30: 27-38.
- Engebretsen I, Wamani H, Karamagi C, Semiyaga N, Tumwine J, et al. (2007) Low adherence to exclusive breastfeeding in Eastern Uganda: A community-based cross-sectional study comparing dietary recall since birth with 24 h recall. BMC Pediatric 7: 10-22.
- UNICEF (2009) News note: World breastfeeding week celebrated in Ethiopia. New York: UNICEF.
- Ministry of Health, Family Health Department (2004) National strategy for infant and young child feeding. Addis Ababa: FMOH.
- Central Statistical Agency (2006) Ethiopia demographic and health survey 2005.
- Getahun Z, Scherbaum V, Taffese Y, Teshome B, Biesalski HK (2004) Breastfeeding in Tigray and Gonder, Ethiopia, with special reference to exclusive/almost exclusive breastfeeding beyond six months. Breastfeed Rev 12: 8-16.
- Academy for Educational Development, LINKAGES (2006) Breastfeeding, LAM, related complementary feeding and maternal nutrition program in Ethiopia. LINKAGES. Â
- John Snow Inc. (2009) Ethiopia: Promoting breastfeeding to ensure healthier babies. JSI.
- Almedom A (1991) Infant feeding in urban low-income households in Ethiopia: I. The weaning process. Ecol Food Nutr 25: 97-109.
- Joshi SK, Barakoti B, Lamsal S (2012) Colostrum feeding: Knowledge, attitude and practice in pregnant women in a teaching hospital in Nepal.
- Ekambaram M, Bhat VB, Ahamed MAP (2014) Knowledge, attitude and practice of breastfeeding among postnatal mothers. Curr Pediatric Res Med J.
- Chaudhary RN, Shah T, Raja S (2011) Knowledge and practice of mothers regarding breast feeding: A hospital based study. Health Renaissance 9: 194-200.
- Haider R, Rasheed S, Sanghvi TG, Hassan N, Pachon H, et al. (2010) Breastfeeding in infancy: Identifying the program-relevant issues in Bangladesh. Int Breastfeed J.
- Odent PLG (2011) Early infant feeding and neonatal survival in Nepal: Breastfeeding, colostrum and discarding of the first milk. Doctoral thesis, UCL (University College London).
- Ulak M, Chandyo RK, Mellander L, Shrestha PS, Strand TA (2012) Infant feeding practice in Bhaktapur, Nepal: A cross-sectional, health facility based survey.
- Ministry of health, New ERA and ORC Marco (2006) Nepal demographic health survey.
- Fjeld E, Siziya S, Katepa-Bwalya M, Kankasa C, Moland KM, et al. (2008) “No sister, the breast alone is not enough for my baby†a qualitative assessment of potentials and barriers in the promotion of exclusive breast feeding in southern Zambia. Int Breastfeed J.
- Dashti M, Scott JA, Edwards CA, Sighayer MA (2010) Determinants of breast feeding initiation among mothers In Kuwait, Int Breastfeed J.
- Legesse M, Demena M, Mesfin F, Haile D (2015) Factors associated with colostrum avoidance among mothers of children aged less than 24 months in Raya Kobo district, North-eastern Ethiopia: Community-based cross-sectional study. J Trop Pediatr 61: 357-363.
- Bench Maji Zone Health Bureau. Bench Maji Zone 2008 EC/2015 GC corrected population.
- Gerensea H, Gegziabher Y, Tsegay Y, Gtsadkan T, Kiros E (2016) Determinants of unwanted pregnancy and induced abortion among female youths in shire town, Tigray, Ethiopia, 2015. World J Pharm Med Res.
Citation: Shewasinad S, Manjura M, Bolesh A, Sisay D, Negash S (2017) Assessment of Knowledge, Attitude and Practice Towards Colostrum Feeding Among Antenatal Care Attendant Pregnant Mothers in Mizan Tepi University Teaching Hospital, Bench Maji Zone, SNNPR, South West Ethiopia, 2016/2017 G.C. J Preg Child Health 4: 348. DOI: 10.4172/2376-127X.1000348
Copyright: © 2017 Shewasinad S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 16516
- [From(publication date): 0-2017 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 13712
- PDF downloads: 2804