Research Article Open Access
Condom-Use by Students in a Higher Educational Institution in South Eastern Nigeria
Adinma JIB1*, Adinma ED2, Eke NO3 and Umeononihu OS1
1Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University, Teaching Hospital, Nnewi, Nigeria.
2Department of Community Medicine, Nnamdi Azikiwe University, Teaching Hospital Nnewi, Nigeria.
3Department of Obstetrics and Gynaecology, Federal Medical Centre, Keffi, Nigeria.
- *Corresponding Author:
- Adinma JIB
Faculty of Medicine
Department of Obstetrics and Gynaecology
Nnamdi Azikiwe University Teaching Hospital
Nnewi, Nigeria
Tel: +2348037080814
E-mail: brianadinma@yahoo.com
Received Date: June 14, 2016; Accepted Date: June 24, 2016; Published Date: July 01, 2016
Citation: Adinma JIB, Adinma ED, Eke NO, Umeononihu OS (2016) Condom-Use by Students in a Higher Educational Institution in South Eastern Nigeria. J Comm Pub Health Nurs 2:127. doi:10.4172/2471-9846.1000127
Copyright: © 2016 Adinma JIB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
Objective: To examines the prevalence and pattern of condom-use among Nigerian university undergraduates.
Methods: This is a cross-sectional questionnaire-based study of 276 undergraduate students from Nnamdi Azikiwe University, Awka, Nigeria, selected using simple random sampling method. Data analysis employed SPSS version 17.0.
Results: There were 168 (60.9%) males and 108 (39.1%) females’ respondents. Their age ranged from 16 to 35 years. Majority, 242 (87.7%) were single and most, 266 (96.4%) were Christians. Up to 266 (96.4%) and 172 (62.3%) were aware of male and female condoms respectively, while 198 (68.8%) respondents and 14 (5.1%) have ever used male and female condoms respectively. Eighty (42.1%) respondents were consistent with condom-use, while 150 (54.3%) and 78 (28.3%) of the respondents respectively, knew condoms could help prevent STIs, and pregnancy. Religion-belief 26 (33.3%) constituted the commonest inhibitor to condom-use. The most commonly known pitfall on condom-use by the respondents is ‘’condom-burst’’ 102 (37.0%). The most common source of information on condom-use by the respondents is media 88(31.9%).
Conclusion: Awareness of condom among the respondents was high, but usage was low. Religion constitute a major inhibitor to condom-use. Re-invigorating sexual and reproductive health enlightenment including condom-use, employing various media platforms is recommended.
Keywords
Condom use; Students; Higher institution; South east; Nigeria
Introduction
Sexual activity among adolescent and young adult is not uncommon and has been reported to be quite high among students in tertiary institutions in Nigeria [1]. HIV/AIDS and other sexually transmitted infections have remained a source of concern globally, especially to healthcare groups and organizations. There is high prevalence of sexually transmitted infections among the adolescents and young adults in Africa, mainly as a result of high risk behaviour and neglect of established preventive measures. Approximately 3.3 million young people are living with HIV/AIDS in sub Saharan Africa, and 76% of those affected in this group are women [2]. Africa accounted for higher than two thirds of people living with HIV/AIDS worldwide and 72% of new infections among adults and children. Africa also, contributed about 71% of the world’s AIDS-related deaths in 2011. Most transmission in Africa occurs in heterosexual relationships [3]. Nigeria is the most populous country in Africa and has the second highest number of people living with HIV/AIDS [4]. The current trend of HIV/AIDS and other sexually transmitted diseases (STDs) still shows a high prevalence in Nigeria despite concerted efforts towards its eradication.
Globally, an estimated 210 million women become pregnant each year, of which 80 million are unintended. In addition about 44 million women have induced abortions, of which 22 million are unsafe. Deaths from unsafe abortion account for 13% of maternal deaths worldwide [5-7]. Of the 4 million abortions that occur in Africa annually, Nigeria accounts for about 760,000 cases [8]. It is estimated that there are about 25 abortions per 1000 women aged 15-44 years [7]. Unsafe abortion causes over 36000 deaths annually in Nigeria, accounting for 30-40% of maternal deaths [9].
The need for consistent and correct use of condom, particularly among young adults, is increasing due to the rapid spread of the HIV. Also, condom is a veritable instrument in prevention of unwanted pregnancy and the unpleasant sequelae of unsafe abortion and maternal death. Its dual function in prevention of sexually transmitted infections as well as contraception makes it very important, especially for the adolescents and young adults who are at high risk of STIs and unwanted pregnancy. The undergraduate students of higher institutions mostly fall into this age category.
Studies on condom use in university populations are few, despite the vulnerability of students to unsafe sexual practices. Previous studies have shown a low prevalence of consistent condom use among undergraduate students [10]. This study is therefore necessary, as it reveals the prevailing trend in condom use in this category of people and the findings from this study will help in planning group specific healthcare and reproductive health programs and interventions aimed at instituting appropriate reproductive health behaviour and practices in adolescent and young adults.
Materials and Methods
This is a cross-sectional questionnaire based study of undergraduate students of the Nnamdi Azikiwe University, Anambra state, drawn from the two campuses – College of Health Sciences, Nnewi and the main campus at Awka. The Respondents were selected from the faculties of the two campuses using simple random sampling method. Oral consent was obtained from them following due explanation of the study. Only students that gave consents were recruited. The questionnaire schedule elicited information on the bio-social characteristics of respondents – age, sex, marital status, and religion; their awareness and use of condom; reasons for non-use of condom by those not using condom; indication for condom use; awareness of functions of condom; knowledge of the pitfalls of condom; and their source of information on condom. All together three hundred questionnaires were distributed but 276 were found usable after editing and coding. Data obtained was analysed using SPSS version 17.0. Statistical relationships between variables were calculated using the Chi-square test and a p-value of <0.05 at 95% confidence interval was considered significant for all statistical comparison.
Results
Table 1 shows the socio-demographic characteristics of the respondents. A total of 276 students were included in the study, 168 (60.9%) males and 108 (39.1%) females.
| Characteristics | Number | Percent |
|---|---|---|
| Age | ||
| 15 – 19 | 32 | 11.6 |
| 20 – 24 | 164 | 59.4 |
| 25 – 29 | 72 | 26.1 |
| 30 – 34 | 6 | 2.2 |
| 35 and above | 2 | 0.7 |
| Sex | ||
| Male | 168 | 60.9 |
| Female | 108 | 39.1 |
| Marital status | ||
| Single | 242 | 87.7 |
| Married | 34 | 12.3 |
| Christianity | 266 | 96.4 |
| Gordian religion | 2 | 0.7 |
| No response | 8 | 2.9 |
Table 1: Distribution by bio-social characteristics N=276.
The ages ranged from 16 to 35 years with a mean age of 23.6±1.1 years. The commonest age group was 20-24 years, 164 (59.4%) followed by 25-29 years, 72 (26.1%). Majority, 242 (87.7%) were single and most, 266 (96.4%) were Christians.
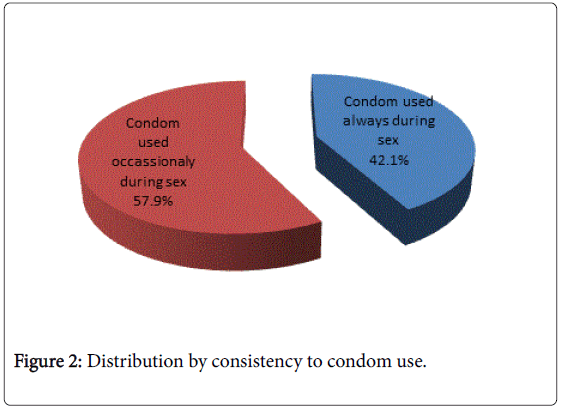
The distribution by awareness and usage of condom as shown in Table 2 indicates that 266 (96.4%) and 172 (62.3%) were aware of male condoms and female condoms respectively. This difference in awareness of male and female condoms by the respondents is significant [p<0.001]. One ninety (68.8%) respondents had ever used the male condom, 14 (5.1%) respondents have ever used the female condom and these had also ever used male condom. The identified difference between ever usage of male and female condoms among the respondents is significant [p<0.001]. There was also significant difference between awareness and use respectively of both male condoms [p<0.001] and female condoms [p<0.001]. Eighty (42.1%) of those who had ever used condoms were consistent in its use.
| Characteristics | Male condom | Female condombar chat | ||
|---|---|---|---|---|
| Number | Percent | Number | Percent | |
| Awareness | ||||
| Yes | 266 | 96.4 | 172 | 62.3 |
| No | 10 | 3.6 | 94 | 34.1 |
| NR | 0 | 0 | 10 | 3.6 |
| Ever used | ||||
| Yes | 190 | 68.8 | 14 | 5.1 |
| No | 78 | 28.3 | 254 | 92 |
| NR | 8 | 2.9 | 8 | 2.9 |
Table 2: Distribution by awareness and use of condom N=276.
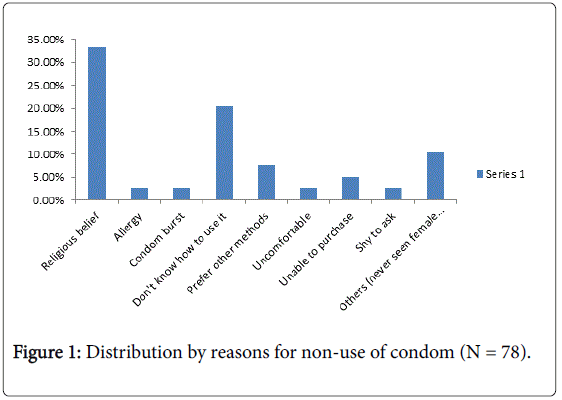
Figure 1 shows the distribution by reasons given by the respondents for non use of condom among the respondents who had not used condoms in the past. The commonest reason for non–use of condom was religious belief, 26 (33.3%), followed by not knowing how to use it, 16 (20.5%) and preference for other methods of contraception, 6 (7.7%). Lack of money was the reason for non use by 4 (5.1%) respondents.
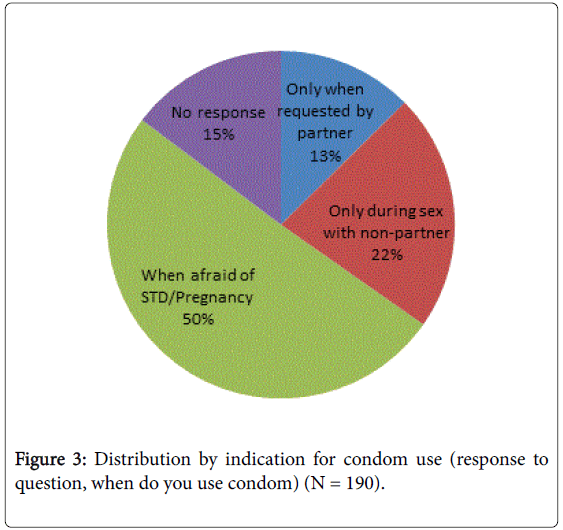
The distribution by consistency to condom use for respondents that use condom as shown in Figure 2 indicate that 80 (42.1%) of the respondents used condoms always during sex, while 110 (57.9%) used condoms occasionally during sex. Figure 3 show the distribution by the indication for the use of condom by the respondents. Many of the respondents, 96 (50.5%) used condoms when afraid of STI or pregnancy. However, few others used condoms only during sex with a non-regular partner, 42 (22.1%) and only when requested by partner, 24 (12.6%).
The distribution by awareness of the functions of condom as shown in Table 3 indicate that 150 (54.3%) are aware that it helps prevent STIs while 78 (28.3%) are aware that it helps prevent pregnancy.
| Characteristics | Number | Percent |
|---|---|---|
| Prevention of STIs | 150 | 54.3 |
| Prevention of pregnancy | 78 | 28.3 |
| Vaginal ultrasound | 6 | 2.2 |
| Treatment of premature ejaculation | 2 | 0.7 |
| Collection of sperm for laboratory tests | 0 | 0 |
| Protection from cervical cancer | 4 | 1.4 |
| NR | 36 | 13 |
Table 3: Distribution by awareness of functions of condom (n=276).
Knowledge of the pitfalls of condom use is shown on Table 4. One hundred and two (37.0%) respondents knew the condom could burst during sex, 60 (21.7%) knew it could delay orgasm in men, 30 (10.9%) knew it could be permeable to some microbes and 30 (10.9%) also knew it could cause allergic reaction.
| Characteristics | Number | Percent |
|---|---|---|
| Causes cancer | 18 | 6.5 |
| Can burst | 102 | 37 |
| Can be permeable to semen and microbes | 30 | 10.9 |
| Causes allergic reactions | 30 | 10.9 |
| Can delay orgasm in males | 60 | 21.7 |
| NR | 36 | 13 |
Table 4: Distribution by knowledge of pitfalls of condom (n=276).
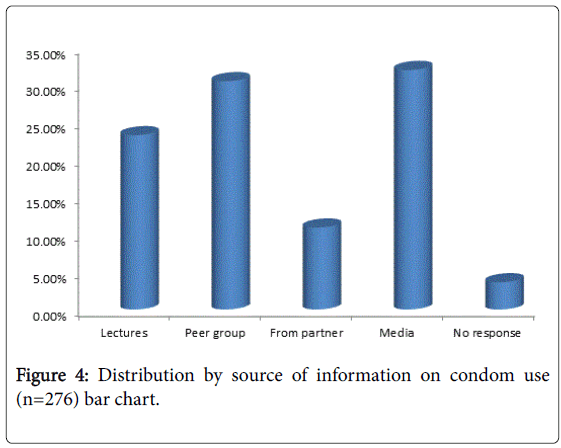
Figure 4 shows the sources of information on the condom among the respondents. The commonest source of information on condom use was through the mass media, 88 (31.9%), followed by peer group, 84 (30.4%) and lectures, 64 (23.2%).
Discussion
The awareness of the students on condoms use was high, as two hundred and sixty-six (96.4%) and 172 (62.3%) were aware of male condoms and female condoms respectively. The level of awareness of female condoms is much lower than findings of a study conducted by Oladeinde et al. [10] in Edo state of Nigeria among female undergraduate students where 93.8% of them were aware of female condoms. These levels of awareness are higher than the Nigerian national average levels [11] of awareness among females of 58.0% and 14.7% for male and female condoms respectively, and among males, 86.2% and 25.9% for male and female condoms respectively. This difference in awareness of male and female condoms by the respondents in this study is significant [p<0.001].
Only 190 (68.8%) and 14 (5.1%) of the respondents had ever used male and female condoms respectively. This is significantly lower than the levels of awareness of both male and female condoms in this group. This level of usage is also lower than findings from a study conducted by Olley at Ibadan, Nigeria [9] which showed the prevalence of condom use among undergraduate students to be 77%. In a similar manner to the findings on levels of awareness, the levels of usage of condom in this study are higher than the Nigerian national average levels [11] of condom use among females of 12.7% and 0.2% for male and female condoms respectively, and among males, 31.3% for male condoms. The findings are also higher than that from a study carried out by Izekor et al. in Edo state, Nigeria [8], which showed a condom usage level of 57.7% among undergraduate students. The level of condom usage from this study is however, similar to the findings from a study done by Ibe and Ibe at Port Harcourt, Nigeria [12] which revealed the prevalence of condom use to be 70.4% among undergraduates. The identified difference between ever usage of male and female condoms among the respondents is significant [p<0.001]. There was also significant difference between awareness and use respectively of both male condoms [p<0.001] and female condoms [p<0.001].
Only 80 (42.1%) of those who had ever used condoms were consistent in its use. This is quiet low and undesirable, considered from the point of view of the untoward consequences of unprotected sexual intercourse which includes mainly unwanted pregnancy and sexually transmitted infections together with their various short and long term complications. A similar pattern of inconsistent condom-use has been reported from various Nigeria studies. Ibe and Ibe [12] in a study conducted among undergraduates student at Port-Harcourt Nigeria reported that 82.4% had engaged in unprotected sex and that 29.6% never use condom during sex. While Fawole et al. [13] in another study carried out at Ilorin Nigeria reported that only 22.5% of sexually active undergraduate students had consistent use of condoms.
This frightening statistics on inconsistent condom use are not unrelated to the un-compelling reasons given by the respondents for their use of the condom–which in most cases are occasional viz, when afraid of pregnancy or STI (50%); only during sex with a non-regular partner (13%); and when requested by partner (22%)–reasons which still retain the risks of transmission of STIs and HIV, as well as unwanted pregnancy. This state of affair is no doubt not unrelated to the rather low number of respondents that had knowledge of the protective effect of condom use against sexually transmitted infections 54.3% and against unwanted pregnancy 28.3%! The commonest reason for non-use of condoms in this study was religious belief (35.0%). This has also been identified in some Nigerian national reviews as one of the common reasons for non-usage of condoms [14]. Religion has played a very important role albeit contentious in reproductive health matters. This may not be unrelated to the doctrinal identity of some religious denomination. The Catholic Church for instance does not uphold the use of artificial method of contraception including the condom for whatever reasons, on account of the church’s deontological bioethical orientation [15,16]. It is interesting to note that lack of knowledge on how to use a condom was given as a reason for non-use of the condom in 20% highlighting the necessity for adequate and proper sexuality education amongst this highly vulnerable population. The media constitute the highest source of information on condom use among the respondents in this study–31.9%. The media, particularly the social media has in recent times played a leading role as an avenue for the dissemination of reproductive health information amongst youth and adolescent, in contradistinction to what obtained more than twenty years ago where peer group had been reported to be a prominent source of information on reproductive health issues among young people [17-20]. It is desirable therefore that a reproductive health education disseminated through the media should be adequately monitored and vetted to ensure that young people are given reliable and correct information. Peer group however, still constituted an important source of information being the source in as high as 30.4%. Peer group is generally believed to be an unreliable source of information on reproductive health since often times the informants are ill-informed and therefore tend to give inaccurate information. The advent of the social media will no doubt, with time constitute an information verification platform that will begin to render ‘’peer group’’ source less acceptable as reproductive health information source.
Conclusion
The study shows that the knowledge of both male and female condoms was high, with knowledge of male condoms, being significantly higher. The use of both male and female condoms respectively, was lower than the knowledge, with the use of male condoms being significantly higher. The use of condoms was found to be significantly lower than the knowledge. There was also high level of inconsistent use of condoms. It is important therefore, to establish sexuality education programs in the higher educational institutions to help enhance safer sex practices by the undergraduate students. Sexuality education programmes leverage on the social media platform have the capacity for wider reach to the generality of young people and is being recommended to enable an improvement not only in condom use but in other sexual and reproductive health outcomes.
Acknowledgement
The authors are grateful to South East Nigeria (SE-PAC-Net) for sponsoring the conduct of this research.
Conflict of Interest
The authors have no conflict of interest.
References
- Izekor S, Osifo UC, Orhue PO, Momoh ARM, Airhomwanbo KO (2014) Knowledge and practice of condom-usage among undergraduate students in Edo State, Nigeria. IJCR 3: 12-18.
- AIDS epidemic update (2007) UNAIDS, Geneva Switzerland.
- UNICEF (2014)Child info: Monitoring the situation of children and women. Global and Regional Trends.
- Agboghoroma CO, Sagay SA, Ikechebelu JI (2013) Nigerian prevention of mother to child transmission of human immunodeficiency virus progress: The journey so far. J HIV Human Reprod1: 1-7.
- Sedgh G, Singh S, Shah IH, Ahman E, Henshaw SK, et al. (2012) Induced abortion: Incidence and trends worldwide from 1995 to 2008.Lancet 379: 625-632.
- World Health Organization (1998) Unsafe abortion. Global and regional estimates of incidence and mortality due to unsafe abortion with a listing of available country data.
- Bankole A, Oye-Adeniran BA, Sigh S (2006) Uwanted pregnancy: The root cause of induced abortion. In: BankoleA, Oye-Adeniran BA, Singh S (eds.) Unwanted pregnancy and induced abortion in Nigeria, causes and consequences. New York: Guttmacher Institute,pp: 10-13.
- Olley BO, Rotimi OJ (2003) Gender differences in condom use behaviour among students in a Nigerian university.Afr J Reprod Health 7: 83-91.
- Oladeinde BH, Omoregie R, Onifade AA, Olley M, Anunibe JA, et al. (2011) Awareness and use of female condoms among young nigerian women. Centrepoint Journal 17: 157-163.
- National Population Commission (NPC) {Nigeria} and ORC Macro (2009) Nigeria Demographic and Health Survey.
- Ibe SN, Ibe AU (2003) Condom use among sexually active students in Bori, Rivers State, Nigeria. African Journal of Applied Zoology & Environmental Biology 5: 49 – 54.
- Fawole AO, Ogunkan DV, Adegoke GS (2011) Sexual behaviour and perception of HIV/AIDS in Nigerian tertiary institutions: University of Ilorin, a case study. Global Journal of Human Social Science 11: 65-71.
- Iyaji A, Ogbuke MU (2011) Condom use in Nigeria: An evaluation. Current Research Journal Economic Theory 3: 10-13.
- Adinma JIB (2013) Bioethics in obstetrics. In: Stavros Sifakis and NikolaosVrachnis (eds.) From Preconception to Postpartum, pp: 979-953.
- Dickens BM (2005) Interactions of law and ethics affecting reproductive choice.Med Law 24: 549-559.
- Makwe E, Adenyuma MO (2014) Awareness of sexually transmitted infections (STIs) including HIV/AIDS among undergraduate students of University of Abuja. British Journal of Applied Science & Technology 4: 705-717.
- Adinma JI, Okeke AO (1995) Contraception: awareness and practice amongst Nigerian tertiary school girls.West Afr J Med 14: 34-38.
- Adinma JI, Nwosu BO (1995) Family planning knowledge and practice among Nigerian women attending an antenatal clinic.AdvContracept 11: 335-344.
- Adinma JI, Agbai AO, Okeke AO, Okaro JM (1999) Contraception in teenage Nigerian school girls.AdvContracept 15: 283-291.
- Adinma JIB, Adinma ED,Ikeako LC, Oguaka V, Egolum J (2016) Clinical pattern of sexually transmitted infection a mong nigeria students in a tertiary institution. World Academic Research Journal of Reproductive health and infectious diseases 2: 033-039.
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 14482
- [From(publication date):
August-2016 - Aug 18, 2025] - Breakdown by view type
- HTML page views : 13402
- PDF downloads : 1080