Case Report Open Access
Duodenal Gastrinoma Associated with Multiple Endocrine Neoplasia Type 1 (MEN1) Detected by Esophagogastroduodenoscopy (EGD), which was buried under Ulcer
Kenji Sasaki*
Department of Internal Medicine, Shiogama City Hospital, Japan
- Corresponding Author:
- Kenji Sasaki, MD, PhD
Department of Internal Medicine, Shiogama City Hospital
7-1, Kouzumachi, Shiogama, Miyagi, 985-0054, Japan
Tel: +81-22-364-5521
Fax: +81-22-364-5529
E-mail: kydosarnymai@aria.ocn.ne.jp
Received Date: April 12, 2016; Accepted Date: April 21, 2016; Published Date: April 26, 2016
Citation: Sasaki K (2016) Duodenal Gastrinoma Associated with Multiple Endocrine Neoplasia Type 1 (MEN1) Detected by Esophagogastroduodenoscopy (EGD), which was buried under Ulcer . J Gastrointest Dig Syst 6:418. doi:10.4172/2161-069X.1000418
Copyright: © 2016 Sasaki K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
A 66-year-old Japanese male was shown to have severe ulcers with hypergastrinemia in the stomach through proximal horizontal part of the duodenum, who complained of dysphagia and vomiting. He suffered from gastric ulcer at 63, proven to have undergone parathyroidectomy for hyperparathyroidism at his 5th decade. Though had no definitely enlarged pituitary detectable by computed tomography (CT), he had slight defects in the visual field and hyperprolactinemia. A diagnosis of MEN1 was entertained. Follow up EGD revealed 5 small sessile submucosal tumors (SMTs) with a central depression or erosion in the duodenal bulb through descending part of the duodenum, which had been obscured beneath ulcers. Demonstrated in the regenerative mucosa by their biopsy were clusters of small tumor cells, which, though considered the tips of neuroendocrine (NE) tumor (NET) lying in the deeper layer, were not large enough to be proven so by immunostaining with the markers in the serial sections, and diffuse hyperplasia of synaptophysin-, chromogranin A- and gastrin-positive NE cells in Brunner glands (BGs), the preneoplastic lesion characteristic of MEN1-associated duodenal gastrinoma, supporting the diagnosis, which was firmly guaranteed by positively elevated glucagon-provoked plasma gastrin. Subtotal stomach-preserving pancreaticoduodenectomy (SSPPD) established the final diagnosis of duodenal gastrinomas graded G1 associated with MEN1, which were shown to be tightly contained in the densely conglomerated hyperplastic BGs. No metastases were detected. This is the first case in the world, in which all the three characteristics of MEN1- associated duodenal gastrinoma were demonstrated by EGD. Difficulty in endoscopically detecting the NET lies in the fact that, in addition to its smallness and deep localization, it might be buried under peptic ulcer at a certain stage of the natural history and that an attempt to biopsy it is hampered by the densely conglomerated barrier of the hyperplastic BGs in some cases.
Keywords
Duodenal gastrinoma; EGD; MEN1; Peptic ulcer; Zollinger-Ellison syndrome (ZES); Natural history
Introduction
MEN1 is a rare, autosomal dominant, hereditary cancer syndrome producing various sets of tumors [1], a practical definition of which is a case with at least two of the three main related endocrine, pituitary, parathyroid and enteropancreatic, tumors [2].
Development of the second commonest tumor in the last category [1] leads to excessively increased gastrin secretion, engendering ZES. Duodenal gastrinoma occurring in about half the cases of the sporadic ZES (3) is hardly localized preoperatively by any diagnostic modalities [3-5] and rarely diagnosed endoscopically [6].
Though almost exclusively presents itself in the duodenum, which should be the first site to be examined for the NET, the MEN1- associated counterpart is no less hardly localized even by the newly developed modalities [3,4] and still less commonly detected by EGD [7].
This report presents a case of MEN1-associated duodenal gastrinoma detected by EGD and definitely diagnosed before the operation, which was buried under peptic ulcer.
Case Report
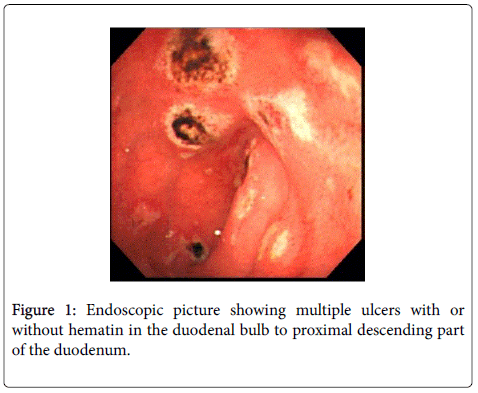
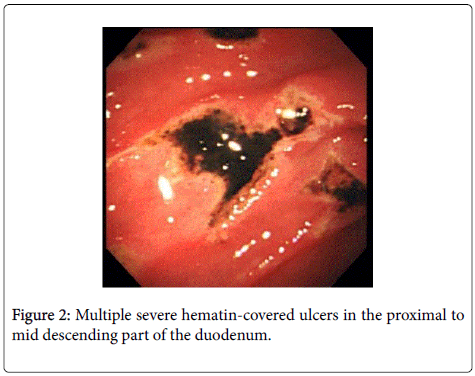
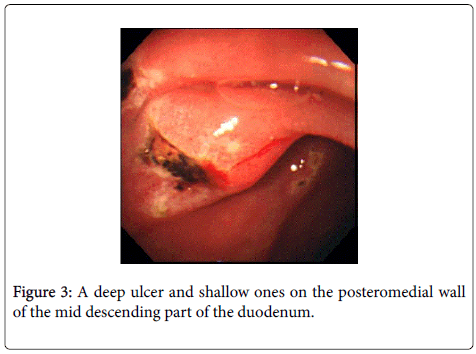
A 66-year-old Japanese male mechanic presented with a 2-day history of dysphagia and vomiting. The abdomen was slightly protruding but there was no organomegaly. EGD demonstrated severe ulcers mostly covered with hematin in the stomach through the proximal horizontal part of the duodenum (Figures 1-3). The rugae of the greater curvature of the gastric body were not coarse.
The papilla of Vater looked normal. The Helicobacter pylori-positive stomach and duodenum were so severely ulcerated with the evidence of recent hemorrhage that biopsy was withheld lest the procedure induce further bleeding.
Though not taking nonsteroidal anti-inflammatory drugs (NSAIDs) or any drugs at the time of this episode, which might influence gastrin secretion, he had hypergastrinemia (680 pg/ml, normal <200 pg/ml). He was suspected of having ZES.
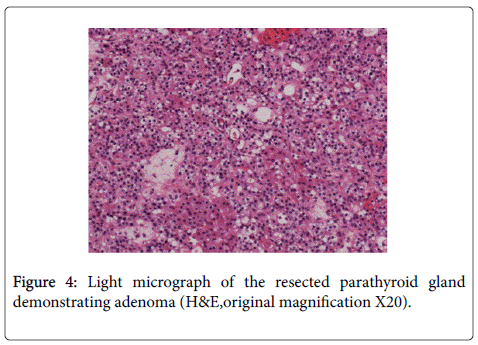
He had a long, broadened U-shaped operative wound in the anterior neck and small ones on the ventral surface of the left forearm, which, though he stubbornly insisted of having been thyroidectomized, were proven to be the evidences of parathyroidectomy for hyperparathyroidism (Figure 4) and autotransplantation of the glands he underwent at his 5th decade by referring to his former endocrinologist. Serum calcium and intact parathyroid hormone (PTH) were at the upper normal limit. Despite his congenital anomaly of the pelvis, his other past and family histories were noncontributory except that he suffered from gastric ulcer at the age of 63. Though had no definitely enlarged pituitary detectable by CT, he had slight defects in the right lower temporal and left upper nasal visual fields and moderate hyperprolactinemia (51.20 ng/ml, normal 3.58-12.78 ng/ml). A diagnosis of MEN1 was entertained.
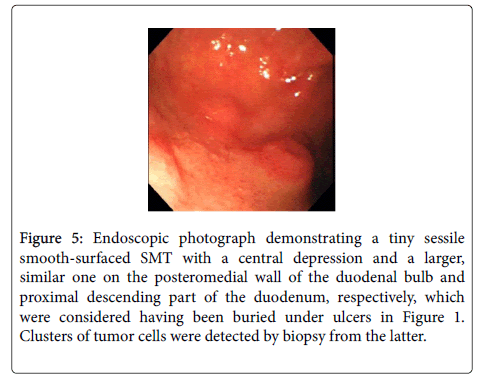
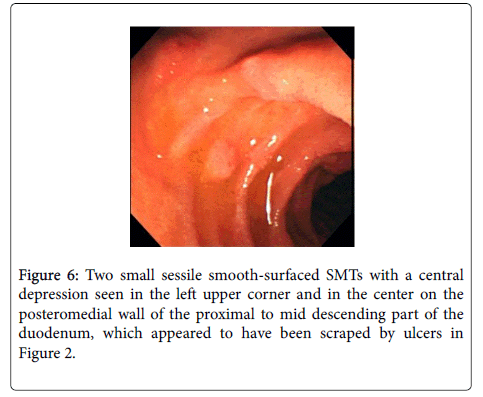
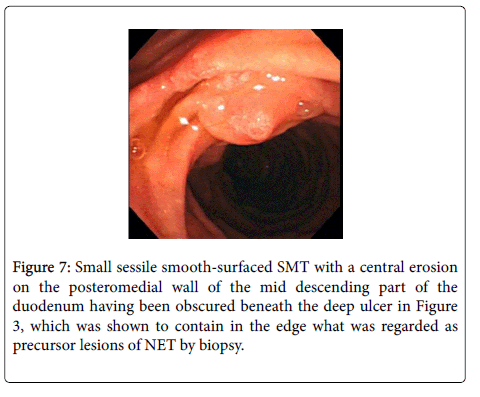
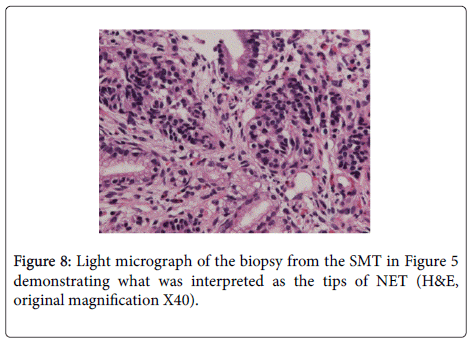
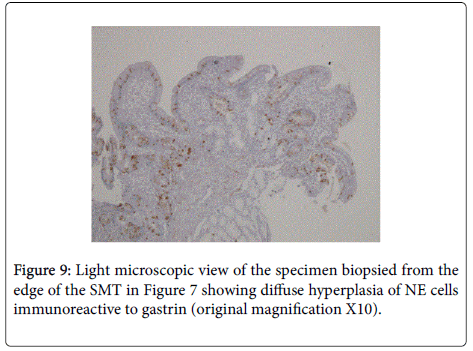
Follow up EGD after healing of duodenal ulcers showed a total of 5 small smooth-surfaced sessile SMTs covered with the normalappearing duodenal mucosa with a central depression or erosion on the posteromedial wall of the duodenal bulb through descending part of the duodenum (Figures 5-7), which, having escaped detection under severe ulceration, could not be proven present by endoscopic ultrasonography (EUS). Gastric ulcers were very much decreased in size or turned into scars, biopsy of which showed no malignancy. A specimen biopsied from the larger SMT in Figure 5 showed tiny clusters of small tumor cells, which, though considered to be the tips of NET lying in the deeper layer, were not large enough to be proven so by immunostainig with the markers in the serial sections (Figure 8) and another specimen obtained from the edge of the SMT in Figure 7 was interpreted as diffuse hyperplasia of NE cells in BGs, which was positive for synaptophysin, chromogranin A and gastrin but negative for insulin, glucagon, cluster designation antigen 56 (CD56) or thyroid transcription factor 1 (TTF1) (Figure 9), the characteristic preneoplastic lesion observed only in a case of MEN1-associated duodenal gastrinoma (8). Both findings were detected in the inflammatory slightly hyperplastic regenerative mucosa, indicating that these lesions had been buried under peptic ulcers, and, though not the definitive evidences, strongly supported the diagnosis of duodenal gastrinoma associated with MEN1.
Figure 5: Endoscopic photograph demonstrating a tiny sessile smooth-surfaced SMT with a central depression and a larger, similar one on the posteromedial wall of the duodenal bulb and proximal descending part of the duodenum, respectively, which were considered having been buried under ulcers in Figure 1. Clusters of tumor cells were detected by biopsy from the latter.
Plasma gastrin was elevated to 761 pg/ml from 524 pg/ml 5 minutes after intravenous administration of 20 g/kg of glucagon, showing increment of greater than both 200 pg/ml and 35% from the basal value, which satisfied the positive diagnostic criteria of gastrinoma [8,9]. The diagnosis of MEN1, multiple duodenal gastrinomas with probable pituitary prolactinoma developed 20 years preceded by hyperparathyroidism, was firmly vindicated.
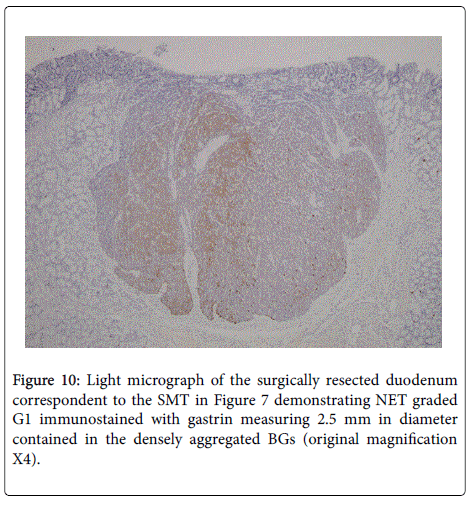
EUS and CT showed a cystic lesion in the pancreatic body, which was revealed to be NET non-immunoreactive to any hormones by EUS-fine needle aspiration biopsy (FNA). SSPPD, during which the duodenal NETs were not palpable by the surgeons from the serosal surface, resulted in the final diagnosis of multiple duodenal gastrinomas graded G1, which, including the largest measuring 2.5 mm in diameter, were shown to be embedded in the densely conglomerated hyperplastic BGs (Figure 10), and nonfunctioning pancreatic NET graded G1 associated with MEN1. No metastases were detected.
Though kept a fair post-operative course, he died apparently from non-occlusive mesenteric ischemia before having the pituitary closely examined.
Discussion
MEN1 is a rare, autosomal dominant, hereditary cancer syndrome developing enteropancreatic tumors, gastrinoma included, in 56% of the afflicted individuals [10], which accounts for 22% of all the ZES [3]. Though almost exclusively originates in the duodenum in MEN1, which should be the first site to be examined for the NET [7], gasrinoma has hardly been localized in the organ preoperatively even by the newly developed diagnostic modalities [3,4] and extremely rarely detected by EGD [7].
The endoscopic feature of duodenal gastrinoma, whether in the sporadic ZES or associated with MEN1, used to be reported to be an SMT covered with the normal-appearing overlying mucosa measuring from 0.3 cm to 1.5 cm in diameter with a central depression [6,11,12], as in the present case. But a case of the sporadic duodenal gasrinoma was also reported [13], which was shown to be a small SMT without a central depression by the endoscopic picture. The lesions reported, so far, are all solitary and no reports have been published, in which gastrinoma was explicitly recognized by EGD as multiple SMTs in the duodenum containing gastrin-positive NET in the deeper layer of the epithelium. The multiplicity of the lesion is definitely due to the fact that the present case was not afflicted with the sporadic ZES but MEN1, because duodenal gastrinoma associated with the latter is considered arising from multiple proliferative gastrin cell changes (8), each of which shows a distinct pattern of allelic deletion of the MEN1 gene, endorsing the concept that each MEN1-associated gastrinoma originates from an independent cell clone [14]. This is the first case in the world, in which all the three characteristics of MEN1-associated duodenal gastrinoma, smallness, deep localization, and multicentricity, underlined in the resected specimens [7] were demonstrated by EGD, the diagnosis of which was pathologically proven accurate.
It could be safely stated that the presence of multiple small sessile SMTs with a central depression or erosion in the duodenum of a patient with peptic ulcer is a finding highly suggestive of MEN1- associated gastrinoma. In the present case, such a finding was completely obscured by the presence of severe gastroduodenal ulcers and it was not until the duodenal ulcers were healed when the duodenal SMTs were distinctly detected. It is certain that the gastrinoma-containing SMTs had been eroded by the severe duodenal ulcers in this case, which rendered them undetectable, and that, as the ulcers were healed, they recovered their size to some extent. Each SMT in Figures 4 and 5 appeared to have been scraped by the ulcers in Figures 1 and 2, respectively, and the one in Figure 7 had also been buried under the deep lesion in Figure 3. Such an opinion was validated by the findings that hyperplasia of gastrin-producing NE cells and the clusters of tumor cells were detected in the regenerative mucosa by biopsy, which indicate that they had been buried under ulcers. In addition, a case of the sporadic ZES was reported with conclusive biochemical and clinical evidence of duodenal gastrinoma complicated with multiple duodenal ulcers including perforating one, in the surgically resected specimen of which no tumors were detected [15]. It is probable that gastrinoma was completely eradicated by one of the ulcers, particularly the perforating one, though the authors contended that it had been overlooked by the pathologists.
If SMTs with a central depression or erosion are detected in the duodenum of a patient with peptic ulcer possessing a background predisposing him to MEN1 even without prominent hypergastrinemia during a course of the disease, it is necessary, in order to establish diagnosis, to execute prudent biopsy from the lesions in the light of tiny NET in the rather deeper layer of the epithelium [7] probably contained in a densely packed mass of the hyperplastic BGs [8], which constitute the firmly embedding outer shell in the SMT far larger than the core, gastrinoma per se: the largest NET in the present case accounted for only 1/8 of the total volume of the SMT. The present gastrinoma was considered derived from BGs but not from the crypts [8].
In conclusion, this is the first case in the world, in which all the three characteristics of MEN1-associated duodenal gastrinoma were exquisitely demonstrated by EGD. The reason the NET is extremely hardly endoscopically detectable is not only due to its small size and deep localization alone but also due to the fact that it might be buried under peptic ulcer at a certain stage of the natural history, as depressed typed early gastric cancer is often alleged to be in the so-called malignant cycle, and that an attempt to biopsy the NET is hampered by the densely conglomerated barrier of the hyperplastic BGs in some cases.
Acknowledgments
The author wishes to express his gratitude to Dr Masuda at Miyagi Cancer Center and Dr Iwama at Tohoku Rosai Hospital for their extremely helpful instructions.
References
- Jensen RT, Cadiot G, Brandi ML, de Herder WW, Kaltsas G, et al. (2012) ENETS consensus guidelines for the management of patients with digestive neuroendocrine neoplasms: functional pancreatic endocrine tumor syndromes. Neuroendocrinology 95: 98-119.
- Brandi ML, Gagel RF, Angeli A, Bilezikian JP, Beck-Peccoz P, et al. (2001) Guidelines for diagnosis and therapy of MEN type 1 and type 2.J ClinEndocrinolMetab 86: 5658-5671.
- Jensen RT (2004) Gastrinomas: advances in diagnosis and management.Neuroendocrinology 80: 23-27.
- Ruszniewski P, Amouyal P, Amouyal G, Grangé JD, Mignon M, et al. (1995) Localization of gastrinomas by endoscopic ultrasonography in patients with Zollinger-Ellison syndrome.Surgery 117: 629-635.
- Cadiot G, Lebtahi R, Sarda L, Bonnaud G, Marmuse JP, et al. (1996) Preoperative detection of duodenal gastrinomas and peripancreatic lymph nodes by somatostatin receptor scintigraphy. Gastroenterology 111: 845-854.
- Wu WC, Kengis J, Whalen GE, Schulte WJ, Unger GF, et al. (1974) Endoscopic localization of a duodenal wall tumor in Zollinger-Ellison syndrome.Gastroenterology 66: 1237-1239.
- Pipeleers-Marichal M, Somers G, Willems G, Foulis A, Imrie C, et al. (1990) Gastrinomas in the duodenums of patients with multiple endocrine neoplasia type 1 and the Zollinger-Ellison syndrome.N Engl J Med 322: 723-727.
- Anlauf M, Perren A, Meyer CL, Schmid S, Saremaslani P, et al. (2005) Precursor lesions in patients with multiple endocrine neoplasia type 1-associated duodenal gastrinomas. Gastroenterology 128: 1187-1198.
- Shibata C, Kakyo M, Kinouchi M, Tanaka N, Miura K, et al. (2013) Criteria for the glucagon provocative test in the diagnosis of gastrinoma.Surg Today 43: 1281-1285.
- Yamazaki M, Suzuki S, Kosugi S, Okamoto T, Uchino S, et al. (2012) Delay in the diagnosis of multiple endocrine neoplasia type 1: typical symptoms are frequently overlooked.Endocr J 59: 797-807.
- Gilhool WJ (1984) Endoscopic diagnosis and removal of a duodenal wall gastrinoma.Am J Gastroenterol 79: 679-683.
- Wadas DD, Foutch PG, Manne RK, Sanowski RA (1988) Endoscopic diagnosis of a duodenal gastrinoma.GastrointestEndosc 34: 430-431.
- Lee SH, Hong YS, Lee JM, Jang BK, Chung WJ, et al. (2009) Duodenal gastrinoma treated with endoscopic band ligation.GastrointestEndosc 69: 964-967.
- Anlauf M, Perren A, Henopp T, Rudolf T, Garbrecht N, et al. (2007) Allelic deletion of the MEN1 gene in duodenal gastrin and somatostatin cell neoplasms and their precursor lesions.Gut 56: 637-644.
- Thompson NW,Vinik AI, Eckhauser FE (1989) Microgastrinomas of the duodenum. A cause of failed operations for the Zollinger-Ellison syndrome.Ann Surg 209: 396-404.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13346
- [From(publication date):
April-2016 - Aug 03, 2025] - Breakdown by view type
- HTML page views : 12382
- PDF downloads : 964