Review Article Open Access
Contribution of an Ultrasound Tissue Characterization on Fetal and Neonatal Health
Maeda K1*, Kihaile PE1, Ito T2, Utsu M2, SerizawaM3and YamamotoN21Department of Obstetrics and Gynaecology Tottori University Medical School, Yonago, Japan
2Department of Obstetrics and Gynaecology, Hakuai Hospital, Yonago, Japan
3Department of Obstetrics and Gynaecology, Hamamatsu Medical Centre, Hamamatsu, Japan
- *Corresponding Author:
- Maeda K
Department of Obstetrics and Gynaecology
Tottori University Medical School
Yonago, Japan
Tel: 81859226856
E-mail: maedak@mocha.ocn.ne.jp
Received date: September 26, 2015; Accepted date: September 28, 2016; Published date: September 30, 2016
Citation: Maeda K, Kihaile PE, Ito T, Utsu M, Serizawa M (2016) Contribution of an Ultrasound Tissue Characterization on Fetal and Neonatal Health. J Preg Child Health 3:286. doi:10.4172/2376-127X.1000286
Copyright: © 2016 Maeda K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Purpose: Objective ultrasonic B-mode image analysis in clinical ultrasound tissue characterization with echogenicity histogram in commercial B-mode devices. Materials: Placental intervillous space fibrin deposit, fetal growth restriction, malignant neoplasia, fetal brain echo density, fetal lung immaturity, meconium-stained amniotic fluid and adult liver. Methods: Commercial ultrasound B-mode histogram base width of a phantom divided by the full gray scale length was constant controlling B-mode gain; it was called gray level histogram width (GLHW) and used to tissue characterization. Image contrast should be lowest. Results: Fibrin deposit in placental intervillous space was diagnosed and treated with heparin to obtain normal neonate. Ovarian, cervical and endometrial malignancies were higher than 50% in GLHW. Fetal brain echo density and fetal lung immaturity were diagnosed. Meconium stained amniotic fluid GLHW was high. Adult liver GLHW will be studied in the future. Helsinki declaration was followed in the studies. Conclusion: The GLHW objectively diagnosed ultrasound B-mode image; thus, it should be widely used even in adult using commercial B-mode device.
Keywords
Ultrasound B-mode; GLHW; Tissue characterization; Placenta; FGR; Fibrin deposit; Malignancy; PVE; PVL; CP; Fetal lung; RDS; Adult liver
Introduction
Although ultrasound B-mode image was superb diagnostic tool, objective tissue characterization was desired. However, particular computer and program were mandatory [1]. The tissue characterization with ultrasound B-mode gray-level histogram width (GLHW) achieved clinical method of ultrasound tissue diagnosis.
Methods
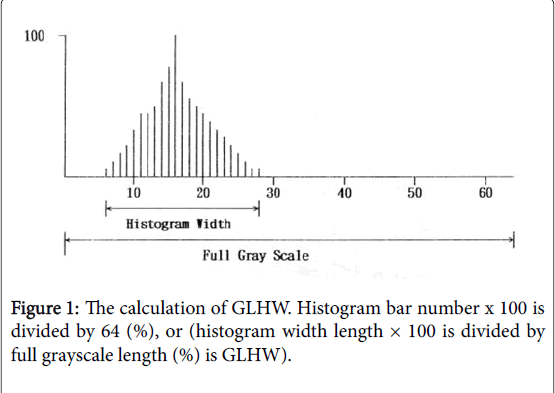
The clinical tissue characterization was the gray level histogram width divided by full gray level length (Figure 1) [2,3] and it was called gray level histogram width (GLHW) which was standardized by the study of RMI 412 ultrasound phantom (Radiation Measurement Inc. Middleton, Wisconsin). The phantom histogram width did not change when the B-mode device gain changed, while image contrast had to be lowest, because histogram width was enlarged when the image contrast was high. The GLHW of RMI 412 phantom was standardized, and confirmed in various Aloka machines (Aloka, Tokyo) and Voluson 530D (GE Healthwear). The GLHW was manually calculated, and also automatically calculated by “%W” index in the histogram of Aloka Bmode devices, where the value was the same as manual determination [3].
Materials and Results
Fibrin deposit in intervillous space treated by maternal heparin administration
GLHW of 1 cm2 region of interest (ROI) of placental image was manually determined in every 2 gestational weeks in 20 to 41 weeks of normal pregnancies, where mean ± 1.5 SD of GLHW were determined. The GLHW was larger in grade 3 placenta than normal placenta [3] (Figure 1).
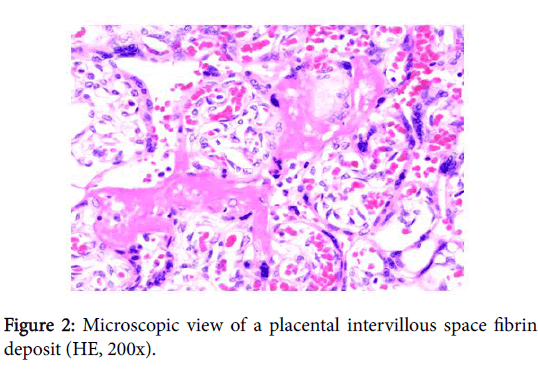
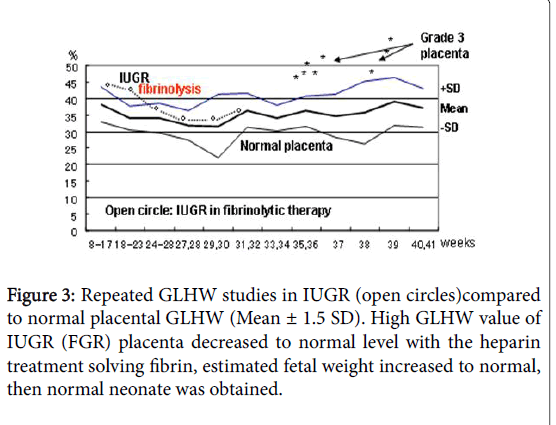
Placental GLHW of a case of IUGR (fetal growth restriction, FGR) was larger than that of normal placenta and diagnosed by Utsu to be intervillous space fibrin deposit (Figure 2) in a pregnant woman of positive cardiolipin antigen, and daily 5000 unit heparin was administered repeatedly to the woman. The GLHW decreased, estimated fetal weight increased to normal, and normal neonate was obtained (Figure 3), despite an FGR fetus died in previous pregnancy of the mother in the present study [3].
The deposited fibrin would reduce placental active transfer of fetal nourishing material developing FGR, and further damaged passive transfer of oxygen causing fetal hypoxia and demise in previous pregnancy. Heparin solved deposited fibrin increasing maternal blood flow in the intervillous space to promote placental transfer function then treated FGR and fetal hypoxia preventing fetal demise due to hypoxia (Figure 3).
Fetal brain periventricular echo density
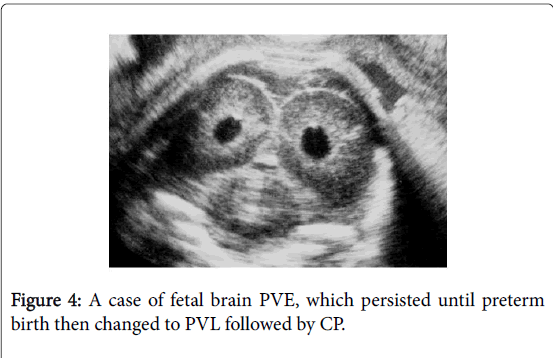
Yamamoto et al. [4] studied fetal brain in preterm pregnancy detecting periventricular echo density (PVE) (Figure 4), of which 18% (corresponding 0.2% of all births) preceded neonatal periventricular leukomalacia (PVL) followed by cerebral palsy (CP), if the PVE lasted until preterm birth, while there was no neonatal PVL when the PVE disappeared before birth. Also, no PVE developed in full-term births’ neonates. The GLHW of fetal brain PVE was 36 ± 5% which was significantly larger than 23 ± 5% of normal fetal brain GLHW [4], thus, GLHW is useful to detect fetal and neonatal brain PVE for the prevention of neonatal PVL and CP, namely, the PVE ultrasonically detected immediately after a preterm birth will be treated with various medicines, e.g. growth factor, erythropoietin, hydrocortisone, in the future.
Diagnosis of immature fetal lung
Fetal lung maturity should be detected prior to preterm birth to treat the neonate with artificial surfactant to prevent respiratory distress syndrome (RDS). Since the amniocentesis to chemically analyze amniotic fluid for the detection of fetal lung immaturity is invasive at present, non-invasive ultrasonic tissue characterization of immature fetal lung has been studied by Serizawa [5-7].
GLHW values of fetal lung declined in immature fetal lung, while fetal liiver GLHW was constant, the ratio of fetal lung GLHW and fetal liver GLHW was studied and fetal lung was immature in young fetus, therefore, the gestational weeks multiplied by the ratio of fetal lung to liver ratio was less than 29, which was the critical level to differentiate immature from mature fetal lung, namely, 96% of neonatal respiratory distress syndrome (RDS) was predicted when the GLHW ratio of fetal lung to liver ratio multiplied by gestational weeks was lower than 29. The detection rate was highest among various RDS detection parameters. The preterm pregnancy management, e.g. maternal steroid administration will be monitored by repeated non-invasive GLHW studies. Neonatal surfactant therapy is prepared or fetal steroid therapy will be repeated, if the fetal lung is still immature with GLHW study [6].
Diagnosis of meconium stained amniotic fluid
As amniotic fluid is stained by meconium, when fetal stool is released into amniotic fluid in fetal asphyxia. The condition is diagnosed with amnioscopy by Saling in 1950s before fetal heart rate monitoring. As the amniotic fluid was stained yellowish dirty, by meconium expelled from relaxed fetal anal ring muscle in asphyxia, amniotic fluid GLHW was expected to be higher than clear fluid, and the GLHW was similar to that of fetal colon in meconium stained fluid. Results were confirmed by Yamamoto [7], where normal fluid GLHW was 6.7 ± 2.0%, Colon 9.5 ± 2.3% and meconium stained fluid 11.0 ± 3.6%, significant difference was present between meconiumstained and normal fluid, while the difference was insignificant between colon and meconium-stained fluid, and significant difference between colon and normal fluid. Meconium stained fluid will be diagnosed by ultrasound GLHW, namely, fetal asphyxia will be detected by GLHW of amniotic fluid.
Diagnosis of malignancy
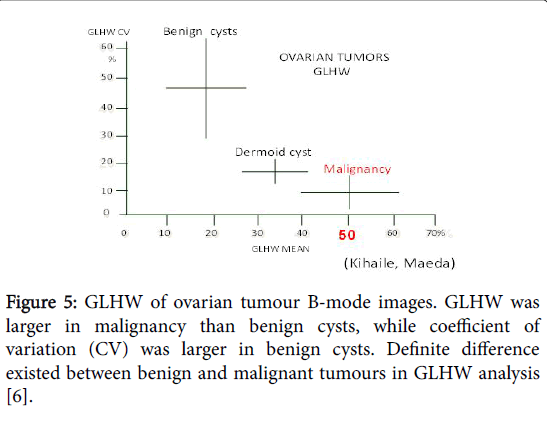
GLHW in preoperative ovarian masses were compared to postoperative pathology [4], where mean GLHW was 18 ± 10% in benign masses, while it was 51 ± 11% in malignancy, i.e., mean GLHW values were larger in malignant masses than benign tumors (Figure 2) [4], therefore, ovarian malignant neoplasia is diagnosed by GLHW. Ovarian dermoid cyst was intermediate between benign and malignant masses; however, a dermoid cyst is diagnosed by its characteristic niveau image in B-mode.
In other studies, mean GLHW was 42.7 ± 5.0% in normal endometrium, while it was 58.2 ± 11.2% in endometrial cancer, thus, endometrial cancer will be diagnosed by GLHW [5,6]. As the author found that the GLHW of a uterine cervical cancer was higher than 50%, general malignancy will be indicated by GLHW higher than 50%.
Nam et al. [7-11] reported differentiation of malignant and benign thyroid nodules using histogram analysis of gray scale sonograms. Ultrasonic B-mode histogram diagnosis of malignancy was supported also by the report (Figure 5).
GLHW of healthy adult liver
Mean GLHW of 33 healthy adult livers was 34.8 ± 3.7%, where the coefficient of variation was 10.5% and no relation of GLHW was noted to the age or gender [3]. Any pathological state of adult liver will be studied in the future using GLHW.
Conclusion
Gray level histogram width (GLHW) is update clinical ultrasound tissue characterization calculated from ultrasound B-mode echogenicity histogram parameter in commercial B-mode imaging device. Placental intervillous space fibrin deposit, malignant neoplasia, fetal brain periventricular echogenesity, immature fetal lung, meconium-stained amniotic fluid and normal adult liver were studied, where GLHW was useful non-invasive clinical tissue characterization using commercial B-mode devices.
References
- Akaiwa A (1989) Ultrasonic attenuation character estimated from backscattered radiofrequency signals in obstetrics and gynaecology. YonagoActaMedica 32: 1-10.
- Maeda K, Akaiwa A, Kihaile PE (1993) Ultrasound tissue characterization, ultrasound in obstetrics and gynaecology. Little Braun Boston,pp: 55-59.
- Maeda K, Utsu M, Kihaile PE (1998) Quantification of sonographic echogenicity with grey-level histogram width. A clinical tissue characterization. Ultrasound Med &Biol 24: 225-234.
- Yamamoto N, Utsu M, Serizawa M, Ohki S, Murakoshi T, et al. (2000) Neonatal eriventricularleukomalacia preceded by fetal periventricular echodensity. FetalDiagTher 15: 198-208.
- Maeda K, Serizawa M (1999) Echogenicity of fetal lung and liver quantified by the gray-level histogram width, Ultrasound. Med Biol 25: 201-206.
- Serizawa M, Maeda K (2010) Non-invasive fetal lung maturity prediction based on ultrasonic gray level histogram width. Ultrasound Med Biol 36: 1998-2003.
- Maeda K, Serizawa M, Yamamoto N (2005) Ultrasound tissue characterization with the gray level histogram width of the B-mode. Ultrasound Rev ObstetGynecol 5: 92-95.
- Kihaile PE (1989) Ultrasonic tissue characterization of ovarian tumors by the scanning of grey-level histograms. YonagoActaMedica 31: 75-82.
- Maeda K, Utsu M, Yamamoto N, Ito T (2002) Clinical tissue characterization with gray level histogram width in obstetrics and gynecology. Ultrasound Rev ObstetGynecol 2: 124-128.
- Ito T (2007) Diagnosis of endometrial cancer with GLHW tissue characterization. Personal communication.
- Nam, SJ, Yoo J, Lee HS, Kim EK, Moon HJ, et al. (2016) Quantitative evaluation for differentiating malignant and benign thyroid nodules using histogram analysis of grayscale sonograms. J Ultrasound Med 35: 775-782.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11579
- [From(publication date):
October-2016 - Aug 28, 2025] - Breakdown by view type
- HTML page views : 10526
- PDF downloads : 1053