Effectiveness of Balloon Kyphoplasty in Patients with Painful Vertebral Compression Fractures
Received: 19-May-2018 / Accepted Date: 25-May-2018 / Published Date: 01-Jun-2018 DOI: 10.4172/2167-0846.1000323
Abstract
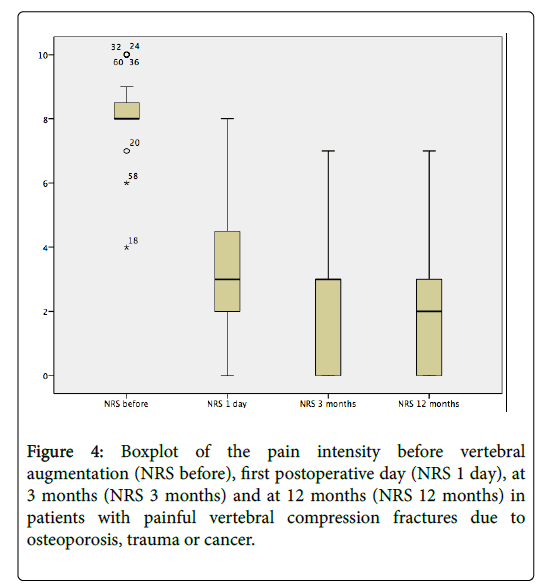
We performed a case series study on the effectiveness of balloon kyphoplasty (BKP) for painful vertebral compression fractures in 60 patients with acute axial lumbar and/or thoracic spinal pain due to osteoporosis, trauma or cancer, who were referred to the pain center of a general hospital. The pain intensity levels appeared to be statistically significant different between the pain level at baseline (T0) and the three moments of measurement (T1, T2, T3) after the procedure, p<0.001. No statistically significant difference in Numerical Rating Scale (NRS) for pain was found between the three moments of measurement after the procedure. No statistically significant difference in NRS for pain was found between the patients with osteoporosis and those with cancer between T0 and T1 (p=0.48). This study shows that in patients with painful (non) malignant vertebral compression fractures BKP can result in a statistically and clinically significant pain reduction lasting at least one year. There is a need for new high quality studies to define the place of BKP in patients with acute axial back pain due to vertebral compression fractures.
Keywords: Balloon vertebroplasty; Vertebrogenic compression fracture; Osteoporotic fracture; Mechanical low back pain
Introduction
Vertebral fractures often are very painful and lead to reduced quality of life and disability [1]. Common causes of vertebral fractures are osteoporosis (postmenopausal, secondary), trauma, primary tumors of the spine and metastasis. The worldwide burden of osteoporotic fractures in the year 2000 was estimated to be 9 million, among them 1.4 million clinical vertebral fractures [2]; about a third come to medical attention [3,4]. The incidence of osteoporotic clinical vertebral fractures in the Netherlands was estimated to be 0.7% in women and 0.2% in men aged 55 years or older [5]. Traumatic spinal fractures occur in 11.8 to 16.4 per 100000 populations (0.012-0.016%) [6,7]; the most common causes are a high-energy fall (39%, evenly distributed over the whole spine) and traffic accidents (26.5%, more fractures at the cervical and thoracic spine) [8]. The spine is also the most frequent site of bone metastasis. Spinal involvement may occur in up to 40% of patients with cancer and approximately 70% of patients with cancer have evidence of metastatic disease at the time of their deaths [9]. As many as 75% of vertebral metastases occur in patients with carcinoma of the breast, kidney, lung, prostate, thyroid and multiple myeloma [10,11].
Vertebral compression fractures occur in 55 to 70% of patients with multiple myeloma and are the initial clinical sign in 34 to 64% of these patients. Usual treatment for vertebral osteoporotic compression fractures consists out of analgesics, bed rest, casting and physical support. Other modalities were introduced depending on the clinical presentation and spinal level, aiming at the vertebra itself (e.g. radiotherapy, surgical approaches and/or cement augmentation). Cement augmentation evolved into a percutaneous technique, injecting cement into the fractured vertebral body. Balloon kyphoplasty (BKP) seems to be a safe, minimally invasive procedure for the treatment of painful vertebral fractures, which is intended to reduce pain and disability and correct vertebral body deformity using balloons [12-18]. Studies have demonstrated that cement augmentation procedures provide better clinical outcome compared to non-surgical management [19]. When comparing BKP with vertebroplasty (VP), the first proved to have better results, which are maintained over long-term follow-up [20-23], with less side effects such as cement leakage [24]. In patients with cancer, BKP proved to be an effective and safe treatment that rapidly reduces pain and improves function [25-31]; a biopsy can routinely be performed [32]. Comparing to surgery, percutaneous cement treatment predicts significantly reduced costs as well as length of stay [33,34]. The use of BKP or VP in the management of vertebral compression fractures in patients with cancer may be a cost-effective strategy [35].
In 2009, two articles appeared in the New England Journal of Medicine, reporting that improvements made in pain (and pain related disability) by VP in patients with painful vertebral osteoporotic compression fractures were similar in the treatment group and the sham group [36,37]. The results of these trials seem to be in disagreement with the accumulated literature on this subject [38]. In one study [36], MRIs and/or bone scans were not required if the fracture was known and under one year of age. The targeted level was 250 patients, but only 131 subjects were enrolled. Eight patients (12%) in the vertebroplasty group crossed over to the sham group, while 27 (43%) of patients in the sham group crossed over to the vertebroplasty group. In the other study [38], out of 219 eligible patients, only 78 (36%) were enrolled. While being a multicenter trial, more than 67% of the patients came from a single site. The mean volume injected into the vertebrae was (only) 2.8 mL. A meta-analysis of the individual patient data in the two randomized placebo controlled trials (RCTs) failed to show an advantage of VP over placebo [39]. More discussion regarding the differences between placebo efficacy and specific efficacy was provided in another article by Miller, Kallmes and Buchbinder [40].
Complications associated with BKP are attributed to the technique itself (e.g. cement leakage, infection) and/or cardiopulmonary events (e.g. cement, fat, bone marrow or air embolisation). These major complications are rarely seen, but may warrant a high level of suspicion and immediate action, e.g. early surgical intervention and/or pharmacological treatment [41-47]. This case series study reports on pain reduction after BKP in patients with painful vertebral compression fractures due to osteoporosis, trauma or cancer, who were referred to the pain center of a general hospital. All BKP procedures were performed by experienced interventional pain physicians.
Materials and Methods
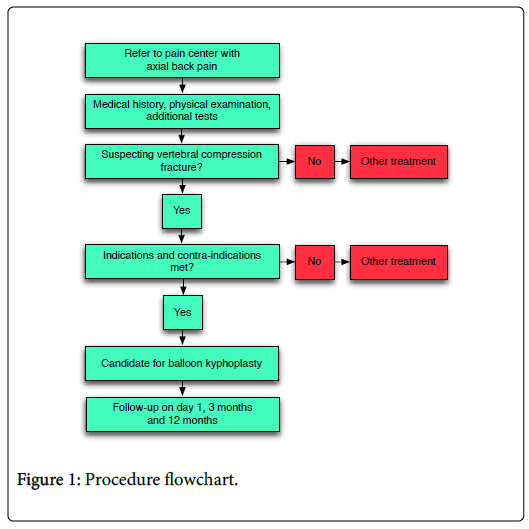
We performed a case series study on the effectiveness of BKP for painful vertebral compression fractures in 60 patients with acute axial lumbar and/or thoracic spinal pain. Patients were referred to the pain center of a general hospital with complaints of acute axial pain on lumbar and/or thoracic level. These patients were managed according to the flowchart presented in Figure 1. When a painful vertebral compression fracture was suspected (Table 1) and patients satisfied to the indications and contra-indications (Table 2), they were eligible for BKP. Each patient received a brochure explaining the complete procedure. After obtaining written informed consent for the procedure patients were scheduled for BKP.
| Medical history |
| 1. Acute (deep) spinal pain episode 2. Trauma 3. Most comfortable when motionless 4. Osteoporosis 5. Cancer 6. Previous vertebral compression fracture(s) 7. Persistent pain after acute pain episode subsided 8. Abdominal symptoms (early satiety, abdominal bloating) 9. Anorexia and subsequent weight loss 10. Lower rib syndrome 11. Inactive, sedentary lifestyle 12. Fear of falling 13. Sleep pattern disturbed (due to pain and inactivity) 14. Depression |
| Physical examination |
| 1. Tenderness to deep palpation and percussion over the affected vertebra 2. Para spinal muscle spasm 3. Short thoracic spine, kyphosis 4. Decreased pulmonary function (restrictive lung disease and reduced vital capacity) |
| Additional tests |
| 1. Lateral X-ray of spine 2. MRI |
Table 1: Medical history, physical examination and additional tests used in establishing the diagnosis of painful vertebral compression fractures.
| Indications |
| 1. Medical history, physical examination and additional tests suggestive of painful vertebral compression fracture on lumbar and/or thoracic level 2. Vertebral edema present on MRI 3. Numerical Rating Scale equal to or higher than 4/10 4. Preoperative anesthetic screening warrents the use of continuous IV sedation and analgesia |
| Contra-indications |
| 1. Active infection 2. Progressive neurological deficits 3. Major psychiatric disorder (according to psychiatrists opinion) 4. Anticoagulation cannot be stopped 5. Allergies to any medication or cement 6. Pregnancy 7. Contra-indication for MRI |
Table 2: Indications and contra-indications for balloon kyphoplasty.
Monitoring of vital parameters took place according to the American Society of Anesthesiologists [48] House of Delegates Standards for Basic Anesthetic Monitoring (ASA). Antibiotic prophylaxis was provided with Cephazolin 2 g. Continuous Oxygen 15 L/min through a non-rebreather mask and bag was applied and patients were placed in the prone position using pillows under the chest and pelvic area. Continuous sedation with intravenous (IV) propofol Target Controlled Infusion (TCI) 0.5 μg/mL and continuous analgesia with IV remifentanyl 0.05 μg/kg/min was used. Doses were titrated to a Ramsay score of 4 out of 6 [49]. Continuous IV sedation and analgesia was provided to the patient by a nurse anaesthetist with subsequent training in sedation.
Skin and periosteal infiltration was performed at each side with Lidocaine 2%. Under fluoroscopic guidance, a bilateral trans- or extrapedicular approach was used with introducer tools and inflatable balloon-like devices, polymethylmethacrylate (PMMA) bone cement and delivery devices (Kyphon inc./Medtronic Spine LLC, 1221 Crossman Ave, Sunnyvale, CA 94089, United States of America). During each procedure, a biopsy was taken and a combination of Paracetamol 1 g IV, Dynastat 40 mg IV and Morphine 0.1 mg/kg IV was given for immediate postoperative pain management. Wound edges were infiltrated with Ropivacaine 0.2%.
The main outcome parameter was pain reduction (Numerical Rating Scale (NRS) for pain) [50-55]. The 0-10 verbal NRS for pain is a tool that enjoys widespread clinical use due to its ease of administration. While using the NRS for pain, patients are asked to rate their pain on a scale from 0 to 10, where 0 represents "no pain" and 10 represents "the worst pain possible," using whole numbers (11 integers including zero). Often the value of "4" is used to confirm clinical nursing judgment as to the need for further intervention or documentation that the patient's goals for analgesia have been achieved. The NRS for pain was measured preoperatively (T0) and during follow-up.
Time periods for follow-up were on the first postoperative day (T1), at 3 months (T2) and at 12 months (T3). Descriptive statistics were used to determine the frequencies of the demographic and the outcome parameters. Differences in pain level between baseline (preoperative, T0) and postoperative (T1, T2 and T3) time periods were analyzed using the related-samples Friedman’s Two-Way Analysis of Variance by Ranks. Post-hoc pairwise comparisons were performed with the Related Samples Wilcoxon Signed Rank Test, using a Bonferroni correction to counteract the problem of multiple comparisons. The independent-samples Mann-Whitney U test was used to study the hypothesis that the distribution of the NRS for pain scores (T0-T1) is the same in the patients with osteoporosis and those with cancer. Data were analyzed using SPSS for Mac, version 22 (International Business Machines (IBM) Corporation, Software Group, Route 100, Somers, NY, 10589, United States of America).
Results
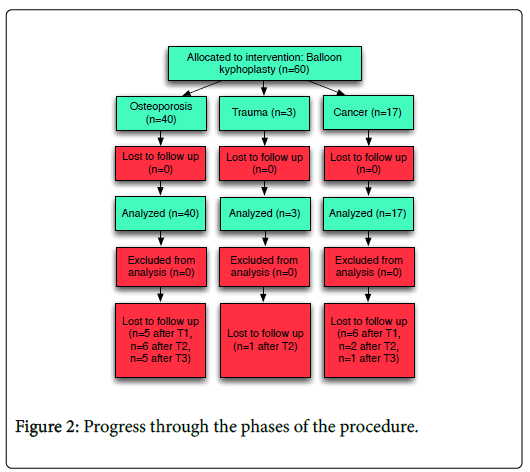
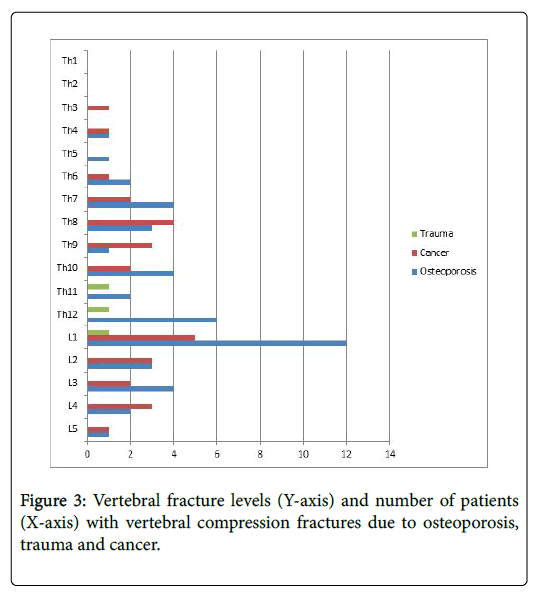
Sixty patients were treated with BKP for painful vertebral compression fractures and had follow-up for 1 year. The procedure is presented in Figure 2. Demographic data are presented in Table 3. Using the Kolmogorov-Smirnov test, the distributions of these parameters appeared to be skewed. Therefore, central tendency and dispersion of the distributions are reported as median and interquartile range (IQR). Vertebral fracture levels are presented in Figure 3. Most fractures occurred at the Th12-L1 region. The pain intensity levels appeared to be statistically significant different between the pain level at baseline (T0) and the three moments of measurement after the procedure, p<0.001 (Figure 4). No statistically significant difference was found between the three moments of measurement after the procedure. Results of the pairwise comparisons are presented in Table 4.
| Group | N (F, %) | Age | BMI | ||
|---|---|---|---|---|---|
| Median | IQR (Q3-Q1) | Median | IQR (Q3-Q1) | ||
| Osteoporosis | 40 (28, 70) | 77 | 16 | 26 | 7.3 |
| Trauma | 3 (2, 66.7) | 59 | N/A | 27.9 | N/A |
| Cancer | 17 (10, 58.8) | 71 | 11 | 22.8 | 10.3 |
Table 3: Demographic data of the patients (100% Caucasian) in the study (IQR: Interquartile range; N: number of patients; F: Female).
| T0 | T1 | T2 | |
|---|---|---|---|
| T0 | |||
| T1 | <0.001 | ||
| T2 | <0.001 | 0.41 | |
| T3 | <0.001 | 0.12 | 0.43 |
Table 4: Results (P-value) of the pairwise comparisons between the moments of measurement, using a Bonferroni correction (α=0.08) (T0=before the BKP procedure; T1=first postoperative day; T2=3 months after treatment; T3=12 months after treatment).
In 40 patients, a painful vertebral compression fracture was present due to osteoporosis, in three patients due to trauma and in 17 patients due to cancer (five patients with multiple myeloma, six with metastatic lung cancer, two with metastatic breast cancer, two with metastatic prostate cancer, one with metastatic ovary cancer and one with metastatic cervix cancer). No statistically significant difference in NRS for pain was found between the patients with osteoporosis and those with cancer between T0 and T1 (p=0.48).
In the patients with cancer, one patient died after one day, another ten within one month and another two within three months. In the patients with osteoporosis, one patient died within one month and another one within three months. In the patients with traumatic vertebral compression fracture, no one died within the follow-up period of 1 year. No major complications occurred as a direct result from the BKP procedure.
Discussion
In this case series study, we measured the pre- and postoperative (until at least one year after operation) pain levels in 60 patients with painful vertebral compression fractures on lumbar and/or thoracic level due to osteoporosis, trauma or cancer, who were treated with BKP. The pain intensity levels appeared to be statistically significant different between the pain level at baseline and the three moments of measurement after the procedure. No statistically significant difference was found between the three moments of measurement after the procedure. No statistically significant difference in pain intensity was found between the patients with osteoporosis and those with cancer between baseline and the first postoperative day. One patient with cancer died within 1 day after the BKP procedure; the exact cause of death is unknown, more specifically a possible contribution to this death from the BKP procedure and/or the IV sedation.
In support of the recently published papers advocating the use of BKP for painful vertebral compression fractures in recent years, and contrary to two papers reporting no statistically significant difference of vertebroplasty compared to a sham control group, our case series study indicates that BKP can result in a statistically significant and sustained pain reduction during 1 year follow-up. This case series study has several limitations: 1) We didn’t include experimental control, and therefore cannot compare the treatment results with a control group, e.g. a placebo procedure; 2) Pain scores were measured during specific moments in time; we don’t know if using pain scores reflecting certain periods of time might lead to a different result; 3) Due to morbidity and mortality predominantly occurring in the group of patients with cancer, the number of missing data increased as time progressed.
Conclusion
This case series study shows that in patients with painful (non) malignant vertebral compression fractures BKP can result in a statistically and clinically significant pain reduction lasting at least one year. There is a need for new high quality studies to define the place of BKP in patients with acute axial back pain due to vertebral compression fractures.
Acknowledgements
The author wishes to thank Bravis hospital, Bergen op Zoom, The Netherlands, for its policy of tolerance (at the moment vertebral augmentation procedures are not reimbursed in the Netherlands) and Fleur A. Schuurmans, RN for her work in partly collecting the data. This manuscript also serves as part of the PhD thesis of the first author on minimally invasive for lumbar spine related pain disorders.
Competing interests
All authors declare that no support from any organisation for the submitted work has been received, no financial relationships with any organisations have been established that might have an interest in the submitted work and no other relationships or activities were established that could appear to have influenced the submitted work.
References
- Wardlaw D, Cummings SR, Meirhaeghe JV, Bastian L, Tillman JB, et al. (2009) Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): A randomised controlled trial. Lancet 373: 1016-1024.
- Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17: 1726-1733.
- Klazen CAH, Lohle PNM, Vries JD, Jansen FH, Tielbeek AV, et al. (2010) Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): An open-label randomised trial. Lancet 376: 1085-1092.
- Mazanec DJ, Podichetty VK, Mompoint A, Potnis A (2003) Vertebral compression fractures: Manage aggressively to prevent sequelae. Cleve Clin J Med 70: 147-156.
- Quality Institute for Healthcare CBO (2002). Osteoporosis second revised guideline. Van Zuiden communications B.V, Utrecht.
- Fredo HL, Rizvi SA, Lied B, Ronning P, Helseth E (2012) The epidemiology of traumatic cervical spine fractures: A prospective population study from Norway. Scand J Trauma Resusc Emerg Med 20: 85-91.
- Moradi-Lakeh M, Rasouli MR, Vaccaro AR, Saadat S, Zarei MR, et al. (2011) Burden of traumatic spine fractures in Tehran, Iran. BMC Public Health 11: 789-795.
- Leucht P, Fischer K, Muhr G, Mueller EJ (2009) Epidemiology of traumatic spine fractures. Injury 40: 166-172.
- Harrington K (1993) Metastatic tumors of the spine: diagnosis and treatment. J Am Acad Orthop Surg 1: 76-86.
- Schaberg J, Gainor BJ (1985) A profile of metastatic carcinoma of the spine. Spine 10: 19-20.
- Wong DA, Fornasier VL, MacNab I (1990) Spinal metastasis: The obvious, the occult, and the imposters. Spine 15: 1-4.
- Van Meirhaege J, Bastian L, Boonen S, Ranstam J, Tillman JB, et al. (2013) A randomized trial of balloon kyphoplasty and nonsurgical management for treating acute vertebral compression fractures. Spine 38: 971-983.
- Diel P, Reuss W, Aghayev E, Moulin P, Roder C, et al. (2010) SWISSspine-a nationwide health technology assessment registry for balloon kyphoplasty: Methodology and first results. Spine J 10: 961-71.
- Health quality ontario (2016) Vertebral augmentation involving vertebroplasty or kyphoplasty for cancer-related vertebral compression fractures: A systematic review. Ont Health Technol Assess Ser 16: 1-202.
- Chen H, Yang H, Jia P, Bao L, Tang H (2016) Effectiveness of kyphoplasty in the treatment of osteoporotic vertebral compression fracture patients with chronic kidney disease. J Orthop Sci 21: 571-578.
- Sonmez E, Comert S, Akdur A, Karakaya E, Gulsen S, et al. (2016) Balloon kyphoplasty is a safe and effective option for the treatment of vertebral compression fractures in solid-organ transplant recipients. Exp Clin Transplant.
- Liu J, Li X, Tang D, Cui X, Li X, et al. (2013) Comparing pain reduction following vertebroplasty and conservative treatment for osteoporotic vertebral compression fractures: A meta-analysis of randomized controlled trials. Pain Physician 16: 455-464.
- Lee HM, Park SY, Lee SH, Suh SQ, Hong JY (2012) Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCF’s): Conservative treatment versus balloon kyphoplasty. Spine J 12: 998-1005.
- Boonen S, Van Meirhaeghe J, Bastian L, Cummings SR, Ranstam J, et al. (2011) Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res 26: 1627-1637.
- Bozkurt M, Kahilogullari G, Ozdemir M, Ozgura O, Attar A, et al. (2014) Comparitive analysis of vertebroplasty and kyphoplasty for osteoporotic vertebral compression fractures. Asian Spine J 8: 27-34.
- Kumar K, Nguyen R, Bishop S (2010) A comparitive analysis of the results of vertebroplasty and kyphoplasty in osteoporotic vertebral compression fractures. Neurosurgery 67: 171-188.
- Zhao G, Liu X, Li F (2016) Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fractures (OVCFs). Osteoporos Int 27: 2823-2834.
- Liang L, Chen X, Jiang W, Li X, Chen J, et al. (2016) Balloon kyphoplasty or percutaneous vertebroplasty for osteoporotic vertebral compression fracture? An updated systematic review and meta-analysis. Ann Saudi Med 36: 165-174.
- Hsieh MK, Chen LH, Chen WJ (2013) Current concepts of percutaneous balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures: Evidnce-based review. Biomed J 36: 154-161.
- Berenson J, Pflugmacher R, Jarzem P, Zonder J, Schechtman K, et al. (2011) Balloon kyphoplasty versus non-surgical management for treatment of painful vertebral body compression fractures in patients with cancer: A multicenter, randomised controlled trial. Lancet Oncol 12: 225-235.
- Lykomitros V, Anagnostidis KS, Alzeer Z, Kapetanos GA (2010) Percutaneous anterolateral balloon kyphoplasty for metastatic lytic lesions of the cervical spine. Eur Spine J 19: 1948-1952.
- Eleraky M, Papanastassio I, Setzer M, Baaj AA, Tran ND, et al. (2011) Balloon kyphoplasty in the treatment of metastatic tumors of the upper thoracic spine. J Neurosurg Spine 14: 372-376.
- Dalbayrak S, Onen MR, Yilmaz M, Naderi S (2010) Clinical and radiographic results of balloon kyphoplasty for treatment of vertebral body metastases and multiple myelomas. J Clin Neurosci 17: 219-224.
- Huber FX, McArthur N, Tanner M, Gritzbach B, Schoierer O, et al. (2009) Kyphoplasty for patients with multiple myeloma is a safe surgical procedure: Results from a large patient cohor. Clin Lymphoma Myeloma 9: 375-380.
- Wang Y, Liu H, Pi B, Yang H, Qian Z, et al. (2016) Clinical evaluation of percutaneous kyphoplasty in the treatment of osteolytic and osteoblastic metastatic vertebral lesions. Int J Surg 30: 161-165.
- Chen F, Xia YH, Cao WZ, Shan W, Gao Y, et al. (2016) Percutaneous kyphoplasty for the treatment of spinal metastases. Oncol Lett 11: 1799-1806.
- Papanastassiou ID, Aghayev K, Berenson JR, Schmidt MH, Vrionis FD (2012) Is vertebral augmentation the right choice for cancer patients with painful vertebral compression fractures? J Natl Compr Canc Netw 10: 715-719.
- Itagaki MW, Talenfeld AD, Kwan SW, Brunner JW, Mortell KE, et al. (2012) Percutaneous vertebroplasty and kyphoplasty for pathologic vertebral fractures in the Medicare population: Safer and less expensive than open surgery. J Vasc Interv Radiol 23: 1423-1429.
- Flug J, Hanford A, Ortiz O (2013) Vertebral augmentation versus conservative therapy for emergently admitted vertebral compression deformities: an economic analysis. Pain Physician 16: 441-445.
- Health Quality Ontario (2016) Vertebral augmentation involving vertebroplasty or kyphoplasty for cancer-related vertebral compression fractures: An economic analysis. Ont Health Technol Assess Ser 16: 1-34.
- Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, et al. (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361: 569-579.
- Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, et al. (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361: 557-568.
- Society of Interventional Radiology. Commentary on vertebroplasty and the august studies in the New England Journal of Medicine.
- Staples MP, Kallmes DF, Comstock BA, Jarvik JG, Osborne RH, et al. (2011) Effectiveness of vertebroplasty using individual patient data from two randomised placebo controlled trials: Meta-analysis. BMJ 343: d3952.
- Miller FG, Kallmes DF, Buchbinder R (2011) Vertebroplasty and the placebo response. Radiology 259: 621-625.
- Katonis P, Hadjipavlou A, Souvatzis X, Tzermiadianos M, Alpantaki K, et al. (2012) Respiratory effects, hemodynamic changes and cement leakage during multilevel cement balloon kyphoplasty. Eur Spine J 21: 1860-1866.
- Tran I, Gerckens U, Remig J, Zinti G, Textor J (2013) First report of a life-threatening cardiac complication after percutaneous balloon kyphoplasty. Spine 1: E316-E318.
- Schulz C, Efinger K, Schwarz W, Mauer UM (2012) Experiences with cement leakage after balloon kyphoplasty. Orthopade 41: 881-888.
- Tins BJ, Cassar-Pullicino VN, Lalam R, Haddaway M (2012) Venous air embolism in consecutive balloon kyphoplasties visualised on CT imagin. Skeletal Radiol 41: 1093-1098.
- Walter J, Haciyakupoglu E, Waschke A, Kalff R, Ewald C (2012) Cement leakage as a possible complication of balloon kyphoplasty-is there a difference between osteoporotic compression fractures (AO type A1) and incomplete burst fractures (AO type A3.1)? Acta Neurochir 154: 313-319.
- Audat ZA, Alfawareh MD, Darwish FT, Alomari AA (2016) Intracardiac leakage of cement during kyphoplasty and vertebroplasty: A case report. Am J Case Rep 17: 326-330.
- Ge CY, He LM, Zheng YH, Liu TJ, Guo H, et al. (20016) Tuberculous spondylitis following kyphoplasty: A case report and review of the literature. Medicine 95: e2940.
- American Society of Anesthesiologists House of Delegates: Standards for Basic Anesthetic Monitoring.
- Ramsay MAE, Savege TM, Simpson BR, Goodwin R (1974) Controlled sedation with Alphaxalone-Alphadolone. Br Med J 2: 656-659.
- Breivik EK, Bjornsson GA, Skovlund E (2000) A comparison of pain rating scales by sampling from clinical trial data. Clin J Pain 16: 22-28.
- Grotle M, Brox JI, Vollestad NK (2004) Concurrent comparison of responsiveness in pain and functional status meaurement used for patients with low back pain. Spine 29: E492-E501.
- van der Roer N, Ostelo RW, Bekkering GE, van Tulder MW, de Vet HC (2006) Minimal clinically important change for pain intensity, funtional status, and general health status in patients with nonspecific low back pain. Spine 31: 578-582.
- Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM (2001) Clinical importance of changes in chronic pain intensity measured on a 11-point numerical pain rating scale. Pain 94: 149-158.
- Childs JD, Piva SR, Fritz JM (2005) Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 30: 1331-1334.
- van Tilburg CWJ (2017) Minimally invasive treatment for lumbar spine related pain disorders.
Citation: van Tilburg CWJ, Groeneweg JG, Stronks DL, Huygen FJPM (2018) Effectiveness of Balloon Kyphoplasty in Patients with Painful Vertebral Compression Fractures. J Pain Relief 7: 323. DOI: 10.4172/2167-0846.1000323
Copyright: © 2018 van Tilburg CWJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7433
- [From(publication date): 0-2018 - Nov 23, 2025]
- Breakdown by view type
- HTML page views: 6462
- PDF downloads: 971