Comparison of Weight Loss Outcomes and Resolution of Obesity Related Comorbidities Following Laparoscopic Sleeve Gastrectomy and Laparoscopic Gastric Bypass - Experience at a Single Metabolic and Bariatric Surgery Center of Srilanka
Received: 25-Jun-2022 / Manuscript No. JOWT-22-67734 / Editor assigned: 27-Jun-2022 / PreQC No. JOWT-22-67734(PQ) / Reviewed: 11-Jul-2022 / QC No. JOWT-22-67734 / Revised: 15-Jul-2022 / Manuscript No. JOWT-22-67734(R) / Published Date: 22-Jul-2022 DOI: 10.4172/2165-7904.1000503
Abstract
Laparoscopic gastric bypass (LGBP) and laparoscopic sleeve gastrectomy (LSG) are two of the commonest bariatric procedures performed in Asia. Gastric bypass performed either as Roux-en-Y gastric bypass or Mini-gastric bypass has shown to be a safe and effective procedure with good long term results. LSG, initially used as a first stage procedure in complex bariatric procedures is rapidly gaining popularity. With a simpler technical aspect and easy learning curve, LSG has shown good short term results in weight loss. The short and long term outcomes of these procedures are affected by multiple factors. Regional studies are required to assess effectiveness of each procedure and this data helps in selecting the suitable surgical approach to individual patients. In this retrospective study we analyzed weight loss outcomes and response of medical comorbidities between the two procedures after 1 year of follow-up. From 2017 January and 2021 January, 138 patients who underwent primary bariatric surgery were included in the study and were assigned for Laparoscopic Sleeve Gastrectomy (n= 84) and Laparoscopic Gastric Bypass (n= 54) by patient choice and informed consent. Data was collected on demographic factors, pre-operative body weight, body mass index (BMI), waist circumference, total body fat percentage and presence of obesity-related comorbidities. After 1 year of follow up weight loss outcomes and resolution of comorbidities were assessed. Both groups were comparable in age, sex and BMI. One year after surgery the LGBP group showed an excess weight loss percentage (%EWL) of 75.46% while the LSG group had a %EWL of 71.35% without statistical significance. Reduction in total body fat content and waist circumference was comparable between the two procedures. Patients in both groups had similar results for improvement and resolution of comorbidities without any statistical significance between the two procedures. In short term both LSG and LGBP were comparable in effectiveness within a Srilankan study population.
Keywords
Morbid obesity; Sleeve gastrectomy; Gastric bypass; Weight loss outcomes; Medical comorbidities
Introduction
Morbid obesity is an emerging health concern globally in the twenty-first century. Lack of physical exercise and unhealthy eating patterns have contributed to an increase in the prevalence of both obesity and obesity-related co-morbidities. Studies in Srilanka have shown a prevalence of 37.0%; and 15.8% for overweight; and obesity respectively within the urban community [1]. Morbid obesity is commonly associated with multiple comorbidities such as diabetes; hypertension; Ishaemic heart disease; obstructive sleep apnea (OSA); osteoarthritis of knee joints etc. These have a significant negative impact on the patient’s life. In addition morbid obesity is associated with an increased risk of cancer; psychological disorders and reduced quality of life. Obesity and its comorbidities contribute significantly to global health expenditure. Effective management of obesity and its associated comorbidities have become a health priority worldwide.
Bariatric and metabolic surgery as a management option for morbid obesity; is rapidly gaining popularity around the world. Surgery offers rapid and sustained weight loss compared to medical therapy and studies have demonstrated better resolution of obesity related comorbidities [2]. These benefits have even been showed in patients with class 1 obesity [3]. Benefits of surgery to the patient and the health care sector of the country are massive. With advanced anesthetic and surgical techniques used over the last few decades; these surgeries have become safe and effective.
Bariatric surgical procedures have evolved overtime. Initially surgeries were performed as open procedures but now with the advent of minimally invasive surgery; surgeries are performed exclusively using laparoscopy. The surgical procedures can be classified as malabsoptive surgeries or restrictive surgeries. Laparoscopic gastric bypass (LGBP); laparoscopic sleeve gastrectomy (LSG) and laparoscopic adjustable gastric band (LAGB) are the commonest surgeries practiced around the globe and are well established in the management of morbid obesity. Numerous other surgical and endoscopic procedures have also been described but the use of them is scarce. In Srilanka; laparoscopic sleeve gastrectomy and laparoscopic gastric bypass are the commonest procedures performed.
Laparoscopic gastric bypass has both restrictive and malabsorptive properties. There are two configurations to which the surgery can be performed - Roux-en–Y gastric bypass (RYGB) or Mini gastric bypass (MGB). Laparoscopic RYBG is considered the gold standard bariatric procedure and is commonly performed around the world. Minigastric bypass is a relatively novel procedure with similar effects [4]. Laparoscopic gastric bypass is proven to be effective with good weight loss outcomes and improvements in medical comorbidities such as diabetes [5]. However it is a technically demanding procedure with a longer learning curve.
Sleeve gastrectomy is a restrictive procedure where 70-80% of the stomach is removed to create a narrow gastric tube. LSG was initially used as the first stage surgery in staged bariatric procedures for high risk patients or super-obese patients who are undergoing complex bariatric surgeries. LSG is a faster and relatively technically simpler procedure with effective weight loss and resolution of comorbidities and is gaining popularity in many countries [6]. There is less chance of nutritional deficiencies and there are no complications associated with bowel anastomosis.
Weight loss after a bariatric procedure is dependent on multiple factors. Does the surgical procedure itself have an effect in the given community? Numerous studies have been carried out to compare the effectiveness of these two procedures. Studies in the Srilankan community are scarce. In this retrospective study we compared the two procedures within a similar patient cohort to assess the weight loss outcomes and resolution of medical comorbidities within the Srilankan setup.
Methods
This single-institution retrospective study was conducted at the University surgical unit of Colombo South Teaching Hospital (CSTH); Kalubowila; Srilanka. Morbidly obese patients who underwent primary bariatric surgeries between January 2017 to January 2021 were included in the study. Laparoscopic sleeve gastrectomy (LSG) and laparoscopic gastric bypass (LGBP) were the two commonest bariatric procedures performed within the unit. Patients were assigned to a laparoscopic sleeve gastrectomy or laparoscopic gastric bypass after a multidisciplinary discussion where patient expectations were considered after explaining the advantages and disadvantages of each procedure. All surgeries were performed by one senior surgeon specialized in Metabolic and bariatric surgery.
Data on demographic factors; pre-operative body weight; body mass index (BMI); waist circumference; total body fat percentage and presence of obesity-related comorbidities - diabetes; hypertension; dyslipidemia and obstructive sleep apnea (OSA) were recorded. Waist circumference was measured using a standard technique in all patients. Total body fat percentage was measured using a bioelectrical impedance analysis (BIA) machine. Bioelectrical impedance analysis utilizes electric current flow to assess impedance/resistance of the body tissue to estimate body composition – Body fat and muscle mass.
Postoperatively these patients were regularly followed-up in the surgical clinic and were assessed after 1 year of surgery. After one year; the percentage of excess weight loss and reduction in waist circumference & total body fat were calculated in each group. Patients with diabetes; hypertension and dyslipidemia were followed up with serial HbA1c measurements; blood pressure measurements and lipid profiles to determine the response to surgery. Weight loss outcomes and improvements in medical comorbidities were assessed between the two surgical procedures after 1 year of surgery.
Weight loss outcomes were assessed as a percentage of excess weight loss (%EWL). Each patient’s ideal body weight was calculated according to the height of the patient using standard BMI charts for Asians. Calculation of %EWL is as follows -
Excess weight (EW) was calculated using the following formula – EW = Preoperative weight minus ideal body weight (IBW).
Percentage of EWL was calculated according to following formula – %EWL = 100 x (Weight loss/EW)
Reduction in waist circumference and total body fat content were converted to a percentage of the pre-operative values.
Data was retrieved from patients’ medical records and the database maintained on operated patients. Data were recorded by a separate investigator in data collection forms to avoid observer bias. The consent to recruit in the study was obtained by interviewing patients.
Data analysis was done using IBM SPSS statistics version 25. Chi square test and t-test were used to assess for stastical significance. Ethical clearance for the study was obtained from Ethical Review Committee; CSTH and hospital administration.
Surgical technique
In Laparoscopic sleeve gastrectomy the greater curvature of the stomach was mobilized from the pylorus upto the angle of His with complete mobilization of the fundus. A narrow gastric tube was created over a 36F bougie starting from 5 cm proximal to pylorus up to the fundus using endoGI staplers. A Leak test was routinely performed. Following removal of the specimen; the stapler line was reinforced with a 4-0 PDS continuous suture.
In LRYGB a 30 ml gastric pouch was created at the level of the 2nd vascular arcade on the lesser curvature. The length of the gastric limb was kept at 100 cm. The side to side Gastrojejunostomy was created using a 45 mm gold linear stapler and the enterotomy was closed in single layer using 4-0 PDS. The biliopancreatic limb was anastomosed to the jejunum 50 cm down the small bowel. The side to side jejunojejunostomy was created using 45 mm blue linear stapler. The Peterson’s defect was closed routinely.
In MGB the gastric pouch was created at the level of the incisura. The fundus was completely mobilized along the greater curvature. The jejunum was traced 150cm down from the DJ flexure and a side to side Gastrojejunostomy was created using a 45mm gold EndoGI stapler. The enterotomy was closed using 4-O PDs running suture. A leak test was routinely performed in both procedures.
Postoperatively patients were observed in an ICU or HDU setup initially. Oral fluids and mobilization were started on the 1st postoperative day. Patients were discharged on the first or second postoperative day when discharge criteria were met - tolerating oral liquid diet; pain free; mobilizing fully etc.
Postoperatively patients were regularly followed up upto 1 year after surgery. During these follow up visits weight loss and improvements in medical comorbidities were recorded.
Results
Of the 165 patients operated between 2017 January and 2021 January; 138 patients were included in the study while 27 patients were lost to follow up. Of these 84 patients underwent Laparoscopic Sleeve Gastrectomy and 54 patients underwent Laparoscopic Gastric Bypass. Of the LGBP group 39 patients underwent Mini-Gastric Bypass and 15 underwent Roux-en-Y Gastric Bypass. The majority of patients who underwent bariatric surgeries were females n=114; 82.6% and patient cohort had a mean age of 38.6yrs with a range of 13-63 years. Both the LSG and LGBP group were comparable in age; sex and BMI (Table 1).
| Characteristic | LSG (Laparoscopic sleeve gastrectomy) | LGBP (Laparoscopic gastric bypass) | p value |
|---|---|---|---|
| Mean Age (years) | 38.2±10.3 | 39.1±9.8 | P > 0.05 |
| Gender (n ;%) | F - 71(83%) M- 13(17%) |
F – 43(80%) M- 11(20%) |
P > 0.05 |
| BMI (kg/m2) | 44.5±5.9 | 46.4±8.6 | P > 0.05 |
Table 1: Both the LSG and LGBP group were comparable in age; sex and BMI.
The presence of DM; HT; DL and OSA was assessed between the two groups. Out of the total study population 112(81.2%) patients had one or multiple comorbidities (Table 2).
| Comorbidity | LSG (Laparoscopic sleeve gastrectomy) | LGBP (Laparoscopic gastric bypass) |
|---|---|---|
| Diabetes (n) | 20 | 24 |
| Hypertension (n) | 33 | 26 |
| Dyslipidaemia (n) | 37 | 36 |
| OSA (Obstructive sleep apnea) (n) | 35 | 24 |
Table 2: Presence of DM; HT; DL and OSA was assessed between the two groups.
Postoperatively at 1 year after surgery; patients were assessed for weight loss; waist circumference reduction and reduction in total body fat percentage. The percentage of EWL was 75.46% in the LGBP group and 71.35% in the LSG group. There was no statistical significance between the two groups; p>0.05.
The mean waist circumference preoperatively of the LSG group was 115.9cm and in the LGBP group was 118.7cm. After 1 year of surgery; there was a 16.9% reduction of the waist circumference in the LSG group and a 14.2% reduction in the LGBP group (p value > 0.05).
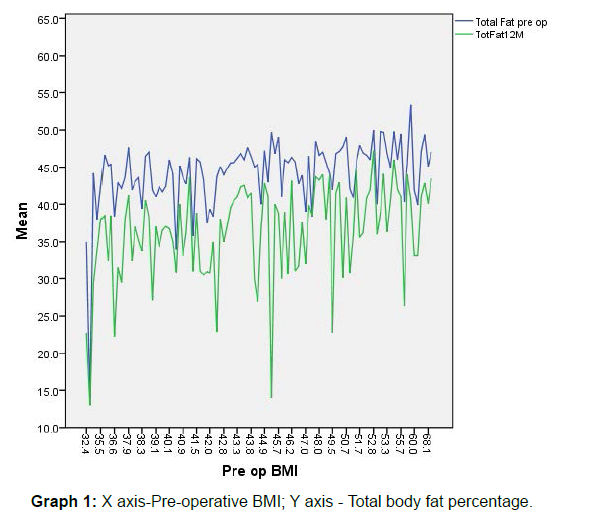
The mean total body fat percentage of the patients who underwent LSG was 44.58% compared to 43.53% for LGBP; p > 0.05. After 1 year of surgery the percentage of reduction in total body fat mass was 18.92% for LSG and 16.73% for gastric bypass; p > 0.05. Total body fat percentage pre-operatively and after 1 year are plotted against the BMI of each patient in Graph 1 which showed a consitent reduction in relation to pre-operative BMI.
Medical comorbidity outcomes were assessed 1 year postoperatively and are summarized in (Table 3). Majority of patients had improvements in the medical conditions with some showing remission.
| Comorbidity | LSG | LGBP | P Value |
|---|---|---|---|
| Diabetes | I – 44% R- 52% |
I – 64% R – 36% |
P >0.05 |
| Hypertension | I – 52% R – 27% |
I – 46% R – 34% |
P >0.05 |
| Dyslipidaemia | I – 43% R – 16% |
I – 30% R – 5% |
P >0.05 |
| OSA | R – 91% | R – 83% | P >0.05 |
| LSG – Laparoscopic sleeve gastrectomy ; LGBP – Laparoscopic gastric bypass I – Improvement ; R - Remission |
Table 3: Comorbidity outcomes after 1 year.
Discussion
Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are the most commonly performed bariatric procedures worldwide. Multiple factors have to be considered when selecting a procedure to a particular patient. Surgeons should consider the pros and cons of each procedure; patient preferences and surgeon experience before deciding the most appropriate procedure.
Laparoscopic Roux-en–Y gastric bypass is a well-established bariatric procedure and is considered the procedure of choice in many countries around the world. It is a safe and effective procedure with good long term results. It is a technically challenging procedure; requires longer operative time and has a risk of nutritional deficiencies. However the benefits of weight loss far outweigh the risks associated with the procedure [6]. Laparoscopic Mini gastric bypass is a relatively novel procedure. It is surgically less challenging than RYGB; but has shown to be as effective as RYGB. A meta-analysis and systematic review conducted by Wang et al; in 2018 showed that MGB offered better weight loss outcomes and better remission rates for diabetes compared to RYGB [7].
Laparoscopic Sleeve gastrectomy (LSG) was initially considered a first stage surgery in the super obese. The rationale of a first stage procedure in the super obese was to reduce sufficient weight and achieve control of comorbidities prior to a second stage definitive surgery. This would in turn increase patient safety and helps achieve good weight loss [8]. However follow-up of these patients showed that a higher proportion of patient’s didn’t require a second stage surgery as there was sufficient weight loss with LSG alone. These reports suggested that LSG is suitable option for weight reduction as a definitive procedure. In LSG about 2/3 of the stomach is removed including the fundus. Removal of the fundus of the stomach leads to decreased levels of Ghrelin; an orexigenic hormone. Reduction of Ghrelin in the body is a major factor implicated with weight loss [9].
Numerous studies have assessed the weight loss outcomes and effect on comorbidities between the two procedures. The main aim of these studies was to assess if LSG; as a solo procedure had adequate weight loss outcomes compared to LGBP. Most of the studies carried out around the world showed similar results between the two procedures. However weight loss outcomes within the Asian population who have a different body type to Caucasians (higher incidence of central obesity and higher body fat content) had to also be assessed [10].
In 2010; Lakdawal et al reported 72.1% EWL for LSG patients and 62.2% EWL for LRYGB patients in a study conducted in India [11]. A similar study conducted by Leyba et al in 2011 showed similar results with EWL of 78.8% for LSG group and 86% EWL for LRYGB without statistical significance [12]. These results show that both surgeries have similar weight loss outcomes in the short term. In our study EWL was 71.35% in the LSG group and 75.46% in the LGBP group with no statistical significance. These values suggest a good response to surgery and patients in both surgical arms had good results after surgery. Similarly waist circumference and total body fat reduction showed effective results in both procedures. Waist circumference and total body fat content are markers of central obesity and excess fat content compared to lean body mass. Bariatric surgery proves to be effective in achieving significant reductions in body fat mass. De Aquino et al; 2012 showed that Laparoscopic RYGB resulted in a reduction of fat content from 48.76% to 41.49% after six months of surgery [13]. This equated to a 7.3% (14.9%) reduction on fat content. In our study after 1 year of surgery percentage of reduction in total body fat mass was 18.92% for LSG group and 16.73% for gastric bypass group.
Factors affecting weight loss after LSG include bougie size; complete removal of the fundus and extend of gastric antral resection. In our study population the gastric tube was calibrated to a bougie size of 36F. The Indian study conducted by Lakdawal et al; similarly used a bougie size of 36Fr and the weight loss outcomes were similar in both studies. There is ongoing debate over the ideal bougie size. There is a wide variation in the bougie sizes used by surgeons ranging from 36Fr up to 48Fr. Use of a thinner bougie size is associated with a greater weight loss but runs the risk of stapler line leakage and higher postoperative Gastro-esophageal reflux(GERD) [14,15]. Within our study population no stapler line leaks were seen and after 1 year of follow up only 2 patients had persistent symptoms of GERD. Similarly there was significant weight loss after 1 year- 71.35% EWL. A study conducted by Wang et al in 2018 showed that use of a thinner bougie did not significantly increase the risk of leaks or GORD [16].
In our study population the surgical technique was kept consistent. In LSG complete mobilization and resection of the fundus was a key component of the surgery. The resection distance from the pylorus was kept at 5cm from the pylorus. With these steps we were able to achieve a substantial weight loss within our LSG group of patients. Long-term follow up is carried out to assess the response in 5 years.
Ethnicity has also been implicated as a factor in the effectiveness of LSG. Findings of our research correlate with other studies done within the Asian population. Han et al is 2005 found that LSG resulted in a EWL of 83.3% at 1 year [17]. The effect of ethnicity needs to be considered. Compared to Caucasian population; Asians are associated with better weight loss outcomes following LSG. Further long term research is required to establish a definitive relationship [18-20]. The effect of ethnicity on the effect of weight loss needs to be evaluated.
Metabolic outcomes were assessed for diabetes; hypertension; dyslipidemia and OSA. Within our study population; a higher number of patients had associated medical comorbidities. 81.2% of the population had at least one associated medical condition. Among the obese patients of Srilanka undergoing bariatric procedures; central obesity and metabolic syndrome are commonly seen.
At 1 year; 52% of the diabetic patients who underwent LSG showed remission of DM; while 36% of LGBP population had remission of DM. However at 1 year; almost all diabetics of the GBP group had improvements in glycemic control while 96% of the LSG group had achieved better glycemic control. There was no statistical significance between the two procedures. Our results are comparable with other studies within the Asian region. Lakdawal et al showed that after 1year LSG and LGBP had similar effects on diabetes resolution. Han et al; reported a 100% resolution of DM after 1 year of LSG.
Response of hypertension and dyslipidemia was similar within the two study groups. Close to 80% of hypertensive patients in both surgical arms had achieved better control of hypertension. Within the LSG group 52% of hypertensive patients and 46% of the hypertensive patients of LGBP group had resolution of hypertension after 1 year. A higher percentage of patients who underwent LSG had better control of the total cholesterol levels at 1 year postoperatively but no statistical difference was noted between the two groups. Patients with OSA benefitted from both surgeries where there was remission rate of 91% in the LSG group while 83% remission rate within the LGBP group. No statistical significance was noted among each group.
In summary within our study population; both surgical procedures had satisfactory weight loss after 1 year. LGBP patients have a slightly better weight loss at 1 year compared to LSG. Both the procedures had statically similar reductions in waist circumference and total body fat percentage. Resolution of obesity related comorbidities were similar between the two procedures. Patients who underwent LSG had better response of DL and OSA.
Certain limitations were noted in our study. The study design was a retrospective observational study done within a short duration. The long-term effect of these two procedures has to be compared and we are planning to conduct a study with 5 year follow-up of these patients. The study population was small with unequal groups. Due to the Covid pandemic in early 2020 the number of surgeries was significantly limited in the years 2020 and 2021. During this period the follow-up of these patients were difficult due to travel restrictions and limited access to our clinics. This resulted in exclusion of these patients. However our study population included super obese patients (BIM>50kgm2) and high risk patients with multiple comorbidities and we were able to assess the response of these patients to bariatric surgery. Patients selected had regular follow-up with routine weight loss assessment and comorbidity assessment.
Conclusion
In conclusion the results of our study showed that both LSG and LGBP resulted in significant weight loss after 1 year. In short term; results of weight loss and effect on medical comorbidities were comparable between the two surgical procedures. Further follow-up and evaluation is required to assess the outcomes in the long term.
Declarations
Competing interests: The authors declare that they have no competing interests
Ethical approval: Ethical approval was obtained from the Ethics Review Committee of Colombo South Teaching Hospital
Funding: None.
References
- Somasundaram N, Ranathunga I, Gunawardana K, Ahamed M, Ediriweera D, et al. (2019) High Prevalence of Overweight/Obesity in Urban Sri Lanka: Findings from the Colombo Urban Study. J Diabetes Res: 1-9.
- Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, et al. (2017) Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 5-Year Outcomes. N Engl J Med 376: 641-651.
- Parikh M, Chung M, Sheth S, McMacken M, Zahra T, et al. (2014) Randomized pilot trial of bariatric surgery versus intensive medical weight management on diabetes remission in type 2 diabetic patients who do NOT meet NIH criteria for surgery and the role of soluble RAGE as a novel biomarker of success. Ann Surg 260: 617-624.
- Georgiadou D, Sergentanis TN, Nixon A, Diamantis T, Tsigris C, et al. (2014) Efficacy and safety of laparoscopic mini gastric bypass. A systematic review. Surg Obes Relat Dis 10: 984-991.
- David E Cummings, Joost Overduin, Karen E Foster-Schubert (2004) Gastric Bypass for Obesity: Mechanisms of Weight Loss and Diabetes Resolution. J Clin Endocrinol Metab 89: 2608-2615.
- Iannelli A, Dainese R, Piche T, Facchiano E, Gugenheim J (2008) Laparoscopic sleeve gastrectomy for morbid obesity. World J gastroenterol 14: 821-827.
- Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J (2000) Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg 232: 515-529.
- Wang FG, Yan WM, Yan M, Song MM (2018) Outcomes of Mini vs Roux-en-Y gastric bypass: A meta-analysis and systematic review. Int J Surg 56: 7-14.
- Gumbs AA, Gagner M, Dakin G, Pomp A (2007) Sleeve gastrectomy for morbid obesity. Obes Surg 17: 9620-969.
- Anderson B, Switzer NJ, Almamar A, Shi X, Birch DW, et al. (2013) The Impact of Laparoscopic Sleeve Gastrectomy on Plasma Ghrelin Levels: a Systematic Review. Obes Surg 23: 1476-1480.
- Misra A, Khurana L (2010) Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes 35: 167-187.
- Lakdawala MA, Bhasker A, Mulchandani D, Goel S, Jain S (2010) Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass in the Indian population: a retrospective 1 year study. Obes Surg 20: 1-6.
- Leyba JL, Aulestia SN, Llopis SN (2011) Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the treatment of morbid obesity. A prospective study of 117 patients. Obes Surg 21: 212–216.
- de Aquino LA, Pereira SE, de Souza Silva J, Sobrinho CJS, Ramalho A (2012) Bariatric surgery: impact on body composition after Roux-en-Y gastric bypass. Obes surg 22: 195–200.
- Aurora AR, Khaitan L, Saber AA (2012) Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg endosc 26: 1509-1515.
- Yuval JB, Mintz Y, Cohen MJ, Rivkind AI, Elazary R (2013) The effects of bougie caliber on leaks and excess weight loss following laparoscopic sleeve gastrectomy. Is there an ideal bougie size?. Obes surg 23: 1685-1691.
- Wang Y, Yi XY, Gong LL, Li QF, Zhang J, et al. (2018) The effectiveness and safety of laparoscopic sleeve gastrectomy with different sizes of bougie calibration: a systematic review and meta-analysis. Int J Surg 49: 32-38.
- Moon Han S, Kim WW, Oh JH (2005) Results of laparoscopic sleeve gastrectomy (LSG) at 1 year in morbidly obese Korean patients. Obes Surg 15: 1469-1475.
- Jaruvongvanich V, Wongjarupong N, Vantanasiri K, Samakkarnthai P, Ungprasert P (2019) Midterm Outcome of Laparoscopic Sleeve Gastrectomy in Asians: a Systematic Review and Meta-analysis. Obes Surg 30: 1459-1467.
- Mui WLM, Ng EW, Tsung BYS, Lam CCH, Yung MY (2008) Laparoscopic Sleeve Gastrectomy in Ethnic Obese Chinese. Obes Surg 18: 1571-1574.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Wijerathne TK, Kariyawasam GMD, Abeysinghe AAGK (2022) Comparison of Weight Loss Outcomes and Resolution of Obesity Related Comorbidities Following Laparoscopic Sleeve Gastrectomy and Laparoscopic Gastric Bypass - Experience at a Single Metabolic and Bariatric Surgery Center of Srilanka. J Obes Weight Loss Ther 12: 503. DOI: 10.4172/2165-7904.1000503
Copyright: © 2022 Wijerathne TK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4058
- [From(publication date): 0-2022 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 3566
- PDF downloads: 492