Did the Coexistence of a Pacemaker Probe, a Prominent Eustachian Valve and Induced Hypothermia Lead to Severe Pulmonary Embolism in a Resuscitated Patient after STEMI?
Received: 28-Feb-2017 / Accepted Date: 03-Mar-2017 / Published Date: 25-Mar-2017
Abstract
Post-cardiac arrest care is a particular interesting field and often depends on individual patient characteristics. Here we present the case of a patient with ST-elevation myocardial infarction, who developed severe pulmonary embolism originating from the proximity of a prominent Eustachian valve and the introduced pacemaker probe after targeted temperature management.
Keywords: Resuscitation; Post-cardiacarrest care; STEMI; Hypothermia; Pulmonaryembolism
78772Introduction
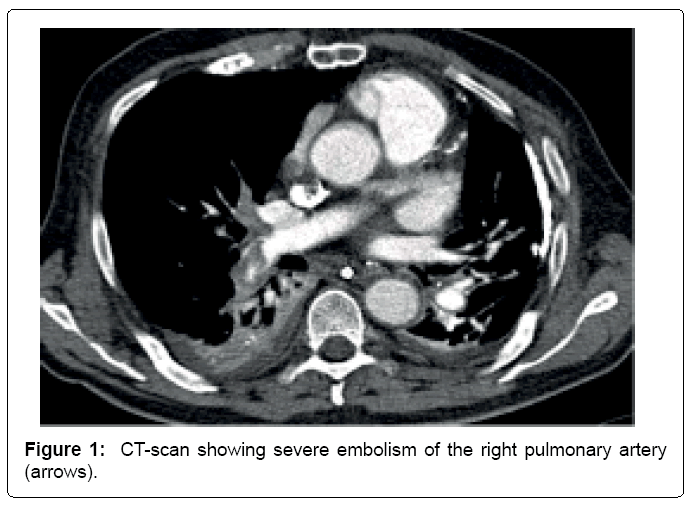
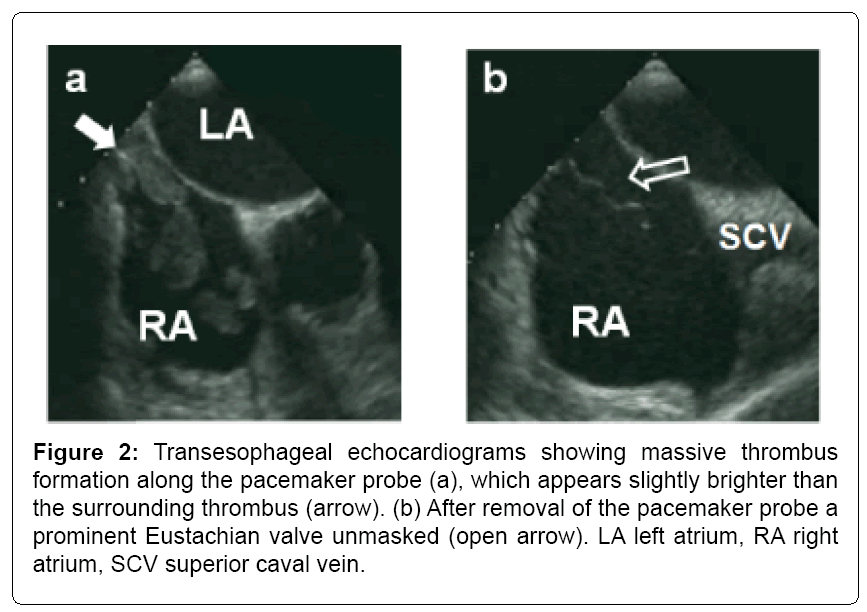
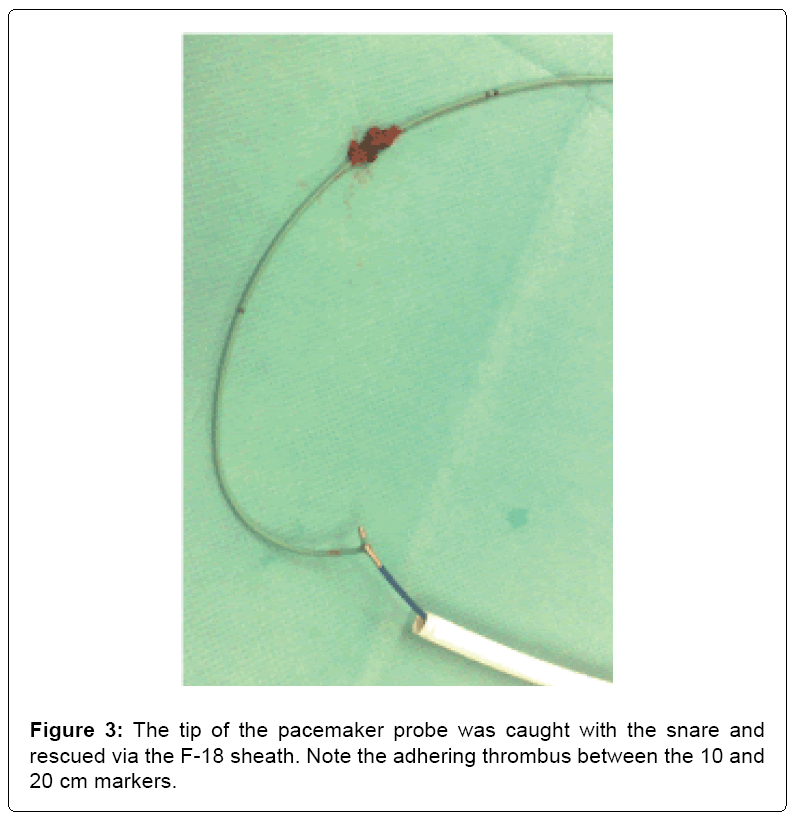
A 79-year old man collapsed in a shopping center. Five minutes later, the called emergency medical service found the patient pulseless and started cardiopulmonary resuscitation for approximately three minutes. Ventricular fibrillation was detected, the second shock was successful and return of spontaneous circulation (ROSC) could be established using low dosages of noradrenaline. Respiration was secured by intubation and the electrocardiogram (ECG) showed a sinus bradycardia with ST-elevations in the inferior leads. The cardiologist on duty scheduled the patient for immediate coronary angiography. The femoral access was chosen to also introduce a pacemaker (PM) probe due to the bradycardia and expected reperfusion arrhythmias. Corresponding to the ECG a fresh occlusion of the medial right coronary artery was found without significant lesions of the left coronary artery. The lesion could be recanalized and stented without complications, CKmax rose up to 1698 U/L the next day. The heart rate after PCI was around 50 bpm with infrequent PM activity: Frequency threshold was set at 40 bpm. Dual antiplatelet therapy (DAPT) was initiated after the patient was transferred to the intensive care unit. Hypothermia was induced with a core body temperature of 33°C for 24 hrs., then warming-up 0.2°C/h. Sinus bradycardia still was present with sporadic PM activity during the hypothermic period as well as in the night after warming. The PM probe was left in place. Two days after warming both, oxygen saturation and arterial blood pressure dropped. Echocardiography showed a prominent thrombus in the right atrium (RA) and a CT-scan revealed a severe pulmonary embolism (Figure 1). Deep vein thrombosis could be excluded via ultrasonography. To better understand the origination of the RA thrombus, a transesophageal echocardiography was conducted displaying a massively thrombotic coat of the pacemaker probe (Figures 2a and 2b). To prevent further embolism, we retrieved the PM probe using an Amplatz ev3 GooseNeck® snare kit introduced via a F-18 Cordis® sheath: therefore, the probe was retracted into the inferior caval vein (ICV) under transesophageal echocardiographic monitoring at first. Then the left ICV was punctured to introduce the snare, the tip of the probe was grabbed and pulled back into the sheath. Afterwards both were drawn out to show thrombotic material adhering to the probe (Figure 3). In the RA, a prominent Eustachian valve was unmasked after removal of the probe (Figure 2b). Additionally, thrombolytic therapy with 100 mg alteplase was given. Hemodynamics stabilized and the patient was weaned from catecholamines as well as ventilation. Still in the ICU, the patient improved hemodynamically and no permanent PM was necessary. Due to hypoxic brain damage within the resuscitation event, the patient was dependent on care. Seven days after the event, the patient was shifted to the cardiologic general ward. However, the patient acquired a severe pneumonia, and died two weeks later despite broad antibiotic therapy.
Figure 2: Transesophageal echocardiograms showing massive thrombus formation along the pacemaker probe (a), which appears slightly brighter than the surrounding thrombus (arrow). (b) After removal of the pacemaker probe a prominent Eustachian valve unmasked (open arrow). LA left atrium, RA right atrium, SCV superior caval vein.
Discussion
Following post-cardiac arrest care guidelines, the patient received an immediate coronary angiography. Several observational studies have demonstrated improved survival as well as improved neurologically favorable outcome associated with emergency coronary angiography in patients with ST elevation after cardiac arrest [1,2]. The hemodynamic goal of post-cardiac arrest care, i.e., a systolic blood pressure of 90-100 mmHg [3], was achieved with low dosages of noradrenaline. Higher blood pressure values could favor bleeding, which is of special interest in this patient due to targeted temperature management, as discussed below. The term targeted temperature management (TTM) refers to induced hypothermia and active control of temperature as well. While with patients experiencing out-of-hospital cardiac arrest and nonshockable rhythms, observational data are conflicting and randomized data are not available, the situation for out-of-hospital cardiac arrest and ventricular fibrillation or pulseless ventricular tachycardia is associated with more conclusive evidence: data exists from one randomized and one quasirandomized clinical trial, both reporting an increased functional recovery and an increased survival after induced hypothermia with a temperature target of 33°C and 32-34°C, respectively [4,5]. However, due to reduced function of enzymatically based coagulation, diminished concentration of thrombocytes (due to increased sequestration in the portal circulation), extended partial thromboplastin time and decreased Quick’s value, bleeding tendency during hypothermia is enhanced [6,7]. The thromboembolic event in this patient occurred two days after warming up to physiological temperature, therefore one might speculate on the occurrence of a rebound effect to an exaggerated clotting. The site of thrombus adherence on the pacemaker probe next to the Eustachian valve in combination with the remarkable size of the valve is suggestive of an influence in thrombus formation (compare Figures 2a and 2b).
The Eustachian valve is an anatomically fairly distinct structure. Helpful in fetal life, it can disappear completely or remain as a thin ridge. In most cases, it is a falciform fold of endocardium arising from the anterior rim of the ICV. Large Eustachian valves can float in the cavum of the RA and appear as a mobile, several centimeters elongated structures. Thrombus formation over the Eustachian valve has been reported to occur extremely rare – under normal circumstances [8,9]. It is expendable to mention, that the situation in TTM has not been evaluated. However, thrombi associated to pacemaker probes are not uncommon. For example, van Rooden et al. report about 23% albeit on permanent probes [10]. The question, whether the pulmonary embolism could have been prevented in this patient is hard to answer. Potentially, an earlier and closer examination, e.g. by echocardiography, on the RA structures could have prevented thrombus growth to such a hemodynamic relevant size. The combined approach of invasive probe removal and lysis therapy helped to restore and maintain a stable cardiopulmonary circulatory in this patient.
Conclusion
We report a rare clinical setting, in which a thrombus formed despite DAPT and prophylactic heparin dosage on a pace maker probe close to a prominent Eustachian valve after induced hypothermia. Apparently, it cannot be determined which of the discussed factors favoring coagulation were most relevant. To learn from this, it could be helpful to check the anatomy of the Eustachian valve in patients after induced hypothermia who have a transfemorally introduced pacemaker probe in order to eventually adapt the anticoagulation scheme or reassess the pacemaker indication more critically.
References
- Jeppesen JB, Kjaergaard J, Wanscher M, Pedersen F, Holmvang L, et al. (2012) Emergency coronary angiography in comatose cardiac arrest patients: do real-life experiences support the guidelines? Eur Heart J Acute Cardiovasc Care 1: 291-301.
- Strote JA, Maynard C, Olsufka M, Nichol G, Copass MK, et al. (2012) Comparison of role of early (less than six hours) to later (more than six hours) or no cardiac catheterization after resuscitation from out-of-hospital cardiac arrest. Am J Cardiol 109: 451-454.
- Kilgannon JH, Roberts BW, Reihl LR, Chansky ME, Jones AE, et al. (2008) Early arterial hypotension is common in the post-cardiac arrest syndrome and associated with increased in-hospital mortality. Resuscitation 79: 410-416.
- Hypothermia after Cardiac Arrest Study G. (2002) Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 346: 549-556.
- Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, et al. (2002) Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 346: 557-563
- Rohrer MJ, Natale AM (1992) Effect of hypothermia on the coagulation cascade. Crit Care Med. 20: 1402-1405.
- Johnston TD, Chen Y, Reed RL (1994) 2nd. Functional equivalence of hypothermia to specific clotting factor deficiencies. J Trauma 37: 413-417.
- Jolly N, Kaul UA, Khalilullah M. (1991) Right atrial thrombus over eustachian valve--successful lysis with streptokinase. Int J Cardiol 30: 354-356.
- Moral S, Ballesteros E, Huguet M, Panaro A, Palet J, et al. (2016) Differential Diagnosis and Clinical Implications of Remnants of the Right Valve of the Sinus Venosus. J Am Soc Echocardiogr. 29: 183-194.
- van Rooden CJ, Molhoek SG, Rosendaal FR, Schalij MJ, Meinders AE, et al. (2004) Incidence and risk factors of early venous thrombosis associated with permanent pacemaker leads. J Cardiovasc Electrophysiol 15: 1258-1262.
Citation: Schach C, Brünnler T, Luchner A (2017) Did the Coexistence of a Pacemaker Probe, a Prominent Eustachian Valve and Induced Hypothermia Lead to Severe Pulmonary Embolism in a Resuscitated Patient after STEMI? Cardiovasc Ther 2: 116.
Copyright: © 2017 Schach C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 4316
- [From(publication date): 0-2017 - Jul 12, 2025]
- Breakdown by view type
- HTML page views: 3397
- PDF downloads: 919