Conjugated and Synergistic Therapies in the treatment of Covid 19 Dysfunction - Pain, Weakness, Parestheria, Respiratory Condition, Memory, Olfactory and Taste: Case Series
Received: 26-Sep-2022 / Manuscript No. jnp-22-75902 / Editor assigned: 28-Sep-2022 / PreQC No. jnp-22-75902 (PQ) / Reviewed: 12-Oct-2022 / QC No. jnp-22-75902 / Revised: 17-Oct-2022 / Manuscript No. jnp-22-75902 (R) / Accepted Date: 26-Oct-2022 / Published Date: 24-Oct-2022
Abstract
The global pandemic of Sars-Cov-2 promoted 566 million infected and more than 6.3 million deaths, around the world. However, after infection, sequelae may appear, often persisting for more than 12 weeks, called post-COVID 19 sequelae, of systemic origin (fatigue and asthenia), respiratory (dyspnea and persistent cough), neuropsychiatric (memory loss, imbalance, anosmia, ageusia and anxiety) and musculoskeletal (myalgia and joint pain). In this context, new technologies and methodologies are developed for the treatment of these sequelae, often with the synergistic use of photonic, ultrasonic and negative pressure resources. In this work, 4 cases of patients with post-Covid 19 sequelae were gathered, from the most varied origins. They were followed up in evolution, varying the number of treatment sessions from case to case. The treatment carried out through these non-invasive and non-drug resources (laser, ultrasound and negative pressure) enabled the complete rehabilitation of these patients, returning their quality of life.
Keywords
Laser; Ultrasound; Suction Cup Therapy; Covid Sequelae; Memory; Breathing
Introduction
According to the World Health Organization (WHO) [1] the global pandemic of SARS-CoV-2 (COVID 19) was declared an emergency situation in late 2019 and early 2020, causing about 566 million infected and more than 6.3 million deaths. deaths, around the world (July/2022). After contagion, persistent sequelae may appear for more than 12 weeks, being called post COVID 19 syndrome, of which we can highlight the systemic manifestations (fatigue and asthenia), respiratory (dyspnea and persistent cough), neuropsychiatric (memory loss, imbalance, anosmia, ageusia and anxiety) and musculoskeletal (myalgia and joint pain).
SARS-CoV-2 is a virus formed by structural proteins called nucleocapsid, membrane, envelope and Spike, the latter being the glycoprotein responsible for the entry of viral particles into the host cell. It has two non-covalently associated subunits: S1, which binds to angiotensin-converting enzyme 2 (ACE2), and S2, which mediates membrane fusion by anchoring protein S to it [2]. The most common physiological change caused by the disease COVID-19 is respiratory [3], but there are several other changes reported, such as an increase in the index of inflammation mediators [4]; alteration in carbohydrate metabolism by deregulating the endocrine function of the pancreas and worsening glycemic control [5]; changes in cardiac activity, such as thickening of the cardiac chambers and heart failure [6]; hepatic [6] and renal [8] failure. In addition, there are reports of neurological manifestations secondary to the infection, such as encephalopathy, meningitis, stroke, encephalitis, Giullian-Barré syndrome, headache, dizziness, hyposmia, reduced level of consciousness, hypogeusia, myalgia and myelitis [3,9,10,11]. Neurocognitive deficits were also cited, characterized by episodic memory deficits [11].
Currently, the sequelae resulting from the post-Covid syndrome have been highlighted as a need for new technologies for treatment, such as photonic technologies associated with ultrasonic technology and negative pressure, which are allowing the rehabilitation of patients from the most varied sequels of COVID 19, such as smell. and taste. Among the combined technologies, the association of laser and ultrasound with the objective of analgesia and reduction of the inflammatory process stands out, since both have vasodilating properties generating a signaling cascade that allows greater tissue ionic permeabilization. According to Enwemeka (2004) [12] and Karu, (2006) [13], the use of photobiomodulation promotes several beneficial effects such as reducing edema and the inflammatory process, increasing analgesic effects, tissue healing, collagen synthesis and ATP production acting in the regulation of homeostasis. The ultrasound, in turn, from mechanical waves, promotes cavitation, greater ionic permeabilization, analgesia and anti-inflammatory action. The overlapping of therapeutic fields promotes a potentialization of individual resources.
Also, vacuum therapy is able to alleviate muscle tension promoting analgesia. Studies show that the application of vacuum therapy in the cervical region produces local redness, resulting in increased blood circulation and muscle relaxation. In addition, the realignment of the fibers occurs by means of the decrease in sliding pressure on the fascia, providing relaxation of the treated region [14]. When associated with laser, the analgesic and anti-inflammatory condition is amplified,increasing the benefits of the combined technique.
Recently, these new technologies have been developed by the Physics Institute of São Carlos (IFSC), University of São Paulo, in the treatment of various pathologies such as arthritis [15], fibromyalgia [16], Parkinson's disease [14], facial disorders [17], adhesive capsulitis [18] and limb and trunk injuries [19].
The objective of this study was to follow the treatment and evolution of 4 cases with different complexities using photonic technologies associated with other therapeutic resources, such as ultrasound and negative pressure, applied in a conjugated and synergistic way, thus promoting the overlap of the therapeutic laser fields. and ultrasound and laser and negative pressure.
Materials and methods
Case 1
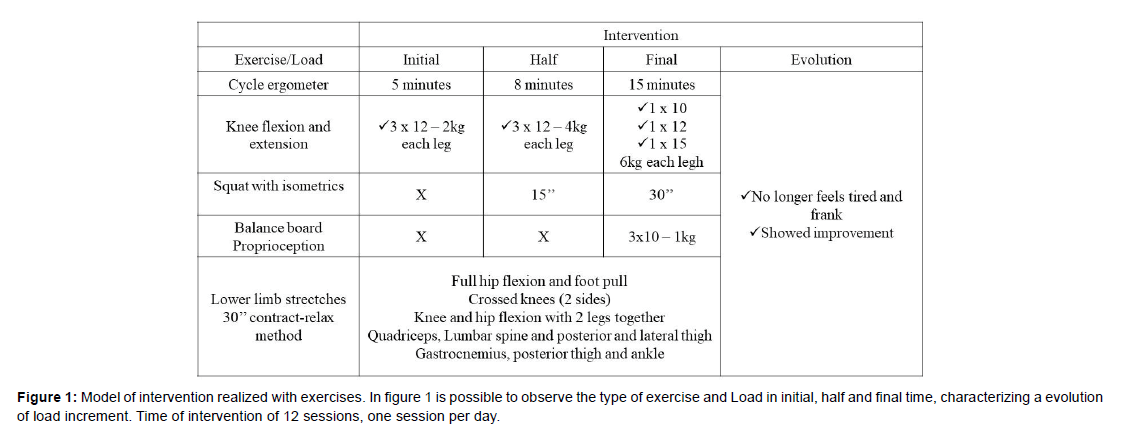
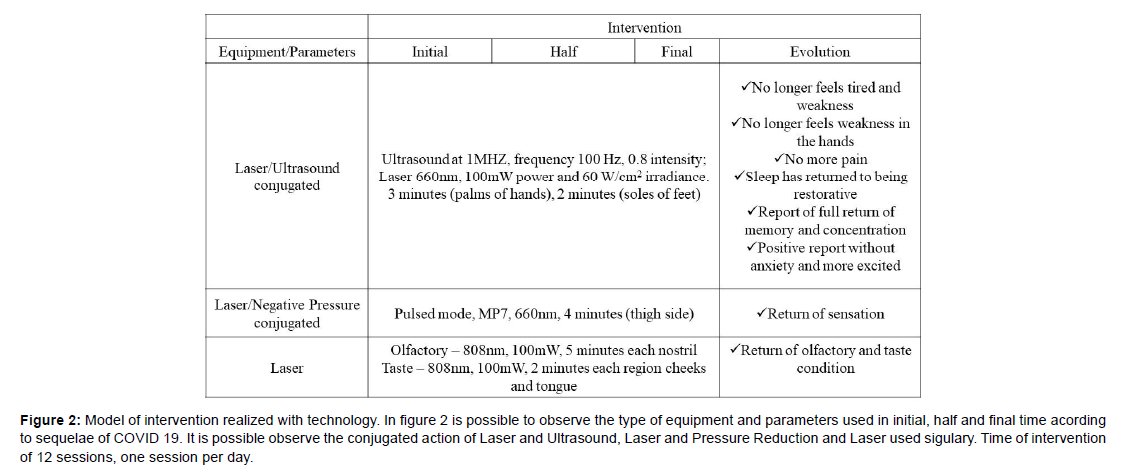
Patient male, 32 years old, Caucasian, physically active, nonsmoker, without comorbidities. He had initial symptoms of sore throat, headache, and fatigue. He was hospitalized for 27 days, of which 21 days in the intensive care unit and was intubated for 13 days. After hospital discharge, left leg without sensitivity, tiredness and weakness in the legs, pain in the left foot, weakness in the hands, difficulty and poor sleep quality, difficulty in memory and concentration, anxiety and depression, altered sense of direction and balance, smell and taste affected. The interventions below (Figures 1 and 2) were carried out in a 12-session intervention.
Figure 2: Model of intervention realized with technology. In figure 2 is possible to observe the type of equipment and parameters used in initial, half and final time acording to sequelae of COVID 19. It is possible observe the conjugated action of Laser and Ultrasound, Laser and Pressure Reduction and Laser used sigulary. Time of intervention of 12 sessions, one session per day.
Case 2
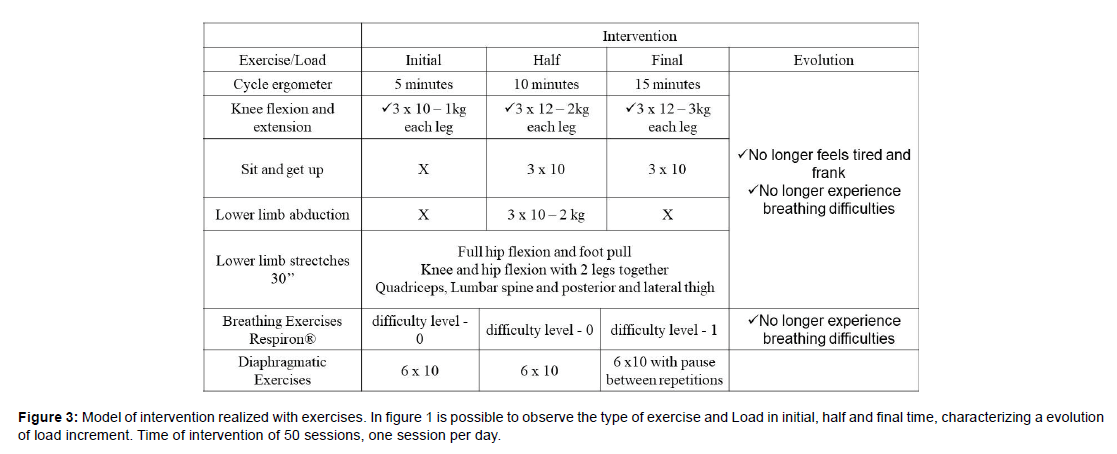
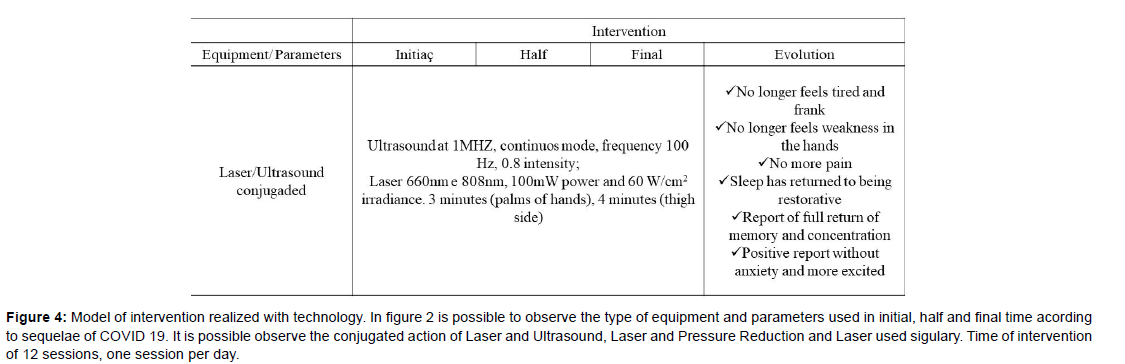
Female patient, 66 years old, Caucasian, physically inactive, nonsmoker, without comorbidities. He presented initial symptoms of lack of balance, pain in the legs, forgetfulness and word exchanges. He was hospitalized for 26 days, of which 11 days he was intubated. After hospital discharge, fatigue and weakness in the legs, pain in the biceps muscle when performing effort (in both arms), difficulty with memory were reported. The interventions below were carried out (Figures 3 and 4), in an intervention of 50 sessions.
Figure 4: Model of intervention realized with technology. In figure 2 is possible to observe the type of equipment and parameters used in initial, half and final time acording to sequelae of COVID 19. It is possible observe the conjugated action of Laser and Ultrasound, Laser and Pressure Reduction and Laser used sigulary. Time of intervention of 12 sessions, one session per day.
Case 3
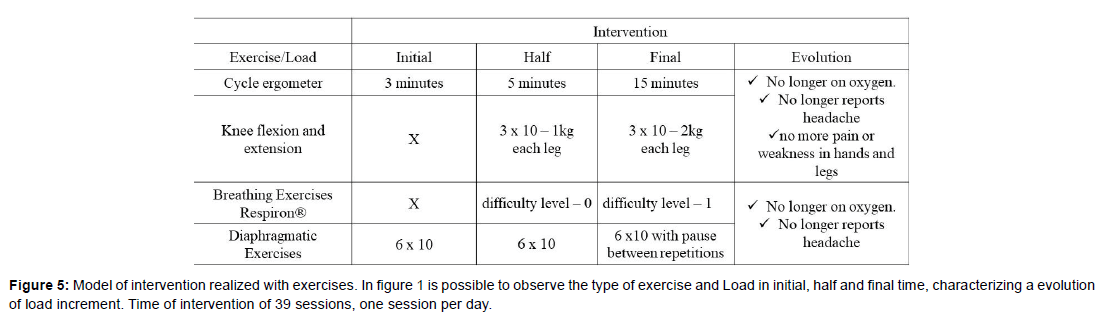
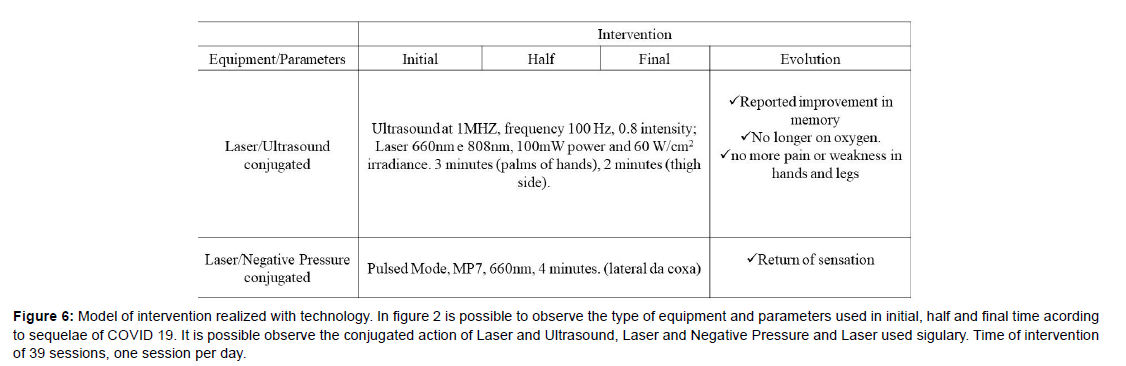
Female patient, 77 years old, Caucasian, physically inactive, nonsmoker, without comorbidities. He had no symptoms but was low on saturation. She was hospitalized for 8 days. After hospital discharge,fatigue, weakness, anxiety and depression were noted, as well as memory difficulties. The interventions below were carried out (Figures 5 and 6), in an intervention of 39 sessions.
Figure 6: Model of intervention realized with technology. In figure 2 is possible to observe the type of equipment and parameters used in initial, half and final time acording to sequelae of COVID 19. It is possible observe the conjugated action of Laser and Ultrasound, Laser and Negative Pressure and Laser used sigulary. Time of intervention of 39 sessions, one session per day.
Case 4
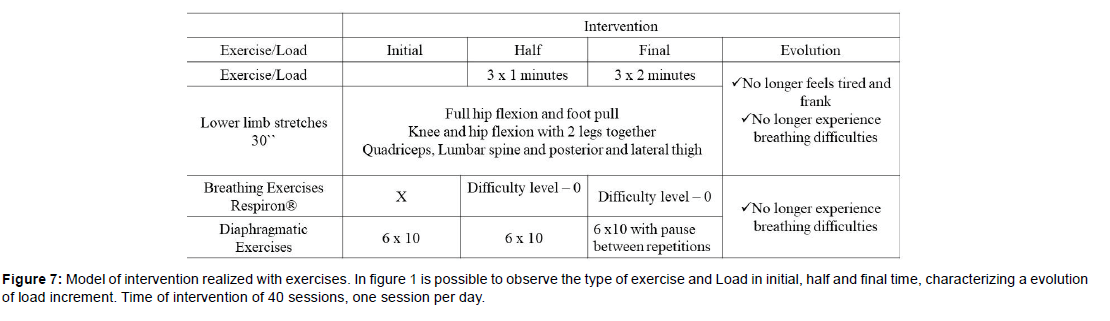
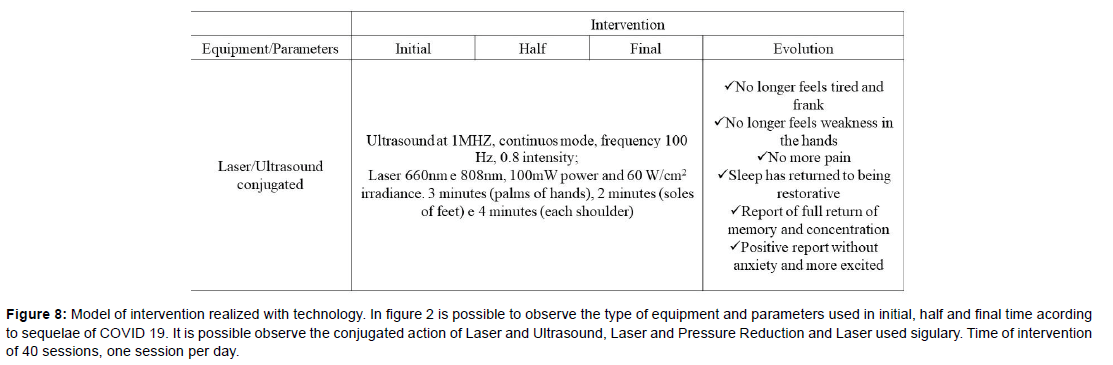
Female patient, 60 years old, Caucasian, physically inactive, smoker for 30 years, with daily consumption of 40 cigarettes. She has comorbidities such as hypertension, cardiomegaly, hypercholesterolemia, obesity, asthmatic bronchitis and chronic obstructive pulmonary disease (COPD). Patient reports that he was not hospitalized. He has leg pain, headache, memory difficulties, and poor sleep quality. The interventions below were carried out (Figures 7 and 8), in an intervention of 40 sessions.
Figure 8: Model of intervention realized with technology. In figure 2 is possible to observe the type of equipment and parameters used in initial, half and final time acording to sequelae of COVID 19. It is possible observe the conjugated action of Laser and Ultrasound, Laser and Pressure Reduction and Laser used sigulary. Time of intervention of 40 sessions, one session per day.
All patients underwent initial anamnesis and daily follow-up. A scale was used for taste and smell evolution. It is observed in the exercise loads presented in figures 1, 3, 5 and 7, the evolution of the work load throughout the performed intervention, being individualized for each case.
Results
Case 1
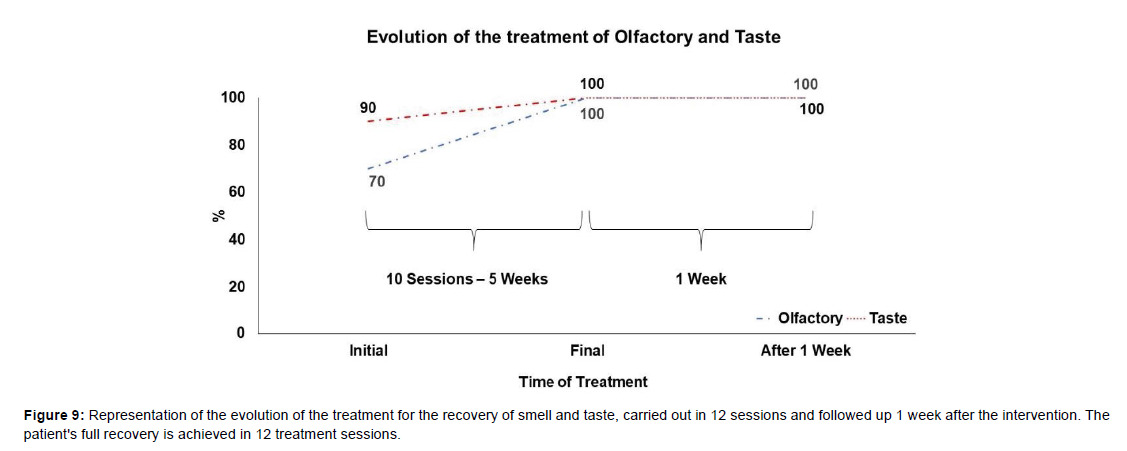
Figure 9 represents the evolution of the sensitivity of smell and taste after 12 sessions, together with case report 1. It is possible to observe that both sequelae are restored in the period of 12 sessions, maintaining 100% recovery after one week after surgery intervention.
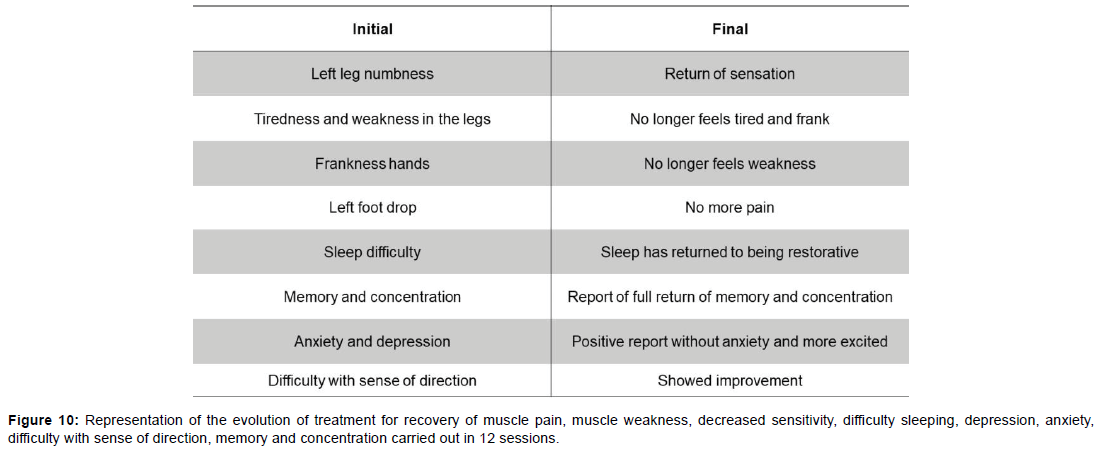
Figure 10 presents the initial assessment versus the final assessment of case 1, where the sequelae are shown (on the left) and their evolution (on the right).
Case 2
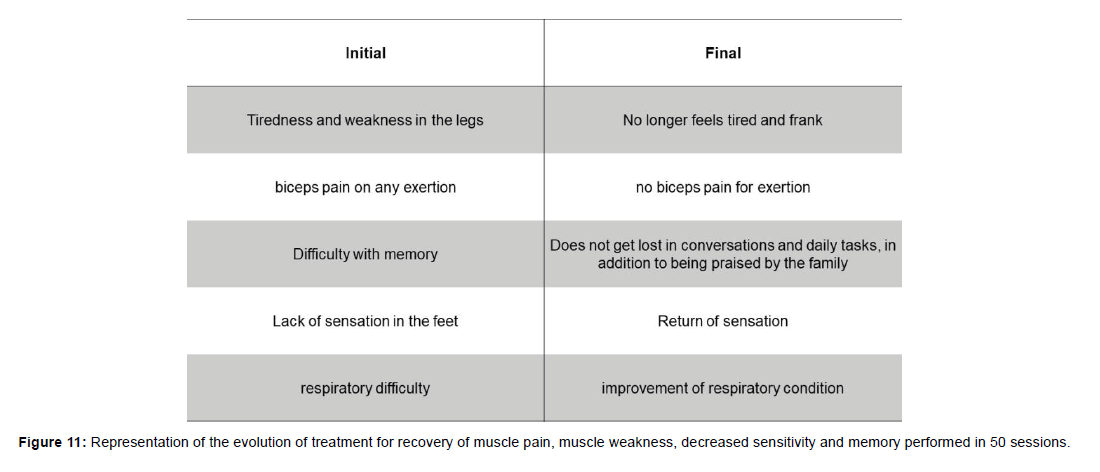
Figure 11 shows the initial assessment versus the final assessment of case 2, where the sequelae are observed (on the left) and their evolution (on the right).
Case 3
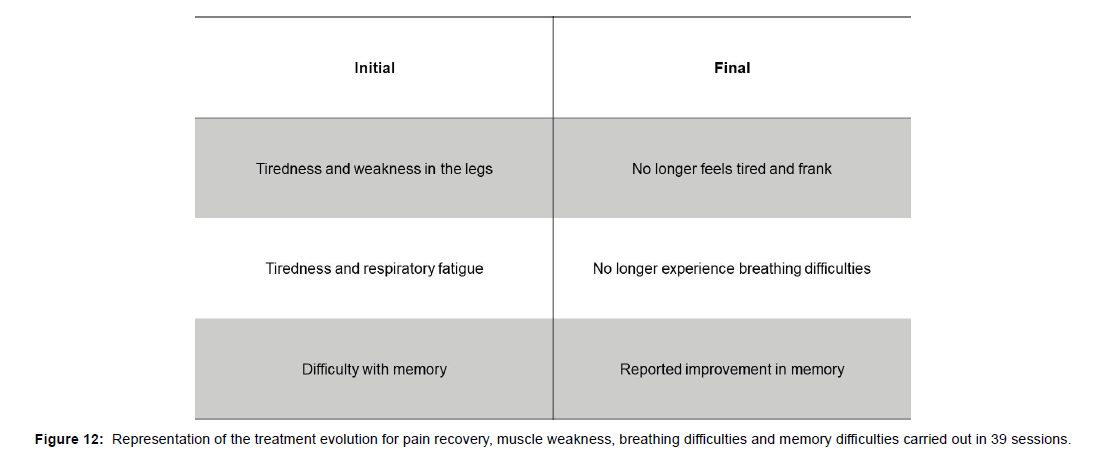
Figure 12 illustrates the initial assessment versus the final assessment of case 3, where the sequelae are pointed out (on the left) and their consequent evolution (on the right).
Case 4
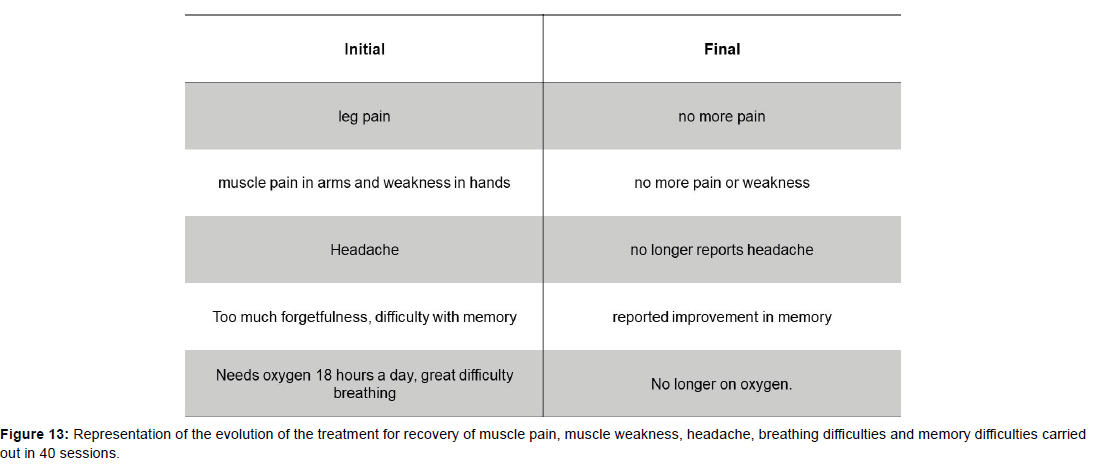
Figure 13 identifies the initial assessment versus the final assessment of case 3, where the sequelae are shown (on the left) and their substantial evolution (on the right).
Discussion
Since the beginning of the pandemic, new technologies have emerged with the aim of promoting rapid diagnosis of the disease. However, over time, sequelae emerged after SARS-COV-2 infection. These new technologies and methodologies are now also aimed at treating the sequelae from the post-infection syndrome, since they can compromise the most varied systems of the body. These technologies allow for the needs of the post-COVID syndrome such as inflammatory and painful diseases, acting directly on the systemic, respiratory, neuropsychic and musculoskeletal sequelae, seeking to face clinical decision-making more effectively combined with traditional rehabilitation treatment. Among these technologies, we can mention photobiomodulation, which has been shown to be efficient in the treatment of patients with anosmia and ageusia resulting from the post-COVID syndrome [20,21], as well as therapies combined with laser/negative pressure, and laser/ultrasound, promoting antiinflammatory effects anti-inflammatory, tissue repair, myofascial mobilization, in addition to sensorimotor stimulation, contributing to the improvement of the patient's clinical manifestations [14-19,22].
In this context, the synergy of resources such as laser/ultrasound and laser/vacum, allow a new non-invasive treatment approach, promising for the post Covid 19 syndrome. Low-intensity lasers produce red and infrared light, which are absorbed by structures lightsensitive, such as cytochrome C oxidase, a unit of the mitochondrial respiratory chain. This generates an increase in electron transport, mitochondrial membrane potential and adenosine triphosphate (ATP) production. Ion channels are photosensitive and, by absorbing photons, increase the concentration of intracellular calcium ions. These processes stimulate anti-inflammatory, immunomodulatory, analgesic and tissue repair effects [23]. Ultrasound, on the other hand, is another non-invasive therapeutic method in which the device is composed of piezoelectric crystals. It transforms electrical energy into oscillatory mechanical energy using high frequency alternating currents. Waves mechanically deform tissue molecules, leading to friction and heat production. These thermal and non-thermal effects induce biological responses such as muscle relaxation and, like low-level laser, tissue regeneration and reduced inflammation [24]. Negative pressure has the same mechanism as vacuum therapy, promoting tissue suction through high pressure. According to Furhad & Bukhari (2022) [25], the pressure difference causes an increase in the blood volume superficial to the skin and removal of interstitial fluid in the applied region, resulting in an anti-inflammatory, immunomodulatory effect, hematological adjustment and pain reduction [26].
However, the already established traditional rehabilitation becomes fundamental, outlining individualized interventions, meeting the conditions related to the patient's health, thus seeking functional independence, quality of life, alleviating disability, improving function and inclusion in social participation [27].
Thus, the results obtained in the treatment of sequelae related to the post-COVID 19 syndrome, such as the loss of neurosensory perception of smell and taste, systemic, respiratory, musculoskeletal changes, among others [20,21] are potentiated together with the established rehabilitation processes and the action of new combined and synergistic technologies that rehabilitate issues of healing, analgesia and inflammatory processes, both local and systemic [18,19,22,28].
Smell and Taste
The human organism has different types of sensations, including smell and taste [29]. The nasal cavity is lined by the respiratory and olfactory epithelium, where the detection of smell begins in the latter, formed by sustentacular cells, olfactory sensory neurons, microvillar cells, basal cells and cells of the olfactory glands, essential in the transmission of information to the region. olfactory function of the central nervous system [30]. Taste is detected by chemosensory receptors known as taste buds present on the tongue, which, when hit by food in the oral cavity, generate action potentials transporting the taste sensation to higher level cortical taste centers. The nasal epithelium [7] and the tongue taste buds [31] show high levels of ACE2 expression, however its physiological role in this region is not described in the literature. As reported by Hoffman et al. (2020) [32], Sars-CoV-2 employs the ACE2 receptor as a means of entry into the host cell, being a key determinant of the transmissibility of the virus. Therefore, it is characteristic that patients with post-COVID syndrome have anosmia and ageusia, which are considered neurological complications [33]. The presence of ACE2 receptors as high-affinity receptors with S1 proteins present in Sars-CoV-2, allows a process of fusion of the virus membrane with the membrane of the target cell [2]. Therefore, it can be said that the morphology of the cell membrane of this cell is altered. Our hypothesis establishes that, consequently, there will be conformational changes in cell membrane structures due to an inflammatory process triggered by the virus, which will affect sensory receptors responsible for smell and taste, which will not be able to perform their functions properly. The neural receptor cells of the nasal mucosa, olfactory bulb and lingual papillae, due to being inflamed, do not allow the entry of molecules from the air and food that are responsible for triggering the normal stimulus of smell and taste [34]. Physiologically, the cell seeks to reestablish these functions through gene transcription of new cell receptors, but because it is infected, its entire cellular metabolism is compromised as it is replicating the viral genetic material. The results presented in Figure 9 corroborate the hypothesis, which is reinforced by the fact that the use of photobiomodulation causes cell homeostasis [15], normalizing cell function. Thus, the recovery of sensations is potentiated.
Muscle and joint pain, Paresthesia and decreased sensation and Weakness in the upper and lower limbs
The infection caused by SARS-CoV-2 causes an imbalance in the Renin-Angiotensin-Aldosterone System, since the virus competes with ACE/ACE-2, causing a deregulation of the conversion of angiotensin II to angiotensin I (1-7) [35] , causing adverse effects on the reuptake of sodium, calcium and potassium ions in the intracellular and extracellular environment, decreasing the polarization of nerve fibers, making it impossible for the adequate conduction of nerve impulses to the tissues [36].
From this, the decrease in ion traffic in potassium ion channels, due to hypokalemia, causes muscle weakness, negatively influencing excitation-contraction in muscle cells, reducing the capacity for voluntary contraction36 as shown in figures 10,11,12 and 13 (left side). Myalgias are commonly reported in patients infected by COVID 19, as well as bone and joint disorders, which may appear as a result of the pro-inflammatory effects present in the viral infection, where cytokines and molecules that promote inflammatory signaling generated by the virus, promote pathological changes in the disease. musculoskeletal tissue which leads to the appearance of muscle and joint pain [37] as shown in figures 10,11,12,13 on the left side.
There is a binding of the Spike protein of the SARS-CoV-2 virus to the ACE 2 receptors, affecting the blood-brain barrier, directly reaching the brain and cerebrospinal fluid (CSF) and may occur through sensory and motor neuronal pathways causing demyelination and inflammatory effects [38,39], preventing coordinated electrical conduction, among which it causes paresthesia and hypoesthesia, symptoms present as in Guillain-Barré syndrome and Peripheral Neuropathy, correlated with COVID 19 infection. Both can be caused by peripheral nervous system (PNS) injuries that consequently inflammation of the nerves that generates a decrease in sensitivity, a sensation of numbness and tingling in the upper and lower limbs [21].
Based on this picture, photobiomodulation and conjugated therapies are punctual and effective in the treatment, as shown in figure 10, 11,12,13 (right side), allowing homeostasis of the clinical picture and consequent evolution of the patient. In this way, photobiomodulation acts on the stimulation of photoreceptors, mitochondria and on the production of adenosine triphosphate (ATP), generating an increase in cell multiplication, which promotes healing and analgesia at the application site. Furthermore, ultrasound, through the mechanical action of ultrasonic waves, allows for greater ionic permeability due to the cavitational effect, positively influencing the increase in nervous stimulation, when applied in conjunction with laser [16]. Vacuum therapy consists of the technique of suctioning the skin tissue in order to increase local blood flow, generating a greater concentration of oxygen and nutrients, stimulating anti-inflammatory and sensorimotor effects, demonstrating the effectiveness in the treatment of patients with symptoms arising from post Covid syndrome [21].
Difficulty sleeping, anxiety and depression, and memory and concentration
In this context, there is a complexity. Meiese et al. (2021) [40] reports that there are ACE2 receptors in the human brain, more specifically in neurons and glia cells, and Desforges (2014) [41] states that coronaviruses are neurotrophic and neuroinvasive pathogens, which explains the neurological manifestations in patients with severe infection by Sars-CoV-2 [42], generating the so-called “cytokine storm”. This storm is a phenomenon caused by the deregulation of the innate immune response in the body's defense process to fight COVID-19 [43] and results in neuroinflammation [44] and increased permeability of the blood-brain barrier, further favoring the entry of microorganisms into the Central Nervous System (CNS).
The blood-brain barrier has a neuroimmune function, controlling the release of cytokines, and because it is affected in the infection, the concentration of cytokines is even more deregulated in the CNS [45], causing an increase. Neuroinflammation causes severe damage to the CNS, such as dysregulation in the production of neurotransmitters, immunological alteration and neuroplasticity, as well as morphological changes in the brain [44].
In the midst of the installed inflammatory process [46], the presence of histamines (a pro-inflammatory agent) is a sleep suppressor, affecting serotonin. Sleep disorder is reported in several cases in patients infected by COVID 19 [47], and can be explained due to the decrease in the production of neurotransmitters, such as serotonin, and the increase in pro-inflammatory mediators, such as histamines. In the same sense, the increase in pro-inflammatory cytokines is directly correlated with the pathogenesis of depression and anxiety, as well as the concentration/ production of neurotransmitters [48], especially serotonin [49].
There is a citation [11] of two clinical cases of post-Covid patients with confirmed cognitive impairments, which also proved dysfunction of the anterior cingulate cortex and poster - both involved in emotions, depression, memory [50] and action decision, emphasizing that the hypometabolism presented in this brain region are common in cases of depression and Alzheimer's disease. Such hypometabolism may be linked to high levels of the neurotransmitter acetylcholine in the plasma of patients infected with Sars-CoV-2.
Thus, we enter into 3 hypotheses to explain memory changes in post Covid 19 syndrome:
1) ACE2 is responsible for the formation of Angiotensin 1-7 through two pathways: ACE2 directly converts Angiotensin II to Angiotensin 1-7 and converts from Angiotensin I to Angiotensin 1-9, which with the action of Angiotensin Converting Enzyme (ACE), is also converted to Angiotensin 1-7 [51]. Angiotensin 1-7 acts on muscarinic-type cholinergic receptors in various tissues, such as the brain [52]. The cholinergic system is directly related to memory formation, since Alzheimer's disease is related to the degeneration of the cholinergic system. In addition, therapies involving cholinesterase inhibitors, enzymes that degrade acetylcholine, show promise in the treatment of memory loss [53]. In this way, our hypothesis is supported that the physiological changes in the cholinergic system caused by Covid 19 directly influence memory loss;
2) The key to memory formation is adequate sleep, as neural reverberation takes place in REM sleep [54]. Furthermore, in the REM stage there are changes in neuronal activities, such as increases in acetylcholine levels [55]. Although the neuroinflammation caused by Sars-CoV-2 is responsible for the increase in acetylcholine in the body [40], the infection is also responsible for sleep disorders [47]. Therefore, our second hypothesis is that memory formation is affected in the post- Covid period due to these patients not having regulated sleep, with no neural reverberation in the REM stage.
3) The posterior cingulate cortex shows changes in Covid 19 [11], and has outputs to the hippocampus, responsible for the formation of memory and spatial notion [56]. Furthermore, memory is related to efficient synaptic transmission [57], neurotransmitter release and synaptic plasticity, all of which are affected by neuroinflammation as a consequence of Covid 19 [44]. Thus, our third hypothesis is that, by affecting the posterior cingulate cortex and, consequently, the hippocampus through neuroinflammation, Sars-cov-2 interferes with memory formation.
Sense of direction and balance
Hearing loss, tinnitus[58] and vertigo [59] are manifestations reported by patients with post-Covid syndrome. Studies show that cochlear outer hair cells undergo deleterious changes due to COVID-19 infection, which are important in sound transmission [58]. This explains the tinnitus reported by patients.
Due to the communication between the inner ear and the nasal cavity through the eustachian tube and the neurotropic characteristic of the coronavirus [41], it can be said that the virus has favorable mechanisms and means for ear infection. Depending on the site compromised during the infection, functions such as balance and hearing can be affected. Jeong et al (2021) [60] demonstrate that inner ear tissue co-expresses ACE2 receptors. Knowing that the method of cellular entry of the coronavirus is through Spike connection with the ACE2 receptor protein. When acting in this place, hearing is affected, and tinnitus may occur. In addition, balance (which happens because of the labyrinthine structure of the inner ear) is also affected. There are two possible causes of vertigo in post-Covid 19 [59] patients, which may relate to hearing loss. Sars-cov-2 can cause microcirculation problems, affecting the blood supply to the inner ear (labyrinth), which can lead to hearing loss. Labyrinthitis can be caused by neurological changes, such as focal axonal degeneration and loss of vestibular ganglion cells, which reinforces the neuroinflammation that is the cause of this pathology.
Our hypotheses are reported as improvements in sleep deficiency (Figure 10), anxiety (Figure 10), depression (Figure 10), memory loss (Figure 10, 11, 12 and 13), and loss of sense of direction (Figure 10), through the use of therapies combined with laser/ultrasound and laser/ negative pressure. Due to the mechanism of this therapy, we can say that it acts on homeostasis in the production of neurotransmitters, cell regeneration, inflammatory modulation in all the aforementioned regions affected by the post-Covid syndrome. Our hypothesis is that due to the application of conjugated laser/ultrasound therapy in the palms of the hands, there is an increase in ion permeability promoted by ultrasound, ATP production via photobiomodulation, in addition to the anti-inflammatory action of both resources. These stimuli are conducted by afferent pathways to the brain, where intracranial pressure is regulated [61], allowing greater regulation of brain activities. Also, there is greater cholinergic activity, allowing neuronal activity to be more active and the reverberation of stimuli for memory formation. Still, there is the occurrence of relaxation promoted by the stimuli, acting as a facilitating agent for sleep, enabling the REM sleep phase. Over time, the feelings of anxiety are overcome, reducing the level of depression gradually.
Breathing Difficulty
In the context of reduced sleep quality, COVID 19, as a neurotropic virus, has the neural pathways to enter the CNS as a gateway. After reaching the brain, it generates adverse reactions that in turn directly interfere with the stimulation of chemoreceptors present in the respiratory center. It is possible that there is a decrease in the ventilatory response of carbon dioxide (CO2) exerting an indirect effect on the chemosensitive area of the respiratory center located in the medulla, which have sensors that are sensitive to hydrogen ions (H+) [62]. The central chemoreceptors present in the spinal cord are responsible for most of the respiratory impulse, being able to verify the pH concentrations present in the central nervous system that can be caused by changes in the normality of carbon dioxide, in this way they respond to changes in pH by sending sensory stimuli to the CNS to stimulate breathing patterns [38].
There is an interaction between CO2 and water (H2O) reacting in carbonic acid (H2CO3), which there is a dissociation of ions of H+ and bicarbonate (HCO3-). From this, it is possible that H+ ions can cross the blood-brain barrier activating the respiratory center. Therefore, sleep deprivation, which can cause respiratory failure, can generate changes in partial pressure (PCO2) in the blood from the decrease in the sensitivity of central chemoreceptors [62].
Furthermore, alterations in the conduction of nerve impulses, especially in the vagus and glossopharyngeal nerves, due to the cholinergic alteration, may have a negative influence on respiratory stimuli, which begin in the vagus and glossopharyngeal nerves, present in the pons and medulla. In this way, the negative influence on the respiratory condition is established.
However, our intervention showed benefits in the respiratory rehabilitation of the cases (figures 11, 12 and 13), especially case 4, shown in figure 13, where the patient stopped using oxygen as support, even with the comorbidity of chronic obstructive pulmonary disease. (COPD). Our hypothesis, in addition to the essential function of the breathing exercises performed, is supported by the use of combined laser/ultrasound in the palms of the hands. This use, already performed in diseases such as fibromyalgia [16,61], promotes direct action on the brain, through the conduction of the stimulus through the afferent pathways. Thus, a cholinergic stimulation is performed, potentiating the respiratory action originating in the medulla and pons, enabling adequate inspirational stimulation via the vagus and glossopharyngeal nerves.
Conclusion
The constant work in the development of non-invasive and nondrug therapies, based on new technologies has allowed solid results to be obtained, allowing, together with the patient with post-COVID 19 sequelae, a full recovery. In this way, the consolidation of new technologies is presented at the moment of greatest need of humanity in the present times, allowing at the same time to reduce health costs and improve the quality of life of society.
Acknowledgement
This work was supported by São Paulo Research Foundation (FAPESP-grants nº2013/07276-1 and 2014/50857-8) and by National Council for Scientific and Technological Development (CNPq – grant nº465360/2014-9).
Conflict of Interest
The authors declare no conflict of interest.
References
- World Health Organization - WHO (2019) Coronavirus disease (COVID-19) pandemic.
- Jackson CB, Farzan M, Chen B, Choe H (2022) Mechanisms of SARS-CoV-2 entry into cells. Nat Rev Mol Cell Biol 23: 3-20.
- Shimohata T (2022) Neuro‐COVID‐19. Clin Exp Neuroimmunol 13: 17-23.
- Perez MM, Pimentel VE, Fuzo CA, da Silva-Neto PV, Toro DM, et al. (2022) Acetylcholine, Fatty Acids, and Lipid Mediators Are Linked to COVID-19 Severity. J Immunol 209: 250-261.
- Taljaard JJ, Conradie M, Coetzee A, Hugo SS, Dave JA, et al. (2020) Diabetes mellitus and COVID-19: A review and management guidance for South Africa. S Afr Med J 110: 761-766.
- Zheng YY, Ma YT, Zhang JY, Xie X (2020) COVID-19 and the cardiovascular system. Nat Rev Cardiol 17: 259-260.
- Zhang Y, Zheng L, Liu L, Zhao M, Xiao J, Zhao Q (2020) Liver impairment in COVID‐19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int 40: 2095-2103.
- Cheng Y, Luo R, Wang K, Zhang M, Wang Z, et al. (2020) Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int 97: 829-838.
- Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, et al. (2020) Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 87: 18-22.
- Mao L, Wang M, Chen S, He Q, Chang J, et al. (2020) Neurological Manifestations of Hospitalized Patients with COVID-19 in Wuhan, China: a retrospective case series study. 77: 683-690.
- Hugon J, Msika EF, Queneau M, Farid K, Paquet C (2022) Long COVID: cognitive complaints (brain fog) and dysfunction of the cingulate cortex. J Neurol 269: 44-46.
- Enwemeka CS, Parker JC, Dowdy DS, Harkness EE, Harkness LE, et al. (2004) Efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg 22: 323-329.
- Karu TI (2006) Mitochondrial mechanisms of photobiomodulation in context of new data about multiple roles of ATP. Photomed Laser Surg 28: 159-160.
- Tamae PE, Santos AVD, Simao MLD, Canelada ACN, Zampieri KR, et al. (2020) Can the associated use of negative pressure and laser therapy be a new and efficient treatment for Parkinson’s pain? A comparative study. J Alzheimers Dis Parkinsonism 10: 1-6.
- Simao ML, Fernandes AC, Ferreira KR, Oliveira LSD, Mario EG (2019) Comparison between the Singular Action and the Synergistic Action of Therapeutic Resources in the Treatment of Knee Osteoarthritis in Women: A Blind and Randomized Study. J Nov Physiother 9: 1-3.
- Carbinatto FM, Franco DM, Bruno JSA, Simao MLS (2020) The Laser and Ultrasound: The Ultra Laser like Efficient Treatment to Fibromyalgia by Palms of Hands–Comparative Study. J Nov Physiother 11: 1-5.
- Panhoca VH, Nogueira MS, Bagnato VS (2020) Treatment of facial nerve palsies with laser and endermotherapy: a report of two cases. Laser Phys 18: 15601.
- Canelada ACN, Carbinatto FM, Aquino Junior AED, Bagnato VS (2021) A Case Report on the use of a Conjugated System of Myofascial Release for Shoulder Capsulitis. J Nov Physiother 11: 1-4.
- Canelada Acn, de Aquino Junior AE, Carbinatto FM, Panhóca VH, Simão G, Zangotti L, Bagnato VS. (2022) The Synergy of Photobiomodulation and Myofascial Release in Upper Limb Injuries-Case Series. J Nov Physiother 12: 1-7.
- de Souza VB, Ferreira LT, Sene‐Fiorese M, Garcia V, Rodrigues TZ, et al. (2022) Photobiomodulation therapy for treatment olfactory and taste dysfunction COVID‐19‐related: A case report. J Biophotonics 15: 1-4.
- Dias LD, Blanco KC, de Faria CM, Dozza C, Zanchin EM, et al. (2022) Perspectives on photobiomodulation and combined light-based therapies for rehabilitation of patients after COVID-19 recovery. Laser Physics Letters 19: 1-9.
- Carbinatto FM, Aquino Junior AE, Coelho VHM, Bagnato VS (2018) Photonic technology for the treatments of venous and arterial ulcers: Case Report. Photodiagnosis and Photodyn Ther 22: 39-41.
- Nejatifard M, Asefi S, Jamali R, Hamblin MR, Fekrazad R (2021) Probable positive effects of the photobiomodulation as an adjunctive treatment in COVID-19: A systematic review. Cytokine 137: 1-9.
- Qing W, Shi X, Zhang Q, Peng L, He C (2021) Effect of therapeutic ultrasound for neck pain: a systematic review and meta-analysis. Arch Phys Med Rehabil 102: 2219-2230.
- Furhad S, Bokhari AA (2022) Cupping therapy. StatPearls Publishing.
- Hasbani GE, Jawad A, Uthman I (2021) Cupping (Hijama) in Rheumatic Diseases: The Evidence. Mediterr J Rheumatol 32: 316-323.
- Yan Z, Yang M, Lai CL (2021) Long COVID-19 syndrome: a comprehensive review of its effect on various organ systems and recommendation on rehabilitation plans. Biomedicines 9: 966.
- de aquino junior AE, Carbinatto FM, Bagnato VS (2021) Metabolic Rehabilitation: Body Homeostasis through the Action of Photobiomodulation in Weight Loss–A Comparative Study. J Obes Weight Loss Ther 11: 1-6.
- Shaikh FH, Soni A (2022) Physiology, Taste. StatPearls Publishing.
- Najafloo R, Majidi J, Asghari A, Aleemardani M, Kamrava SK, et al. (2021) Mechanism of Anosmia Caused by Symptoms of COVID-19 and Emerging Treatments. ACS Chem Neurosci 12:3795-3805.
- Park GC, Bang SY, Lee HW, Choi KU, Kim JM, et al. (2022) ACE2 and TMPRSS2 immunolocalization and oral manifestations of COVID-19. Oral Dis.
- Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, et al. (2020) SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically prove protease inhibitor. 181: 271-280.
- Khani E, Khiali S, Beheshtirouy S, Entezari-Maleki T (2021) Potential pharmacologic treatments for COVID-19 smell and taste loss: A comprehensive review. Eur J Pharmacol912: 174582.
- Rouadi PW, Idriss SA, Bousquet J (2021) Olfactory and taste dysfunctions in COVID-19. Curr Opin Allergy Clin Immunol 21: 229-244.
- Rivellese F, Predileto E (2020) ACE2 at the centre of COVID-19 from paucisymptomatic infections to severe pneumonia. Autoimmun Rev 19: 102536.
- Dixon RE, Navedo MF, Binder MD, Santana LF (2022) Mechanisms and physiological implications of cooperative gating of clustered ion channels. Physiol Rev 102: 1159-1210.
- Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, et al. (2020) Musculoskeletal consequences of COVID-19. J Bone Joint Surg Am 102: 1197-1204.
- Kumar S, Veldhuis, A, Malhotra T (2021) Neuropsychiatric and cognitive sequelae of COVID-19. Front Psychol 12: 577529.
- Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, et al. (2020) Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 87: 18-22.
- Maiese A, Manetti AC, Bosetti C, Del Duca F, La Russa R, et al. (2021) SARS-CoV-2 and the brain: A review of the current knowledge on neuropathology in COVID-19. Brain Pathol 31: 1-17.
- Desforges M, Le Coupanec A, Stodola JK, Meessen-Pinard M, Talbot PJ (2014) Human coronaviruses: viral and cellular factors involved in neuroinvasiveness and neuropathogenesis. Virus Res 194: 145-158.
- Hascup ER, Hascup KN (2020) Does SARS-CoV-2 infection cause chronic neurological complications? Geroscience 42: 1083-1087.
- Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LF (2020) The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol 20: 363-374.
- Serrano-Castro PJ, Estivill-Torrus G, Cabezudo-García P, Reyes-Bueno JA, Petersen NC, et al. (2020) Impact of SARS-CoV-2 infection on neurodegenerative and neuropsychiatric diseases: a delayed pandemic?. Neurologia 35: 245-251.
- Kurz C, Walker L, Rauchmann BS, Perneczky R (2022) Dysfunction of the blood-brain barrier in Alzheimer's disease: Evidence from human studies. Neuropathol Appl Neurobiol 48: 12782.
- Bollu PC, Kaur H (2019) Sleep Medicine: Insomnia and Sleep. Mo Med 116: 68-75.
- Sher Leo (2020) COVID-19, anxiety, sleep disturbances and suicide. Sleep Med 70: 124.
- Schou TM, Joca S, Wegener G, Bay-Richter C (2021) Psychiatric and neuropsychiatric sequelae of COVID-19–A systematic review. Brain Behav Immun 97: 328-348.
- Dell'osso L, Carmassi C, Mucci F, Marazziti D (2016) Depression, Serotonin and Tryptophan. Curr Pharm Des 22: 949-954.
- Pilotto A, Cristillo V, Cotti Piccinelli S, Zoppi N, Bonzi G, et al. (2021) Long-term neurological manifestations of COVID-19: prevalence and predictive factors. Neurol Sci 42: 4903-4907.
- Andone S, Bajko Z, Motataianu A, Maier S, Barcutean L, et al. (2022) Neuroprotection in Stroke-Focus on the Renin-Angiotensin System: A Systematic Review. Int J Mol Sci 23: 3876.
- Santos RAS, Sampaio WO, Alzamora AC, Motta-Santos D, Alenina N, et al. (2017) The ACE2/angiotensin-(1–7) /MAS axis of the renin-angiotensin system: focus on angiotensin-(1-7). Physiol Rev 98: 505-553.
- Hampel H, Marsel MM, Cuello AC, Farlow MR, Giacobini E, et al. (2018) The cholinergic system in the pathophysiology and treatment of Alzheimer’s disease. Brain 141: 1917-1933.
- Ribeiro S, Shi X, Engelhard M, Zhou Y, Zhang H, et al. (2007) Novel experience induces persistent sleep-dependet plasticity in the cortex but not in the hippocampus. Front Neurosci 1: 43-55.
- Fatma S, Anjum R (2020) Sleep: Physiology & its Concept in Unani Medicine. Int J Adv Res Innov Ideas Educ 6: 1321-1327.
- Lisman J, Buzsáki G, Eichenbaum H, Nadel L, Ranganath C, et al. (2017) Viewpoints: how the hippocampus contributes to memory, navigation and cognition. Nat Neurosci 20: 1434-1447.
- Jiao Y, Fan H, Wang K, Lu S (2019) Sevoflurane impairs short-term memory by affecting PSD-95 and AMPA receptor in the hippocampus of a mouse model. Behav Neurol.
- Chirakkal P, Al Hail AN, Zada N, Vijayakumar DS (2021) COVID-19 and Tinnitus. Ear Nose Throat J 100: 160-162.
- Maslovara S, Košec A (2021) Post-COVID-19 benign paroxysmal positional vertigo. Case Rep Med.
- Jeong M, Ocwieja KE, Han D, Wackym PA, Zhang Y, et al. (2021) Direct SARS-CoV-2 infection of the human inner ear may underlie COVID-19-associated audiovestibular dysfunction. Med Comum 1: 1-14.
- de Aquino Junior AE, Carbinatto FM, Rocha Tomaz CS, Bagnato VS (2022) Photosonic Treatment and Fibromyalgia: The Effect on Brain Compliance - Case Report. J Nov Physiother 12: 1-6.
- Adler D, Janssens J (2019) The pathophysiology of respiratory failure: control of breathing, respiratory load, and muscle capacity. Respiration 97: 93-104.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Junior AEA, Rodrigues TZ, Garcia V, Simão G, Carbinatto FM, et al. (2022) Conjugated and Synergistic Therapies in the treatment of Covid 19 Dysfunction - Pain, Weakness, Parestheria, Respiratory Condition, Memory, Olfactory and Taste: Case Series. J Nov Physiother 12: 545.
Copyright: © 2022 Junior AEA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3611
- [From(publication date): 0-2022 - Dec 03, 2025]
- Breakdown by view type
- HTML page views: 3087
- PDF downloads: 524