Case Report Open Access
Cyroglobulinemia in Chronic Hepatitis B Infection with Undetectable Viral Load
Adham M. Osman1*, Stacey Honda1, Karen Ching1 and Michael Sharrak2
1Kaiser Permanente, Hawaii Residency Program, Internal Medicine, Honolulu, Hawaii, USA
2University of Medicine and Health Sciences, Federation of Saint Kitts and Nevis
- *Corresponding Author:
- Adham Osman
Kaiser Permanente, Hawaii Residency Program
Internal Medicine, Honolulu, Hawaii, USA
Tel: (808)-425-2540
E-mail: Adham.M.Osman@kp.org
Received date: July 28, 2017; Accepted date: August 16, 2017; Published date: August 21, 2017
Citation: Osman MA, Honda S, Ching K, Sharrak M (2017) Cyroglobulinemia in Chronic Hepatitis B Infection with Undetectable Viral Load. J Clin Infect Dis Pract 2:119. doi:10.4172/2476-213X.1000119
Copyright: © 2017 Osman AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical Infectious Diseases & Practice
Abstract
A 53 year old woman with history of chronic hepatitis B presents with palpable purpura of the lower extremities and recurrent hematuria. She was found to have elevated creatinine (1.4 mg/dl increased from her baseline of 0.8 mg/dl) and proteinuria (6.8 mg/dl). Renal biopsy revealed membranoproliferative glomerulonephritis and epidermal biopsy revealed leukocytoclastic vasculitis. Serum cryoglobulin precipitate was positive and Hepatitis B viral load was initially undetectable as the sample was allowed to cool to room temperature. A repeat sample was retested while keeping the serum above 37°C, this time the viral load was found to be elevated at 361 copies/ml. Both antiviral (entecavir) and immunosuppressive therapy (cyclophosphamide and prednisone) were initiated and the patient’s skin and renal manifestations improved rapidly. Proper communication between the clinician and laboratory is essential to ensure an accurate diagnosis in the context of cryoglobulinemic vasculitis.
Keywords
Vasculitis; Hepatitis; Infection
Background
The skin and kidneys are some of the most commonly affected organs in mixed cryoglobulinemic vasculitis. Most cases of cryoglobulinemic vasculitis are caused by hepatitis C and have only rarely been associated with hepatitis B [1,2]. Precipitation of cryoglobulins may lead to decreased viral load from aggregation of immunoglobulin G (IGG) and immune globulin M (IGM) complexes making cryoglobulinemia within the setting of chronic hepatitis B infection a diagnostic challenge [3,4].
We present this case in order to illustrate a rare cause of cryoglobulinemic vasculitis and to emphasize the importance of proper handling of cryoglobulin samples. Hepatitis B is often overlooked as a potential cause of cryoglobulinemia. In general there is often a lack of communication between the clinician and laboratory within the context of proper handling of potential cryoglobulin samples. In our case, the initial serum sample was collected routinely and allowed to cool to room temperature (less than 37°C) leading to precipitation of cryoglobulins and aggregation of hepatitis B antigen within these complexes. This resulted in a falsely low viral load and delay in effective treatment (anti-viral therapy with entecavir). Early recognition by the clinician and communication to the lab, of the possibility of a cryoglobulin sample, would to a standard protocol that would keep the serum sample above 37°C.
Case Presentation
A 53 year old woman with history of chronic hepatitis B presented to Kaiser Moanalua ER with palpable purpura of the lower extremities and recurrent hematuria. She had recently been treated in the outpatient clinic for a urinary tract infection and was treated with a 3 day course of ciprofloxacin 4 weeks earlier. At that time the patient was noted to have 0-3 RBC/HPF on urinalysis which was attributed to infection. On current presentation, examination showed a coalescing palpable purpuric rash on the lower extremities up to the mid tibia, no costovertebral, abdominal or suprapubic tenderness was noted. General examination was otherwise unremarkable and she was found to have 10-50 RBC//HPF.
Investigations
Hematologic investigations showed a hemoglobin of 9.0 g/dl down from her baseline of 10.0 g/dl. Creatinine was elevated to 1.4 mg/dl increased from her baseline of 0.8 mg/dl.
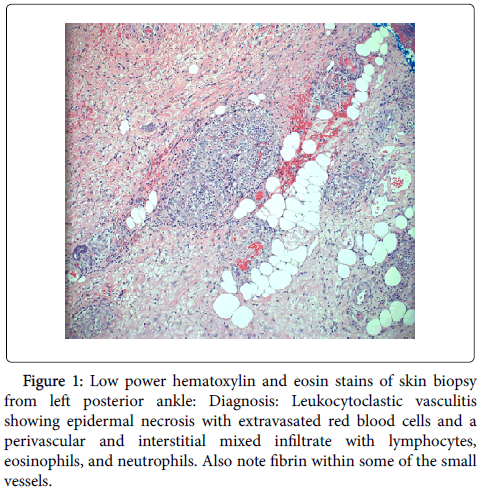
Epidermal biopsy demonstrated a leukocytoclastic vasculitis. Hematoxylin and eosin (H and E) staining showed epidermal necrosis with extravasated red blood cells and a perivascular and interstitial mixed infiltrate with lymphocytes, eosinophils, and neutrophils (Figure 1).
Figure 1: Low power hematoxylin and eosin stains of skin biopsy from left posterior ankle: Diagnosis: Leukocytoclastic vasculitis showing epidermal necrosis with extravasated red blood cells and a perivascular and interstitial mixed infiltrate with lymphocytes, eosinophils, and neutrophils. Also note fibrin within some of the small vessels.
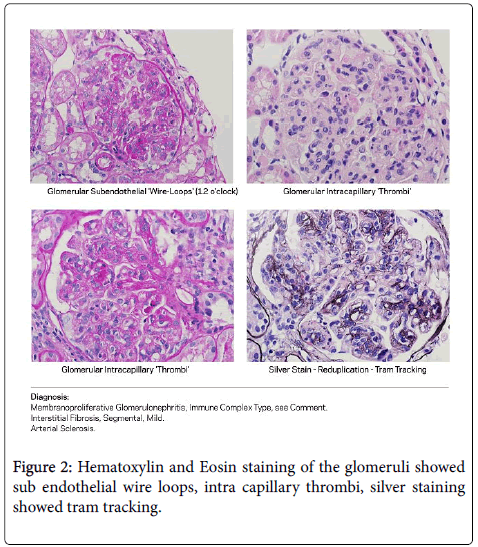
Renal biopsy demonstrated membranoproliferative glomerulonephritis with cryoglobulins. H and E staining of the glomeruli showed sub endothelial wire loops, intra capillary thrombi, silver staining showed tram tracking (Figure 2).
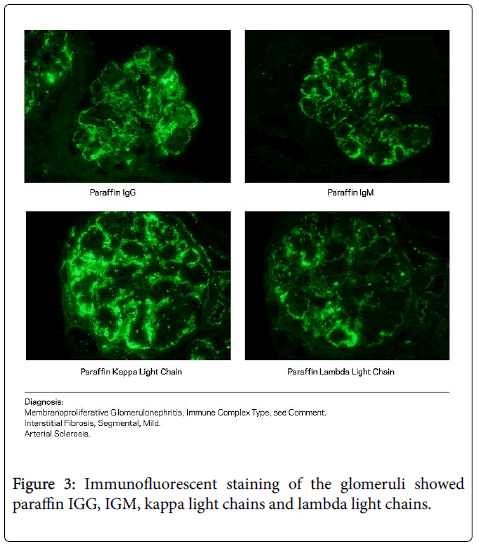
Immunofluorescent staining of the glomeruli showed paraffin IGG, IGM, kappa light chains and lambda light chains (Figure 3). Initially her hepatitis B viral load was undetectable. On repeat testing, the serum sample was kept above 37°C and demonstrated an elevated viral load of 361 copies/ml.
Differential Diagnosis
Both the renal and epidermal biopsies revealed cryoglobulin accumulation in the small vessels. The differential diagnosis for small vessel cryoglobulinemic vasculitis includes infection, autoimmune, hypersensitivity, IGA and anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis [2]. In our case, the precipitant of the cryoglobulinemia was initially unclear.
Hypersensitivity vasculitis was considered as our patient had a recent urinary tract infection and was given a course of ciprofloxacin. Fluoroquinolones have been shown to cause a delayed onset maculopapular non pruritic rash in 2-3% of patients though this typically occurs within 10 days of taking the drug and there does not appear to be renal involvement in this process [3]. Autoimmune etiology was considered though ANCA, double-stranded DNA, rheumatoid factor (RF) and cyclic citrullinated peptide were negative. Serum IGA levels were normal and ANCA was negative.
Our patient was known to have chronic hepatitis B though initially the viral load was found to be undetectable as the sample was allowed to cool to room temperature. Previous case report by Pasquet et al. 2012 has shown low viral loads in the setting of hepatitis B infection due to accumulation of viral particles within cryoglobulinemic complexes [4]. Serum from our patient was kept from precipitating by keeping the sample in a thermos that kept the temperature above 37°C. The viral load was then found to be elevated at 361 copies/ml. While hepatitis B is a rare cause of cryoglobulinemic vasculitis, it should be considered in the presence of small vessel cryoglobulinemic vasculitis and samples should be handled as above.
Treatment
Our patient was started on entecavir 0.25 mg daily due to reduced glomerular filtration rate along with cyclophosphamide 1150 mg one dose and prednisone 60 mg daily.
Outcome and Follow up
Within 6 weeks, the hepatitis B viremia decreased below the limit of detection. Our patient’s renal function improved with creatinine returning to baseline within 2 weeks (1.5 to 0.8 mg/dl) and proteinuria nearly resolved within 6 months (6.8 to 0.4 mg/dl). Her purpuric rash resolved within four weeks after initiating therapy. No residual scarring occurred.
1 year following hospitalization, the patient has had no further exacerbations of hepatitis B, her renal function remains at baseline and no further skin manifestations have arisen. She remains on daily entecavir.
Discussion
Cryoglobulins are composed of immunoglobulins and complement components and will precipitate upon cooling of serum and plasma, typically at temperatures below 37°C. Several different types of cryoglobulins have been identified with variable presentations and can affect the kidneys, skin, nerves, lungs, muscles and joints among other organ systems. Three types of cryoglobulinemia are recognized, according to the composition of precipitated immunoglobulin complexes. In type I, a monoclonal immunoglobulin is identified, typically IGM though less frequently IGG, IGA or light chains. Types II and III are known as mixed cryoglobulins. These types contain rheumatoid factors which are typically IGM though less likely IGG or IGA. The rheumatoid factors will form complexes with the fragment crystallizable (fc) portion of the IGG. In type II, the rheumatoid factor may be monoclonal while type III is polyclonal [5].
Treatment of cryoglobulinemia involves reversal of the underlying process, in our case with anti-viral therapy. No current guidelines exist for the treatment of hepatitis B related cryoglobulinemic vasculitis. In the absence of a clear viral etiology, corticosteroids, immunosuppressive drugs and plasma exchange are the standard of care for treatment of this disease process [6].
There have been 2 well known case studies in which hepatitis B associated cryoglobulinemic vasculitis was successfully treated with entecavir therapy [6,7]. One reported a 57 year old woman with a purpuric rash on her legs. She was found to have elevated transaminases with aspartate aminotransferase (AST) 143 IU/ml, alanine aminotransferase (ALT) 119 IU/ml, gamma-glutamyl transferase (GGT) 27 IU/ml and total bilirubin 29.1 mg/dl. Her hepatitis B DNA level was 448,551 copies/mL. Entecavir was initiated at 0.5 mg/day. Serum hepatitis B DNA level decreased immediately and became undetectable by week 6. Her aminotransferases normalized within 12 weeks [7]. A second case report described a 40 year old woman presenting with cryoglobulinemic vasculitis with multiple organ involvement including liver, kidney and skin with hemolytic anemia and autoimmune thyroiditis. Hepatitis B viral load was 2,185,500 copies/ml, ALT 178 IU/L, total bilirubin 1.40 mg/dl, thyroid stimulating hormone (TSH) 7 μIU/mL, hemoglobin 10.0 g/dL and creatinine 1.77 mg/dl. Entecavir was initiated at 0.25 mg every 72 hours due to reduced glomerular filtration rate. Her transaminases and renal function including proteinuria improved within 4 weeks from discharge. Her hepatitis B DNA viral load became undetectable after 5 months [6].
Other cases of hepatitis B related cryoglobulinemia have responded to lamivudine and adefovir dipivoxil. A case of a patient treated with the former resulted in recurrence of hepatitis B infection and cryoglobulinemia due to occurrence of lamivudine resistant hepatitis B. The patient was then treated with adefovir and recovered [7].
Interferon alpha is used for treating chronic hepatitis B infection though it has not been shown to be as effective in treating extra hepatic manifestations of hepatitis B vasculitis [7]. Interferon alpha has immunomodulatory activity and facilitates rapid viral suppression in only a minority of patients.
Though no official guidelines currently exist, entecavir is often used first line in hepatitis B associated cryoglobulinemic vasculitis. Entevacir has been shown to be more effective than lamivudine in randomized controlled trials [6,7].
It is not practical or possible to handle all serum as potential cryoglobulin samples. The key in our clinical case is to recognize Hepatitis B as a possible cause of cryoglobulinemic vasculitis. Early recognition of a potential cryoglobulinemia, early communication to the lab to handle serum samples above 37°C, and early therapy will lead to effective management of this patient population. As more cases of hepatitis B associated cryoglobulinemic vasculitis arise in the literature, definitive guidelines for treatment of this phenomenon may aid clinicians and lead to better outcomes in patients with this disease.
Learning Points
Hepatitis B can be a cause of small vessel cryoglobulinemic vasculitis. Entecavir can be considered first line therapy in the treatment of extra hepatic effects of chronic hepatitis B infection including small vessel cryoglobulinemic vasculitis. Hepatitis B viral load may be falsely low due to precipitation of antigens in the cryoglobulin complexes.
When handling serum containing cryoglobulins, it is necessary to keep the sample above 37°C. Early clinical detection of possible cryoglobulin samples and communication with the lab to facilitate proper handling of the specimen are essential in minimizing diagnostic error or delays in treatment.
References
- Ferri C (2008) Mixed cryoglobulinemia. J Rare Dis 3: 25.
- Ghetie D, Mehraban N, Cailin H, Sibley M (2014) Cold Hard Facts of Cryoglobulinemia. Rhe Dis Clini 41: 93-108.
- Schmid D, Depta J, Pichler W (2005) T cell-mediated hypersensitivity to quinolones: mechanisms and cross-reactivity. Clini Expr Allr 36: 59-69.
- Pasquet F, Combarnous F, MacGregor B, Coppere B, Mausservey C, et al. (2012) Safety and efficacy of rituximab treatment for vasculitis in hepatitis B virus-associated type II cryoglobulinemia: a case report. J Med Case Reports 6: 39.
- Ramos-Casals M, Stone J, Cid M, Bosch X (2012) The cryoglobulinemias. Lancet 379: 348-360
- Vigano M, Martin P, Cappelletti M, Fabrizi F (2014) HBV-associated cryoglobulinemic vasculitis: remission after antiviral therapy with entecavir. Kindey Blood Press Res 39: 65-73.
- Enomoto M, Nakanishi T, Ishii M, Tamori A, Kawada N (2008) Entecavir to treat hepatitis B–associated cryoglobulinemic vasculitis. Ann Intern Med 149: 912-913.
Relevant Topics
- Antibiotics and Resistance
- Antifungal
- Antiviral therapy
- Bacteremia
- Bacterial diseases
- Broad Spectrum of Antibiotics
- Clinical Infectious Diseases
- Diagnosis of Pathogenic microorganisms
- Emerging infections
- Natural Antibiotics
- Opportunistic Pathogens
- Parasitic Diseases
- Pertussis Vaccines
- Prevention of infection
- Septicemia
- Viral Infections
- Viremia
Recommended Journals
Article Tools
Article Usage
- Total views: 3473
- [From(publication date):
September-2017 - Aug 05, 2025] - Breakdown by view type
- HTML page views : 2588
- PDF downloads : 885