Research Article Open Access
Dysfunctional Behaviors in Children and Adolescents with Neurocardiogenic Syncope
Teresa Grimaldi Capitello1*, Silvia Placidi2, Corrado Di Mambro2, Fabrizio Gimigliano2, Roberta Vallone1, Fabrizio Drago1, Simona Scateni3, UmbertoRaucci3, Vincenzo Maria Di Ciommo4 and Simonetta Gentile21Department of Neuroscience and Neurorehabilitation, Clinic Psychology Unit, Bambino Gesù Children’s Hospital, Rome, Italy
2Department of Paediatric Cardiology and Cardiac Surgery, Paediatric Arrhythmia and Syncope Unit, Bambino Gesù Children’s Hospital, Rome, Italy
3Emergency Department, Bambino Gesù Children’s Hospital, Rome, Italy
4Epidemiology and Biostatistics, Bambino Gesù Children’s Hospital, Rome, Italy
- *Corresponding Author:
- Grimaldi Capitello
Department of Neuroscience and Neurorehabilitation
Clinic Psychology Unit, Bambino Gesù Children’s Hospital
Piazza S.Onofrio, 4, 00165, Rome, Italy
Tel: 0039 06 68592179
Fax: +39.06.68592781
E-mail: teresa.grimaldi@opbg.net
Received Date: July 21, 2014; Accepted Date: August 29, 2014; Published Date: September 01, 2014
Citation: Grimaldi Capitello T, Placidi S, Mambro CD, Gimigliano F, Vallone R et al. (2014) Dysfunctional Behaviors in Children and Adolescents with Neurocardiogenic Syncope. J Child Adolesc Behav 2:156. doi:10.4172/2375-4494.1000156
Copyright: © 2014 Capitello TG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Objective: We evaluate a large sample of children and adolescent with suspected neurocardiogenic syncope (NCS) and we compared the results with a healthy sample, with the aim to reveal a possible correlation between syncopal events and dysfunctional behaviors. Methods: A total number of ninety two patients with NCS (median age 14.7 years) were evaluated with Head-Up Tilt Test (HUTT) and psychological assessment at the same time. The results of the ninety two patients who underwent HUTT and completed psychological tests were compared with a normative group. The risk of psychosocial dysfunctions was assessed by using the standardized Italian version of the Child Behavior Checklist in Youth Self Report (YSR). Results: Compared with normative group, patients with NCS reported worse scores to the internalizing and total problem scales and to the syndrome scales of anxiety problems, depressive withdrawal problems, somatic complaints, social problems and thought problems. Conclusions: Patients with NCS present major emotional and behavioral dysfunctions than healthy sample. Our findings call for additional investigations on the possible pathophysiological association between psychosocial problems and the reflex mechanism that produces syncope. Furthermore, future clinical studies are necessary to plan an interventional strategy and optimize the clinical management.
Keywords
Neurocardiogenic syncope; Parenting distress; Multidisciplinary approach; Internalizing problems
Abbreviations
CBCL- Child Behaviour Checklist; ECG-12-lead electrocardiogram; HUTT- Head Up Tilt Test; NCS-Neurocardiogenic Syncope
Introduction
Syncope is a common clinical problem in children and adolescents, with as many as 15% of children experiencing at least one episode before the end of adolescence [1].
Although syncope is almost always benign, in few cases it may be a clue to the presence of underlying cardiovascular problem and may predict a risk of sudden death. Secondarily it may reflect neurological or metabolic pathology. Thus, syncope represents a major challenge for physicians, and medical resources and expenses associated with syncope management are enormous [2,3].
Several guidelines and diagnostic algorithms have been developed with the aim to improve the management of such patients, but only few data are available for paediatric patients.
As previously reported, neurocardiogenic syncope (NCS) is the most common in paediatric age [4]. It is not based on cardiac or neurological origins.
Although the pathogenesis is well known, the causes of NCS in children are not yet well established. This can generate anxiety in the children and their family. The re-occurrence of these events can have a negative impact on participation in daily activities (e. g. make many school absences, do not attend sports and in general reduce physical fitness) and increase emotional aspects such as fear and emotional distress, reinforcing psychosocial maladaptive behaviors.
As many other stress-related symptoms, syncope is recognized as a condition with a great psychological component that involves autonomic nervous system dysfunction [5].
Some studies showed a high prevalence of psychiatric morbidity among syncope patients, with rates up to 80% in adult patients, but relevant data in children and adolescents are few [6,7].
Several earlier studies on patients with syncope have found significant deviations in behavior, in the development of psychopathological symptoms [7] and in the effects of pediatric syncope on health-related quality of life [6], but few studies have observed significant difference in behavior if compared with control group of healthy subjects [8,9].
Byars et al. [9] studied 44 children with a history of recurrent syncope and reported adjustment difficulties, including symptoms of anxiety and social withdrawal. In contrast, Blount et al. [8] reported no significant differences in depressive symptoms in 36 children with syncope and a positive HUTT, when compared with 20 children with syncope but negative HUTT.
Moreover, the identification of psychosocial difficulties is complex in pediatric populations and requires input from the family. Many of these investigations have been guided by a conceptual framework incorporating stress and coping, family systems, and social learning theories[8,9].
The aim of our study was to evaluate the psychological profile in patients with NCS, making the hypothesis that children with NCS have major dysfunctional emotions and behaviours compared with a normative sample.
Methods
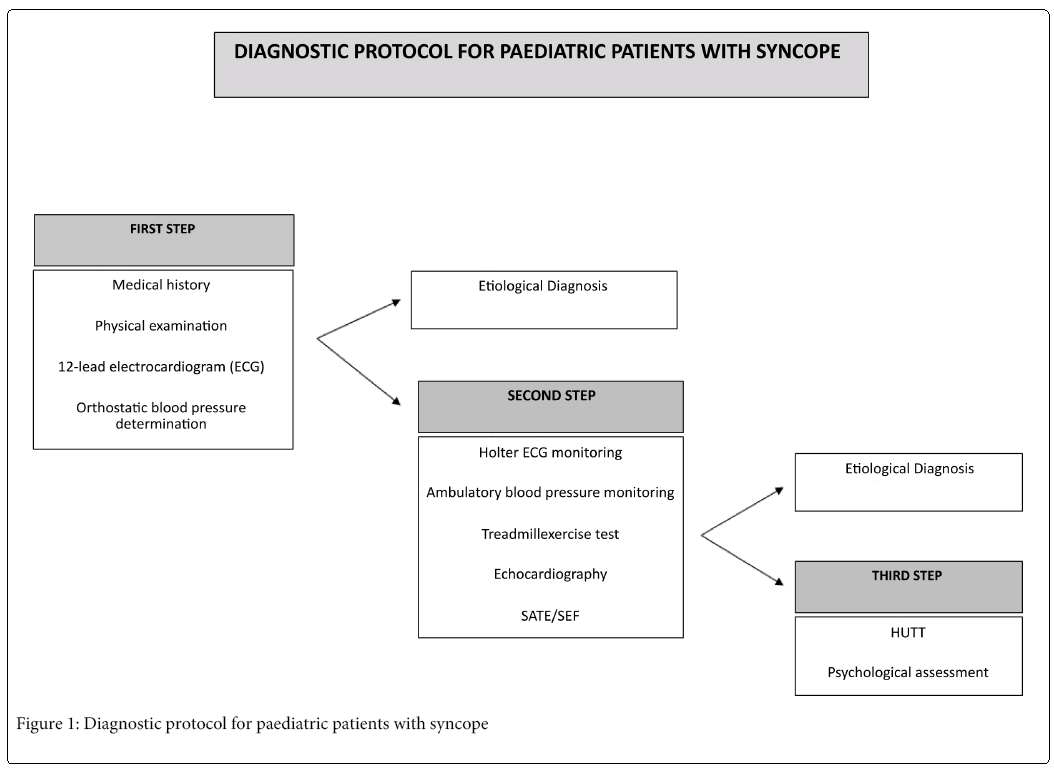
This study included all consecutive patients with syncope or pre-syncope who underwent the Head Up Tilt Test (HUTT) in our Paediatric Arrhythmia and Syncope Unit at Bambino Gesù Children’s Hospital from October 2011 to August 2012. All patients were visited and diagnosed by a paediatric cardiologist with broad experience in pediatric syncope, following a specific protocol with three steps, described in Figure 1.
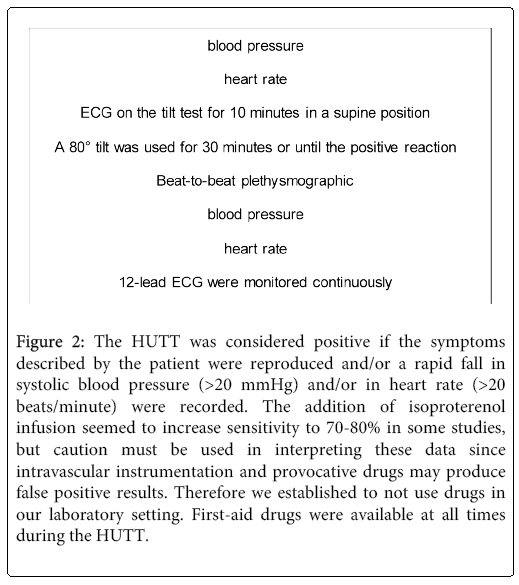
The third step was performed in patients with suspected NCS when all other causes of syncope were excluded (e. g. cardiac and neurological causes). These patients were admitted HUTTs and to a contextual psychological assessment. All HUTTs were performed by a paediatric cardiologist, following a specific protocol, described in Figure 2. The psychological profile in these patients was assessed by a psychologist researcher to reveal a possible correlation between syncopal events and significant dysfunctional emotions and behaviors. Ethical Committee of our Institution approved the study and informed parental consensus was obtained for each patient.
Figure 2: The HUTT was considered positive if the symptoms described by the patient were reproduced and/or a rapid fall in systolic blood pressure (>20 mmHg) and/or in heart rate (>20 beats/minute) were recorded. The addition of isoproterenol infusion seemed to increase sensitivity to 70-80% in some studies, but caution must be used in interpreting these data since intravascular instrumentation and provocative drugs may produce false positive results. Therefore we established to not use drugs in our laboratory setting. First-aid drugs were available at all times during the HUTT.
Exclusion criteria
Patients with diagnosis of cardiac, neurological or metabolic causes of syncope were excluded. Subjects were excluded if parents did not speak Italian, if the child was in foster/social care, if a mental retardation was diagnosed or the consultant felt that parents could become unduly distressed by participation.
Psychological assessment
Each patient with suspected NCS underwent a psychological evaluation and completed a questionnaire booklet.
The booklet contained one questionnaire for the patients. Some standardized measures were identified as related to social and school competences, to perception of own and other emotions and to presence of dysfunctional behaviors in childhood and adolescence.
The results of the questionnaires for the patients were compared with a normative population composed by healthy age- and gender-matched children and adolescents, recruited randomly from a sample selected in the schools in three provinces of Northern Italy [10].
Child-completed measure. The risks of dysfunctional behaviors and low adaptability in children and adolescents with syncope were assessed using the standardized Italian version of the Youth Self-Report form for patients 11-18 years (YSR/11-18) [10,11]. It is a self-report questionnaire with eight syndrome subscales (Anxious/Depressed, Withdrawn/Depressed, Somatic Complaints, Social Problems, Thought Problems, Attention Problems, Rule-Breaking Behavior, and Aggressive Behavior) which are related to screening emotional and behavioral problems across multiple cultures [12,13]. Although no normative Italian data on the most recent YSR are available to date, the psychometric properties of the previous YSR [14] version have been investigated recently in a study conducted in Italy, that showed the good validity and reliability of this test on the Italian population [15].
Statistical analysis
Data were analysed using SPSS (v20.0) (IBM Corporation, Somers, NY, USA). Differences between patients and non-patients for psychological variables were assessed using chi-squared and t-tests, as appropriate. Continuous and categorical variables ( e. g., clinical and demographic characteristics) were analysed using independent t-tests and chi-squared tests respectively. All values are reported as mean (M) and/or standard deviation (SD).
Results
Demographic and diagnostic characteristics
In a study period of eleven months we investigated a total number of one hundred twenty six patients with suspected NCS. Of the one hundred twenty six patients who underwent HUTT and were evaluated by a contextual psychological assessment, ninety-two (73%), completed the psychological evaluation and results were compared with a normative group. Thirty-four patients were excluded because they satisfied the exclusion criteria. In this multidisciplinary study were studied ninety two patients with NCS. All patients were aged between 6 and 18 years and 55% were male. Median age was 14.7 years (range 9.9- 18.8 years). Median age at the first syncopal event was 11.3 years. Median follow up was 5.2 months.
Recurrent syncope, defined as more than 2 events over a period of 6 months, was present in 66/92 patients (71.7%). Medical history highlighted a positive family history for NCS, breath holding spells or sudden death in 28/92 cases (30.4%). Moreover, in 25/92 (27%) of our patients with syncope the etiology remained unexplained. HUTT showed a positive response in 45/92 patients (48.9%). (view Table 1).
| Number of child partecipants | 92 |
|---|---|
| Patients Mean age (SD) | 14.7(2.75) |
| Sex | |
| Female | 45% |
| Male | 55% |
| Recurrent syncope | 66 (71.7%) |
| Mean age first syncopal event | 11.3 |
| Family history for syncope | |
| Breath holdind spells | 28 (30.4%) |
| Unexplained etiology | 25 (27%) |
| HUTT | |
| Positive | 45 (48.9%) |
SD= Standard Deviation; NCS= Neurocardiogenetic Syndrome;
HUTT= Head Up Tilt Test
Table 1: Description of patients characteristics
Emotional and behavioral dysfunctions
Data are presented regarding between-group differences based on children’ and adolescents’ psychological functioning. YSR broad scale scores reveal the presence of psychopathological problems in many pediatric patients. The mean of total problem scale score for children and adolescents was 33.6, (range 3.0-91.0, SD = 19.3). The mean internalizing problem scale score for patients was 12.1 (range 1.0-37.0, SD = 8.0). The mean externalizing problem scale score for children and adolescents was 7.5 (range 0 -29.0, SD = 6.0). In our clinical sample, thirty-three patients (38%) scored above the 65th percentile in Total problems scale. And fourteen patients (16%) scored above the 65th percentile indicated by Achenbach as indicative of borderline and clinical levels in emotional (internalizing) and behavioral (externalizing) problems.
In particular, our pediatric patients with syncope had higher scores than healthy sample in YSR syndrome scales as Anxious/depressed scale (M 5.1, SD 3.5 vs M 3.6, SD 3.2), Withdrawn/depressed scale (M 3.2, SD 3.0 vs M 2.1, SD 2.0), Somatic Complaints scale (M 3.8, SD 3.1 vs M 1.3, SD 1.6), Social problems scale (M 2.8, SD 2.2 vs M 1.6, SD 1.7), Thought problems scale (M 2.5, SD 2.7 vs M 0.2, SD 0.6) (view Table 2).
| YSR Syndrome scales |
Patients with syncope N 92 |
General population N 1423 |
P value | t test |
|---|---|---|---|---|
| M (SD) | M (SD) | |||
| Anxious/depressed | 5.1 (3.5) | 3.6 (3.2) | <.001 | 4.08 |
| Withdrawn/depressed | 3.2 (3.0) | 2.1 (2.0) | <.001 | 4.82 |
| Somatic complaints | 3.8 (3.1) | 1.3 (1.6) | <.001 | 12.36 |
| Social problems | 2.8 (2.2) | 1.6 (1.7) | <.001 | 3.15 |
| Thought problems | 2.5 (2.7) | 0.2 (0.6) | <.001 | 22.82 |
| Attention problems | 4.4 (3.6) | 3.6 (2.9) | .015 | 2.44 |
| Rule-breaking behavior | 1.8 (1.7) | 1.3 (1.5) | .002 | 3.09 |
| Aggressive behavior | 5.7 (4.7) | 6.3 (4.7) | .26 | 1.12 |
|
YSR Broad scales |
||||
| Internalizing problems | 12.1 (8.0) | 6.9 (5.5) | <.001 | 8.27 |
| Externalizing problems | 7.5 (6.0) | 7.6 (5.8) | .91 | 0.11 |
| Total problems | 33.6 (19.4) | 23.2 (14.8) | <.001 | 6.25 |
Table 2: YSR scores of patients with syncope compared to general population
Discussion
Children and adolescents with NCS had major dysfunctional emotions and behaviours compared with a normative sample.
On top, YSR reports revealed some significant differences between the patients with NCS and healthy comparison subjects in internalizing and total problems scales and in many syndrome scales [16,17].
Although, other studies [6,7] evidenced a good prognosis in patients with NCS, we experienced a great impact on quality of life in patients and their families. In this group of patients we reported a major frequency of somatic and thought problems as skin problems, vomit, stomach problems, sleep problems and unusual thoughts compared with healthy subjects and of emotional problems as anxiety, depressive withdrawal and somatic complaints. According to used model a stress factor as the recurrent NCS and emotional and behavioral dysregulation can combine to determine the presence and severity of symptoms; therefore a conceptual framework incorporating stress and coping, family systems, and social learning theories could help to define which variables are more relevant [8,9].
Such divergent ratings are frequently observed [18], mainly because tendency to underestimate the presence of internalized disorders in pediatric age and for the few diagnostic tools in pediatric psychology. Thus, our data, along with previous reports [19], emphasize the need for health care providers to include psychological evaluation in clinical assessment of pediatric patients.
The identification of psychosocial difficulties is complex in pediatric populations and requires input from the family.
Our findings are in line with previous reports, implicating distressed family bonds and unstable parent-child relationship as important factors for syncope in children and adolescents. In addition, it has been reported that family cohesion and adaptability are significant factors in the adolescents’ feeling in control over their own health [10].
In our opinion, future researches should include cohort studies and further examination of the associations between children with NCS and other aspects of the psychological well-being, including the exploration of the influence of systemic factors on patient illness and psychological functioning. Extant literature supports the efficacy of specific therapeutic approaches designed to reduce symptoms of anxiety and depression that concomitantly reduce symptoms of recurrent syncope [19].
Conclusions
Syncope in pediatric age is a clinical challenge and requires diagnostic accuracy, clinical experience, and standardized protocol to optimize management.
NCS is a common disturbance in children, and it is well recognized as a stress related event and the psychological implication in pediatric age is relevant.
At the time of diagnosis, children and adolescents with NCS had higher scores of clinically significant somatic complaints and thought problems.
Our findings call for additional investigations on the possible pathophysiologic relation between somatic complaints, thought problems and the reflex mechanism that produces syncope.
The American Heart Association and European Society of Cardiology proposed guidelines for management of syncope [3,4] in adults. The clinical spectrum of syncope distinctly differs between children and adults, and the causes of syncope in adults are rarely the same in children [3].
Recently, an Italian Task Force developed guidelines for syncope in paediatric age with the contribute of major national scientific societies [20].
Future clinical studies are necessary to plan an interventional strategy during follow up and obtain the best management for these patients.
Acknowledgments
Authors Contribution
Dr. Grimaldi Capitello, Dr. Placidi, Dr. Scateni and Dr. Di Mambro contributed to the conception and the design of the study, as well as the data acquisition, analysis and interpretation. They drafted the manuscript and revised the final version.
Dr. Gimigliano, Dr. Raucci, Dr. Vallone and Dr. Gentile contributed to the conception and the design of the study, and data analysis and interpretation. They revised the drafted version and approved the final manuscript.
Dr. Di Ciommo contributed to the design of the study, the statistical analysis and the interpretation of results. He approved the final version as submitted.
Dr. Drago contributed to the conception and the design of the study, critically reviewed the data and the manuscript for important intellectual content and approved the final version as submitted.
The authors would like to thank Dr. Elisa Del Vecchio for her valuable collaboration in the editorial revision.
What is already known on this subject
Syncope is a common clinical problem in children. The causes of syncope in children and adolescents differ from that of adult patients. NCS is the most frequent type in children and is well recognized as a stress-related symptom.
What this study adds
This study reported a great number of children with syncope studied in a single centre. A psychological evaluation performed in patients with NCS highlights a significant prevalence of child distress.
Reference
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ Group and co-owners or contracting owning societies (where published by the BMJ Group on their behalf), and its Licensees to permit this article (if accepted) to be published in Archives of Disease in Childhood and any other BMJ Group products and to exploit all subsidiary rights, as set out in our licence.
References
- Wieling W, Ganzeboom KS, Saul JP (2004) Reflex syncope in children and adolescents. See comment in PubMed Commons below Heart 90: 1094-1100.
- Steinberg LA, Knilans TK (2005) Syncope in children: diagnostic tests have a high cost and low yield. See comment in PubMed Commons below J Pediatr 146: 355-358.
- Strickberger SA, Benson DW, Biaggioni I (2006) AHA/ACCF Scientific Statement on the evaluation of syncope: from the American Heart Association Councils on Clinical Cardiology, Cardiovascular Nursing, Cardiovascular Disease in the Young, and Stroke, and the Quality of Care and Outcomes Research Interdisciplinary Working Group; and the American College of Cardiology Foundation: in collaboration with the Heart Rhythm Society: endorsed by the American Autonomic Society. Circulation 113: 316-327.
- Brignole M, Alboni P, Benditt DG, Bergfeldt L, Blanc JJ, et al. (2004) Guidelines on management (diagnosis and treatment) of syncope--update 2004. See comment in PubMed Commons below Europace 6: 467-537.
- Vaddadi G, Guo L, Esler M, Socratous F, Schlaich M, et al. (2011) Recurrent postural vasovagal syncope: sympathetic nervous system phenotypes. See comment in PubMed Commons below CircArrhythmElectrophysiol 4: 711-718.
- Anderson JB, Czosek RJ, Knilans TK, Marino BS (2012) The effect of paediatric syncope on health-related quality of life. See comment in PubMed Commons below Cardiol Young 22: 583-588.
- Hyphantis TN, Pappas AI, Vlahos AP, Carvalho AF, Levenson JL, et al. (2012) Depressive symptoms and neurocardiogenic syncope in children: a 2-year prospective study. See comment in PubMed Commons below Pediatrics 130: 906-913.
- Blount RL, Morris JA, Cheng PS (2004) Parent and child psychological factors in pediatric syncope and other somatic symptoms. Journal of Consulting and Clinical Psychology 72: 597-604.
- Byars KC, Brown RT, Campbell RM, Hobbs SA (2000) Psychological adjustment and coping in a population of children with recurrent syncope. See comment in PubMed Commons below J DevBehavPediatr 21: 189-197.
- Frigerio A, Rucci P, Goodman R, Ammaniti M, Carlet O, et al. (2009) Prevalence and correlates of mental disorders among adolescents in Italy: the PrISMA study. See comment in PubMed Commons below Eur Child Adolesc Psychiatry 18: 217-226.
- Roskam I, Stievenart M, Tessier R, Muntean A, Escobar MJ, et al. (2014) Another way of thinking about ADHD: the predictive role of early attachment deprivation in adolescents' level of symptoms. See comment in PubMed Commons below Soc Psychiatry PsychiatrEpidemiol 49: 133-144.
- Crijnen AAM, Achenback TM, Verhulst FC (1997) Comparisons of problems reported by parents of children in 12 cultures: Total problems, externalizing and internalizing. Journal of the American Academy of Child and Adolescent Psychiatry 36: 1269-1277.
- Weine AM, Phillips JS, Achenbach TM (1995) Behavioral and emotional problems among Chinese and American children: parent and teacher reports for ages 6 to 13. See comment in PubMed Commons below J Abnorm Child Psychol 23: 619-639.
- Calkins SD, Graziano PA, Keane SP (2007) Cardiac vagal regulation differentiates among children at risk for behavior problems. See comment in PubMed Commons below BiolPsychol 74: 144-153.
- Frigerio A, Cattaneo C, Cataldo MG (2004) Behavioral and Emotional Problems Among Italian Children and Adolescents Aged 4 to 18 Years as Reported by Parents and Teachers. European Journal of Psychological Assessment 20: 124-133.
- American Psychiatric Association (1996) DSM-IV. Manualediagnostico e statisticodeidisturbimentali. Milano: Masson.
- World Health Organization, ICD-10 (1992) Classification of Mental and Behavioural Disorders Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization.
- De Los Reyes A, Kazdin AE (2004) Measuring informant discrepancies in clinical child research. See comment in PubMed Commons below Psychol Assess 16: 330-334.
- De Los Reyes A, Kazdin AE (2005) Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin 131: 483-509.
- Raucci U, Di Pietro P, Longhi R (2009) La sincope in etàpediatrica, lineeguida a cura di SIP, SIMEUP, SICP, FMSI, AIAC, SIC Sport, FIMP, GSCP, GSMESPO, SINPIA, LICE, SINC, SINP. Prospettive in Pediatria 39: 180-195.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 17334
- [From(publication date):
October-2014 - Aug 16, 2025] - Breakdown by view type
- HTML page views : 12623
- PDF downloads : 4711