Colostrum Feeding Practice and Associated Factors Among Mothers Attending Child Immunization Clinic at Public Healthcare Facilities in Dire Dawa City, Eastern Ethiopia, in 2022
Received: 01-Jul-2023 / Manuscript No. nnp-23-103822 / Editor assigned: 07-Jul-2023 / PreQC No. nnp-23-103822 / Reviewed: 21-Jul-2023 / QC No. nnp-23-103822 / Revised: 24-Jul-2023 / Manuscript No. nnp-23-103822 / Published Date: 31-Jul-2023 DOI: 10.4172/2572-4983.1000324
Abstract
Introduction: Colostrum is yellow to orange colored milk produced during a first few days of lactation and it is rich in nutrients and antibodies that have great role in health of the new born baby. Despite the world health organization recommends that every new born baby has to feed breast milk with colostrum within one hour of delivery; poor colostrum feeding practice is still a common problem in Ethiopia. Objectives: Assess the practice of colostrum feeding and related factors among women attending a child immunization clinic in governmental health facilities in Dire Dawa City, Eastern Ethiopia, in 2022. Method: Institution based cross-sectional study was conducted from February 1–30/2022 in governmental health facilities of Dire Dawa administrative city among 292 mothers with baby less than or equal to 12 months. The data were collected by systematic random sampling technique and analyzed using Statistical Package of Social Sciences 25.0 version. Bivariate and multivariate logistic regression analyses was employed to estimate the crude and adjusted odds ratio with confidence interval of 95% and P value of less than 0.05 considered Statistically significant. Result: 68.8% [95% CI: 63.4-74.3] of the mothers had good colostrum feeding practice. Living in an urban area [AOR=2.52, 95% CI=1.08-5.88], having at least a secondary education [AOR=2.79, 95% CI=1.12- 6.98], having visited an antenatal clinic in the past [AOR=3.12, 95% CI=1.12-9.21], receiving counseling on when to start breastfeeding [AOR=2.59, 95% CI=1.02-6.59], receiving colostrum feeding counseling [AOR=2.65, 95% CI=1.12- 6.30], having a professional attend the birth [AOR=3.20, 95% CI=1.23-8.31], getting information from a professional [AOR=3.89, 95% CI=1.54-9.82], and having good knowledge of colostrum feeding [AOR=3.53, 95% CI=1.56-7.96] were found to be associated with practice of colostrum feeding. Conclusion: In the present study, even if more than two-thirds of mothers have good practice of CF, still its gap is wide with WHO recommendation on timely initiation of BF, with colostrum of more than 80%. Promoting antenatal care visits and maternal education on breastfeeding is recommended for the increasing colostrum feeding practice of the mothers.
Keywords
Dire Dawa; Practice; Milk; Colostrum
Introduction
Colostrum is the first milk or a viscous, yellow fluid that mammals’ mammary glands create in the final stages of pregnancy, right before giving birth, and throughout the early stages of breastfeeding. Although colostrum has less lipids and potassium than regular milk, it is much richer in proteins, carbs, vitamin A, and salt chloride. Because colostrum contains nutrients and antibodies that are essential in the protection of infections and nutritional issues, it is regarded as a baby’s first immunization and has a good impact on the prevention of childhood sickness and malnutrition. Additionally, it promotes the first bowel movement, which aids in clearing excess bilirubin, which is produced in huge amounts during birth, and prevents jaundice [1].
The World Health Organization (WHO) and United Nations Children’s Emergency Fund (UNICEF) advised mothers to exclusively breastfeed their infants for the first six months of their lives. They also advised against using bottles, teats, or pacifiers, and to continue breastfeeding until 24 months or later [2].
Despite the recommendations of the WHO, UNICEF, and Ethiopian Infant and Young Child Feeding (EIYCF) guidelines, many mothers in the country continue to discard colostrum because they view it as heavy, dirty milk, harmful to children’s health, lacking in nutrition, or as bad karma for the family and the infant given other pre-lacteal foods other than mother’s milk in the first few days after birth [3].
Negligent colostrum feeding practices can raise a newborn’s risk of infection, stunting, wasting, underweight, and death [4]. Therefore, the purpose of this study was to evaluate the colostrum feeding practice (CFP) and its associated factors in the government health facility of Dire Dawa Administrative City (DDAC), Eastern Ethiopia [5].
Methods and Materials
Study area and period
The study was conducted from February 1–30, 2022, in governmental health facilities in Dire Dawa City. Dire Dawa city is located about 515 km from Addis Ababa, the capital city of Ethiopia. The city has ten public health institutions, of which two are hospitals and eight are health centers [6].
Study design
An institutional-based cross-sectional study design was used [7].
Source population and study population
All moms who visited the child immunization clinics at the governmental health facilities in DDAC during the study period served as the study’s source population. All moms who attended child immunization clinics in particular governmental health institutions during the study period made up the study population [8].
Inclusion and exclusion criteria
All mothers who had baby less than or equal to twelve months and attended child immunization clinic at selected governmental health facilities, of DDAC were included [9].
Sample size determination
Based on research done in North West Ethiopia, where the prevalence of colostrum feeding practice was estimated to be 91.2% (38), the sample size was computed using a single population proportion formula while taking the following assumptions into account. Z value at alpha=0.05, or 1.96, is the crucial value for a normal distribution at a 95% confidence level. P = Expected Level of Practice of Colostrum Feeding, d = Margin of Error, 0.05. Therefore,
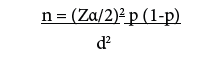
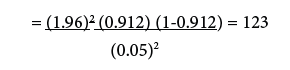
by considering 10% non-response rate and design effect 2 = 123 *10/100 = 123+13 = 136*2=272 [10].
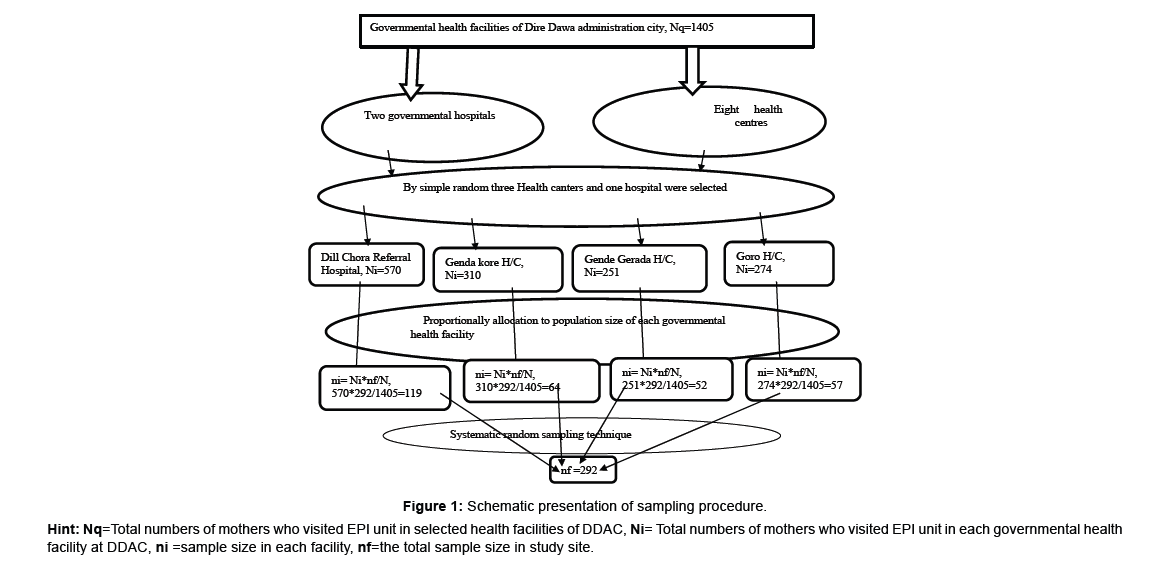
Sampling technique
The study population was chosen using a multi-stage sampling procedure. The administrative city’s public health facilities are divided into hospitals and health centers based on the ten public health facilities that DDAC possesses (two hospitals and eight health centers). Then one hospital and three health centers were chosen using a straightforward random sampling procedure. Based on each health facility’s quarterly extended program of immunization (EPI) unit flow, the total sample size was proportionally distributed for each of the administrative city’s health facilities [11].
Based on EPI registration books at all chosen health institutions, the average number of mothers who visited an EPI unit quarterly was 1405. In the Dilchora referral hospital (DCRH), Genda kore health center (GKHC), Gende Gerada health center (GGHC), and Goro health center (GHC), respectively, there were 570, 310, 251, and 274 mothers who visited the EPI unit on a quarterly basis [12].
After proportionate allocation, the overall sample size for DCRH, GKHC, GGHC, and GHC was 119, 64, 52, and 57 mothers, respectively. Each facility’s eligible mothers were chosen using a methodical random sampling process. By dividing the number of mothers who visited an EPI unit on a monthly basis by the sample size, the sampling interval or Kth units (1405/292 = 5) was calculated. The first Kth units in each healthcare facility were drawn at random to determine the starting unit (Figure 1).
Hint: Nq=Total numbers of mothers who visited EPI unit in selected health facilities of DDAC, Ni= Total numbers of mothers who visited EPI unit in each governmental health facility at DDAC, ni =sample size in each facility, nf=the total sample size in study site.Operational definition
Colostrum: is the yellowish breast milk during the three days following delivery (18).
Practice: The behavior, habit or custom of mothers of infants on CF to their current infants (19).
Good practice: Participant who responds for ≥ 60% of practice related questions(19).
Poor practice: Those participant who answer <60% of practice related questions (19).
Knowledge: In this study, knowledge refers to mothers’ understanding of colostrum breast milk and was assessed by mothers’ responses to knowledge-related questions. (19).
Good knowledge: Those mothers who answer ≥ 60% knowledge related questions (32).
Poor knowledge: Those mothers who answer < 60% knowledge related questions (19).
Study variables
Dependent variable: Colostrum feeding practice Independent factors: Age, place of residence, marital status, religion, level of education, line of work, partner’s level of education, and who she was living with are sociodemographic characteristics. Obstetric and reproductive factors: Parity, ANC visits, TIBF, CF, and BF counseling during ANC visits, delivery site, birth attendant, mode of delivery, and BF counseling following delivery. Factors relating to knowledge and practice: the information’s source.
Data collection tools
Data was gathered using a structured interviewer-administered questionnaire that was adjusted to the local context and derived from pertinent literatures. An expert in this language initially developed the questionnaires in English, after which they were translated into Amharic and then back into English to ensure uniformity. The questionnaire asked about socio demographic traits, obstetric and reproductive traits, as well as questions about knowledge and practice. Correct answers received a score of +1, while incorrect ones received a score of –1. Each mother’s score was added up and put into categories.
Data collection method
Data collection involved using a standardized intervieweradministered questionnaire that had been pre-tested. Four BSc midwives, a nurse, and a public health officer collected the data under the direction of a public health officer.
Data quality control
The instrument was pretested before the actual data collection, and the data were gathered by skilled data collectors. Prior to the actual data collection period, the questionnaire was pre-tested on 5% (15) of the moms who attended the child immunization clinic at Sabian General Hospital but were not included in the study. The investigator gave two days of training to the supervisors and data collectors. Additional adjustments were made based on the findings of the pre-test after the necessary modifications and corrections were made to standardize, ensure, and guarantee its reliability and validity. During data collection, data collectors verified that the data were comprehensive, and supervisors examined the data on a daily basis to ensure it was.
Data processing and analysis
The data were entered into Epi data 4.2, edited and cleaned for inconsistencies, missing values and outliers, then exported to SPSS version 25.0 for analysis. During analysis all explanatory variables which have significant association in bivariate analysis with P value <0.20 was entered into a multivariate logistic regression model to get adjusted odds ratio (AOR) and those variables with 95% of confidence intervals (CI) and a P value of < 0.05 was considered as statistically significance with CFP. Multi collinearity test was done using variance inflation factor and no collinearity exists between the independent variables. The model goodness of the test was checked by Hosmer- Lemeshow goodness of the fit and the p-value of the model fitness of the test was 0.780. Frequency tables, and descriptive summaries were used to describe the study variables.
Result
Socio demographic characteristics of child immunization clinic attendees
A total of 292 mothers participated in the study with a response rate of 100%. The mean age of the child immunization clinic attended mothers was 24.72 years with (±SD=4.55) ranging from 15-40 years. Of these, 134 (45.9%) of them found in the age group of 20-25 years. Majority of the mothers (80.5%) lived in urban and 278 (95.2%) of them were married. Of the child immunization clinic attendees 151 (51.7%) of them were Muslim religion followers. From the total child immunization attended mothers115 (39.4%) of them had primary educational level and 165 (56.5%) of them were house wife. Regarding to their partner educational level 87 (31.3%) of them had secondary educational level.
Reproductive and obstetric characteristics of the child immunization clinic attendees
In this study, 218 (74.7%) of the mothers were multigravida and 238 (81.5%) of them had history of ANC visit in their most recent pregnancy. Among mothers who had history of ANC visit, 195 (81.9%) of them were counselled on timely initiation of breast feeding (TIBF) during your ANC visits. One hundred seventy-six (73.9%) of them were counselled on CF and 189 (79.4%) counselled on exclusive breast feeding (EBF) for the first six months after delivery during their ANC visit. From the total child immunization clinic attended mothers 248 (84.9%) of them gave child birth at health institution and 253 (86.6%) of the birth were attended by health professional. Two hundred thirtytwo (79.5%) of the mothers were counseled about BF immediately after delivery and 255 (87.3%) of them were gave child birth vaginally.
Knowledge of the study participants on colostrum feeding
According to the above predetermined criteria, from total study participants 187 (64.0%) mothers had good knowledge about CF., and most of the mothers obtaining their information on colostrum from health professional (n=149, 51.1%).
Practice of study participants towards colostrum feeding
In our study, 259 (88.7%) of the mothers gave colostrum to their baby within three days after birth, while 33 (11.3%) did not provide colostrum and it may cause abdominal discomfort and diarrhea for the baby 13 (39.4%) was their mean reason not feeding colostrum. Of the participants 43 (14.7%) them were gave PLF to their baby and majority of them 24 (55.8%) gave infant formula milk. Two hundred ten (71.9%) of the mothers were put the baby to the breast immediately within an hour and 203 (69.5%) of them were start colostrum with breast milk feeding within an hour, while 287 (98.3) of the mothers were continued to give colostrum with breast milk within the first three days of delivery. Overall, in our study, according to the predetermined criteria, 201 (68.8%) mothers had good practice of CF.
Factors associated with colostrum feeding practice
In bivariate analysis variables which have significant association with a P value of <0.20 were age, residency, educational level of the mothers, parity, history of ANC visit, counselling on; TIBF, CF and EBF as well as place of deliver, giving child birth with the assistant of health care provider, counselling on BF after delivery, source of information and good knowledge of CF. In a multivariate logistic regression analysis; Living in an urban area [AOR=2.52, 95% CI=1.08- 5.88], having at least a secondary education [AOR=2.79, 95% CI=1.12- 6.98], having visited an antenatal clinic in the past [AOR=3.12, 95% CI=1.12-9.21], receiving counseling on when to start breastfeeding [AOR=2.59, 95% CI=1.02-6.59], receiving colostrum feeding counseling [AOR=2.65, 95% CI=1.12-6.30], having a professional attend the birth [AOR=3.20, 95% CI=1.23-8.31], getting information from a professional [AOR=3.89, 95% CI=1.54-9.82], and having good knowledge of colostrum feeding [AOR=3.53, 95% CI=1.56-7.96] were found to be associated with practice of colostrum feeding .
References
- Ward JD (2000) La Leche League: At the crossroads of medicine, feminism, and religion: UNC Press Books.
- Loureiro I, Frankel G, Adu-Bobie J, Dougan G, Trabulsi LR, et al. (1998) Human Colostrum Contains IgA Antibodies Reactive to EnteropathogenicEscherichia coli Virulence-Associated Proteins: Intimin, BfpA, EspA, and EspB. J Pediatr Gastroenterol Nutr 27(2): 166-71.
- Organization WH. Baby-friendly hospital initiative: revised, updated and expanded for integrated care. 2009.
- Haile D, Biadgilign S (2015) Higher breastfeeding performance index is associated with lower risk of illness in infants under six months in Ethiopia. Int Breastfeed J 10(1):1-7.
- McGuire S (2015) World Health Organization. Comprehensive Implementation Plan on Maternal, Infant, and Young Child Nutrition. Geneva, Switzerland, 2014. Adv Nutr 6(1):134.
- Abie B, Goshu Y (2019) Early initiation of breastfeeding and colostrum feeding among mothers of children aged less than 24 months in Debre Tabor, northwest Ethiopia: a cross-sectional study. BMC Res Notes 12(1): 65.
- Adugna D (2014) Women's perception and risk factors for delayed initiation of breastfeeding in Arba Minch Zuria, Southern Ethiopia. Int Breastfeed J 9: 8.
- Tamiru D, Belachew T, Loha E, Mohammed S (2012) Sub-optimal breastfeeding of infants during the first six months and associated factors in rural communities of Jimma Arjo Woreda, Southwest Ethiopia.
- Legesse M, Demena M, Mesfin F, Haile D (2015) Factors associated with colostrum avoidance among mothers of children aged less than 24 months in Raya Kobo district, North-eastern Ethiopia: community-based cross-sectional study. J Trop Pediatr 61(5): 357-63.
- Habtewold TD, Islam MA, Sharew NT, Mohammed SH, Birhanu MM, et al. (2017) SystEmatic review and meta-aNAlysis of infanT and young child feeding Practices (ENAT-P) in Ethiopia: protocol. BMJ Open 7(8).
- Amare ZY, Ahmed ME, Mehari AB (2019) Determinants of nutritional status among children under age 5 in Ethiopia: further analysis of the 2016 Ethiopia demographic and health survey. Global Health 15(62).
- Edmond K, Zandoh C,Quigley M, Amengo-Etego S, Owusu-Agyei S, et al. (2006) Delayed Breastfeeding Initiation Increases Risk of Neonatal Mortality. Ped 117: 380-6.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, GoogleScholar, Crossref
Indexed at, Google Scholar, Crossref
Indexedat, GoogleScholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Gemeda ND, Wirtu AW, Muse YG, Yilma SM, Getie SA, et al. (2023)Colostrum Feeding Practice and Associated Factors Among Mothers AttendingChild Immunization Clinic at Public Healthcare Facilities in Dire Dawa City, EasternEthiopia, in 2022. Neonat Pediatr Med 9: 324. DOI: 10.4172/2572-4983.1000324
Copyright: © 2023 Gemeda ND, et al. This is an open-access article distributedunder the terms of the Creative Commons Attribution License, which permitsunrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2039
- [From(publication date): 0-2023 - Dec 07, 2025]
- Breakdown by view type
- HTML page views: 1683
- PDF downloads: 356