Effects of Superficial and Deep Dry Needling on Pain and Muscle Thickness in Subject with Upper Trapezius Muscle Myofascial Pain Syndrome
Received: 14-May-2018 / Accepted Date: 21-May-2018 / Published Date: 28-May-2018 DOI: 10.4172/2167-0846.1000322
Abstract
Background: Dry needling is one of the main therapeutic approaches in patients with Myofascial pain syndrome. Few studies have been compared the superficial and deep dry needling methods in these patients.
Objective: To evaluate the effects of superficial and deep dry needling on pain and muscle thickness in subjects with upper trapezius myofascial pain syndrome.
Design: A randomized quasi-experimental double-blinded trial.
Methods: 50 subjects with upper trapezius myofascial pain syndrome (age=26/08 ± 4/62, weight=63/88 ± 8/71 kg, height=167/7 ± 4/82 cm, pain duration=9/75 ± 7/05 m) randomly assigned to the superficial (n=25) and deep (n=25) dry needling groups. The pain and maximum thickness of upper trapezius muscle in rest, fair and normal contractions were measured by visual analogue scale (VAS) and an ultrasound device respectively before and after the intervention as well as 7 and 15 days follow-up.
Results: The mixed-model ANOVAs revealed a significant group-by-time interaction (F=44.03, p<0.001) for pain and muscle thickness in rest (F=67.00, p<0.001), fair (F=108.73, p<0.001) and normal contraction (F=17.73, p<0.001). The main effects of group and time were statistically significant for pain, rest, fair and normal muscle thickness (p<0.001). There were not any significant differences in rest, fair and normal muscle thickness after intervention as well as 7 and 15 days follow-up.
Conclusion: Both superficial and deep dry needling techniques induced significant short-term changes in the VAS. Muscle thickness in rest, fair and normal contractions did not show any significant changes between the groups.
Keywords: Myofascial pain syndrome; Physical therapy modalities; Ultrasonography; Neck pain
Introduction
Approximately, 95% of patients with chronic pain have myofascial pain syndrome [1]. This syndrome has involved millions of people and has a high economic cost for people and communities [2]. One of the main treatments of this syndrome is the use of dry needling, which is performed by different methods such as superficial, deep and fascia [3-5].
Dry needling has been suggested as a valid therapeutic approach in subjects with myofascial pain syndrome. Although many studies have compared the needling methods of Chinese medicine (Acupuncture), few studies have been compared Superficial Dry Needling (SDN) and Deep Dry Needling (DDN) [6-9]. As well, the effects of these methods have been studied mostly on pain, pressure pain threshold and range of motion [10-13]. Since these methods are different in the mechanisms of the effects, depth of penetration, and especially later complications, finding a method with greater improvement in pain and muscle function could be useful to determine a more effective treatment.
Changes in muscle thickness have been considered as a critical clinical outcome after treatment in patients with myofascial pain syndrome [14,15]. In the present study, assessment of muscle thickness in rest and contraction modes after SDN and DDN methods is a new perspective expanding in recent studies [16]. Therefore, the purpose of this clinical trial was to determine the effects of SDN and DDN methods on pain intensity and muscle thickness in individuals with upper trapezius myofascial pain syndrome.
Methods
Study design and population
The present study was a quasi-experimental study in which 50 subjects (18 men, 32 women) aged 20 to 36 years (mean ± standard deviation (SD): 25.68 ± 4.39 y) with myofascial pain syndrome of upper trapezius were recruited from a general hospital and an outpatient clinic. The variables included pain and muscle thickness in three situations: Rest position, fair and normal contractions of the muscle.
Inclusion criteria in this study were: Presence of at least one active trigger point in the central region of upper trapezius, age between 20 and 40 years, pain duration ≥ 3 months and diagnosis of myofascial pain syndrome based on clinical examinations. Also, the subject’s exclusion criteria were: Fibromyalgia, thoracic outlet syndrome, upper extremity entrapment syndromes, severe joints immobility, and torticoli. Moreover, participants with history of rheumatoid arthritis, cancer, and surgical interventions in the neck and shoulder, and other regions of the trunk were also excluded. Additionally, participants who had received physical therapy or any local injection within the last 3 month were excluded.
At first, the subjects filled the consent and the personal information questionnaire forms. The subjects were evaluated at the first session and then were treated by 3 sessions of dry needling and re-evaluated after treatment and 7 and 15 days follow-up.
Clinical Examination
The diagnosis of the myofascial pain syndrome was based on standard clinical criteria including: (1) palpable taut bands in upper trapezius muscle, (2) local tenderness in the taut bands (trigger points), and (3) pain recognition by the subjects [3,15]. The presence or absence of the active or latent TrPs in the upper trapezius muscle recognized by the examiner. Spontaneous pain, acute tenderness and developing of referral pain by palpation are three main features of active TrPs [17].
Interventions
The patients were randomly assigned to the superficial (n=25) and deep (n=25) dry needling groups. Randomization was based on random number table. Odd numbers allocated in SDN group and even numbers in DDN group. Notably, for each intervention, both patients and investigators were blinded. All evaluation and treatment process were performed by two independent physiotherapists.
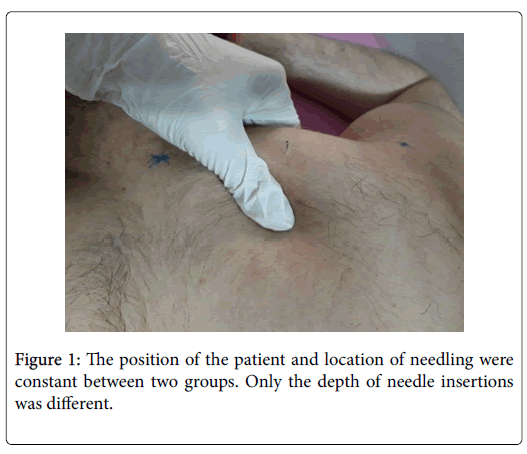
To carry out the dry needling procedures, the patient was asked to lie prone as the hands were placed under the forehead. To insure the fixed position of the trigger point in the treatment sessions, nonmuscular sites, including 7 cervical vertebral spinous process and acromion were used. The C7 spinous process was found through flexion-extension method of the cervical spine and then the examiner drew a line between C7 and acromion process and marked the midpoint of this line [18]. All measurement and treatment methods were performed on this point that is the primary point of upper trapezius muscle trigger points. The alcohol solution was used to disinfect the area, and the examiner used sterile latex gloves. For the DDN group, a needle with 50 mm long and 0.25 mm in diameter and for the SDN group, a needle with a length of 20 mm and a diameter of 0.25 mm were used. In the SDN group, the needle penetrated only up to 5 mm (distance of the needle from the plastic tube) for each subject but in the DDN group the needle inserted into the trigger point. It should be noted that the type and country of manufacture as well as the diameter of needles and the place of needling were the same in the two groups. After recognizing the location of the trigger point by the touch, the second and third fingers of the non-dominant hand of the therapist were held at the trigger point and then, by the dominant hand of the therapist, the needle was inserted into the skin and slightly penetrated into the trigger point (Figure 1). Eliciting a local twitch response confirmed the proper insertion of needles in DDN group. From this moment, the needle was inserted 8 times by fast moving back and forth without getting out of the skin and after the last blow was remained in the place for 5 minutes.
Outcome measures
Pain assessment
In order to evaluate the pain intensity, a visual analogue scale (VAS) by marking the 10 cm lines was used. The pain level that the subjects experienced before, after treatment and 7 and 15 days follow-up was recorded.
Ultrasound evaluation
All subjects were evaluated using ultrasound with 5-10 MHz linear probe. At the beginning, the examiner identified the longitudinal view of upper trapezius muscle clearly. Then the closest vertical distance between superior and inferior high echogenic borders of the muscle, in the center of the image, was calculated as muscle thickness. Position of the patient, the way of placing the probe and the method of muscle thickness measurements were based on the last published article. Rest, fair and normal contraction conditions based on manual muscle testing grading system (head and neck combined extension and rotation to the same side) were used to measure the muscle thickness by ultrasound (Table 1) [19].
| Contractile degree | Position of the subject | Position of the examiner | Level of muscle activity |
|---|---|---|---|
| Rest | Prone, head on the bed, hands near the body | Standing along the upper trunk | The patient does not move the head and neck. |
| Fair | Prone, head out of the bed, hands near the body | Standing next to the patient's head | The patient lifts head and neck opposite to the gravity and looks up |
| Normal | Prone, head on the bed, hands near the body | Standing next to the patient's head, One hand on the parieto-occipitalis area for putting resistance to the head | The patient moves the head and neck in the range upward opposite to the maximum resistance. |
Table 1: Measurement conditions of upper trapezius muscle thickness by ultrasound.
Statistical analysis
The sample size calculation was based on mean and SD of VAS scores of the recent study. In the mentioned study, the main dependent variable was pain (measured by the VAS). Before and after 1 month treatment, the mean VAS score ± SD were 5.3 ± 1.5 and 2.1 ± 1.6 respectively. The alpha level was assumed 0.05 and power of 80% with a ratio of the sample size of the two groups being 1. According to the formula (n=(Zα/2+Zβ) 2 × 2 × σ2/d2) the sample size was 21 for each group. Finally by estimation of 10% missed data based on the formula (1/1-f) the sample size were calculated 25 subjects for each group.
Descriptive statistics, including mean and standard deviation (SD) values of all variables were computed for the SDN and DDN groups. The normality of distribution was evaluated by the Shapiro-Wilk test, and the results confirmed the use of parametric tests. A 2 × 4 (two groups: SDN and DDN; four times of measurements: Before and after 7 and 15 days of follow-up) mixed-model analyses of variance (ANOVAs) were conducted for pain and thickness parameters. Posthoc analyses were performed using multiple comparison by Bonferroni’s method to indicate the interaction between group and time. In addition, the effect size was calculated as the differences in outcome measures between the two groups divided by the SD of the either groups. Significant level was set at 0.05 for all tests.
Results
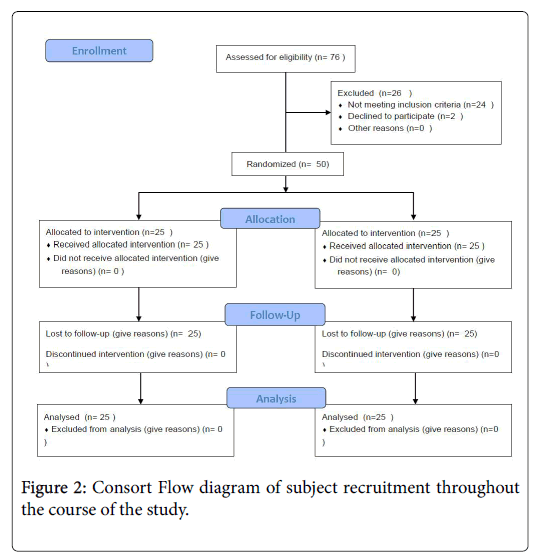
76 subjects were screened for eligibility. 26 were excluded: 24 were excluded because they did not meet the inclusion criteria and 2 declined to participate (Figure 2). Finally 50 subjects were treated, and 25 were assigned to the SDN group and 25 to the DDN group.
All muscle thickness measurements have been found to be reliable based on the mean of three scores of three conditions by ultrasound (ICC=0.75-0.98). Table 2 shows the mean and SD values of demographic characteristics, and the results of independent t-tests for the differences between the groups showed no statistical differences in the distribution of age, height, weight, and body mass index (p>0.05).
| Variables | SDN group (n=25) | DDN group (n=25) | P-Value | ||
| Mean | SD | Mean | SD | ||
| Age (year) | 26.08 | 4.32 | 25.28 | 4.5 | 0.52 |
| Height (cm) | 167.72 | 4.82 | 164.36 | 5.85 | 0.37 |
| Weight (kg) | 63.88 | 8.71 | 61.52 | 7.07 | 0.29 |
| Body mass index (kg/m2) | 22.68 | 2.82 | 22.74 | 2.13 | 0.93 |
Table 2: Mean and standard deviation (SD) of demographic variables in SDN and DDN groups. P-values are related to the result of independent t-test.
Table 3 shows the mean and SD of VAS, rest, fair and normal muscle thickness in the SDN and DDN groups at four times of measurements, including before and after interventions, as well as 7 and 15 days of follow-up. The mixed-model ANOVAs revealed a significant group-bytime interaction (F=44.03, p<0.001) for pain, in which the patients treated with SDN and DDN experienced a reduction of 20 and 39 mm, respectively from before to 15 days after interventions. The main effects of group and time were statistically significant for pain (p<0.001). The effect size of pain relief in SDN and DDN groups was 1.46 to 2.5 and 1. 64 to 4.68, respectively. The between group comparisons indicated that the DDN group had a greater reduction of pain intensity than the SDN group 7 days and 15 days after treatment (2.9 and 3.9 points less pain in the DDN group) (Table 4). Despite the 1.4 points pain reduction in the DDN group after intervention, it was not significant with pain reduction in the SDN group (1.2 points less pain).
| Dependent variables | SDN group | DDN group | |||||||
| Before | After | Follow 7 days | Follow 15 days | Before | After | Follow 7 days | Follow 15 days | ||
| VAS | mean | 5.2 | 3.94 | 3.32 | 3.2 | 5.06 | 3.66 | 2.12 | 1.08 |
| SD | 0.86 | 0.78 | 0.77 | 0.85 | 0.85 | 0.87 | 0.94 | 0.98 | |
| Rest thickness | Mean | 12.02 | 11.98 | 11.93 | 11.92 | 12.21 | 11.84 | 11.74 | 11.66 |
| SD | 1.98 | 1.97 | 1.96 | 1.95 | 1.64 | 1.65 | 1.65 | 1.66 | |
| Fair thickness | Mean | 13.18 | 13.15 | 13.11 | 13.06 | 13.09 | 12.77 | 12.68 | 12.6 |
| SD | 1.9 | 1.88 | 1.88 | 1.6 | 1.6 | 1.58 | 1.58 | 1.6 | |
| Normal thickness | Mean | 13.59 | 13.54 | 13.52 | 13.5 | 13.44 | 13.04 | 12.94 | 12.85 |
| SD | 1.91 | 1.91 | 1.91 | 1.92 | 1.42 | 1.43 | 1.44 | 1.43 | |
Table 3: Mean and SD of VAS, rest, fair and normal muscle thickness in SDN and DDN groups.
| VAS | Rest thickness | Fair thickness | Normal thickness | |
| F | P-Value | F | P-Value | |
| Main effect | ||||
| Group | 18.89 | <0.001 | 0.03 | 0.85 |
| Time | 360.79 | <0.001 | 132.49 | <0.001 |
| Interaction | ||||
| Group × Time | 44.03 | <0.001 | 67 | <0.001 |
Table 4: Results of two-way ANOVAs (Group × Time interactions) for VAS, rest, fair and normal muscle thickness: F ratios and P values by variable. (P-values equal or less than .05 are in bold).
The mixed-model ANOVAs revealed a significant group by time interaction for rest (F=67.00, p<0.001), fair (F=108.73, p<0.001) and normal (F=17.73, p<0.001) muscle thickness. The main effects of time were statistically significant for rest, fair and normal muscle thickness (p<0.001). The results of between group comparisons did not show any significant differences in rest, fair and normal muscle thickness after intervention and 7 and 15 days of follow-up (Table 4). Furthermore, the mean differences in the SDN group for rest, fair and normal muscle thickness from before to 15 days after Interventions were 0.1, 0.3 and 0.1, respectively. Otherwise, in the DDN group, the mean differences for rest, fair and normal muscle thickness were 0.5, 0.5 and 0.6, respectively (Table 3).
Discussion
The effect of SDN and DDN on pain
Intensity of pain is the main outcome studied in nearly all cases of myofascial pain syndrome. The minimum change in the intensity of pain that is clinically important is 12 mm for the VAS [20]. In the present study, the intensity of pain in the SDN group from pretreatment to follow-up period was reduced 20 mm, and in the DDN group was reduced 39 mm. IIbuldu et al. stated that the DDN had no significant effect on the reduction of pain in patients with myofascial pain syndrome of the upper trapezius muscle in short-term and longterm follow-up [21]. Moreover, Kamanli et al showed that the analgesic effects of injection of lidocaine and botulinum toxin were significantly higher in the short and long term compared to the DDN group [22]. It should be noted that in the mentioned researches, the syringe was used instead of the acupuncture needle. In addition, the local twitch response during the DDN was not considered, and the syringe was used in the pain point not in the main point of the muscle. In other studies, the short-term effects of pain relief are indicated by using superficial and deep dry needling methods [23,24].
One of the important indices for using DDN is mechanical stimulations of the trigger point. These mechanical stimulations include improved fiber structure, decreased local stiffness and improved blood circulation. Also, Mechanical stimulation seems to increase the production of smooth muscle actin and improve the repair of fascia in damaged areas [25]. On the other hand, the needle may also be able to fix the homeostasis in fascia by damaging additional collagenous connections, and consequently, reduce tension in the connective tissue. In the SDN method, the mechanical stimulation is very small and only under the surface of the skin which does not hit the trigger points. So, it is not highly effective in the SDN method.
To explain the reduction of pain in the SDN, elimination of tight muscle fibers and resolution of the energy crisis have been mentioned [26]. By the DDN, there was no significant difference in pain reduction compared to the SDN in the short-term, which may be due to destruction and inflammation of the tissue and increase of the secondary pain. However, in the long term, with the reduction of inflammation, the needle entrance into the trigger points causes changes in muscle structure and increases blood supply to the area [27]. Therefore, the long-term effects of DDN on pain reduction were more than the SDN. SDN is a quick and painless method for pain relief. It is indicated that the main mechanism of SDN in reducing pain is stimulation of A delta fibers and inhibition of C fibers through posterior horn of the spinal cord. Since stimulation of A delta fibers induces a sharp and transient pain and due to the fact that the SDN does not cause too much pain during the procedure, then other mechanisms, including increased skin circulation, effects on the limbic system, as well as stimulation of the A beta fibers should be considered.
From the clinical point of view, the ability of needling to increase circulation about twice in the main area of the trigger points is highly desirable [28]. In the SDN, increasing blood circulation does not occur in deep tissue and maybe it is one of the reasons that its effect is less than the DDN method in reducing pain in the long term. Apart from the depth of the needle issue, another effective factor in the therapeutic consequences of DDN is the local twitch response of the muscle. Local twitch response of the muscle causes changes in blood circulation, as well as improvement of ischemia, hypoxia, and increased pain mediators, such as substance P and calcitonin peptide due to stimulation of C and A delta fibers by axonal reflex. In this study, the patients treated with DDN showed local twitch response in the affected muscle. In contrast, in the SDN method, despite the therapeutic effects, no local twitch response was elicited. It seems that developing or not developing a local twitch response in muscle is an issue needing further investigations [29].
Effects of SDN and DDN on Rest, Fair and Normal Muscle Thickness
Although, in the present study, thickness of the muscle in the DDN group was reduced compared to the SDN group after treatment, and the follow-up period, the reduction was not significant between the two groups (0.5 mm). On the other hand, the maximum slope of muscle thickness reduction in the three modes was in the DDN group, before and after the treatment. The reason may be the localized twitch response following the application of DDN [30].
Examination of the muscle thickness with ultrasound has been shown contradictory results in different muscles [31-33]. Change (decrease or increase) of muscle thickness in people with myofascial pain syndrome is a challenge needing further investigations [32-34]. Koppenhaver et al. in a recent study found that infraspinatus muscle thickness (in rest mode) was greater than 0.4 mm in those with shoulder pain. It should be noted that, researchers mentioned the measurement error as a reason for this difference. O’sullivan et al. showed that the upper, middle and lower trapezius muscle thickness in the patients with shoulder pain was not different with healthy people. Obviously, one of the main reasons was the mild shoulder pain in the patients [35]. Another important issue is that the level of thickness change in people with chronic pain that is clinically important is not known yet [36]. However, the muscle thickness alterations need further research.
Koppenhaver et al. in another study to investigate the effects of DDN on the change in thickness of infraspinatus muscle showed that dry needling did not make a significant change in the muscle thickness of rest and contraction modes. In this study, similar to the present study, it was shown that the change in the function and thickness of the muscle is not associated with the improvement of the subject’s symptoms. One of the reasons mentioned for the lack of a significant change in the muscle thickness after dry needling is that electromyographic studies have shown that the time of muscle activity following the dry needling changes, but there is not any changes in muscle function.
Study Limitations
In the present study, due to the ethical considerations, there was no group without treatment. Therefore, the researchers did not know the natural course of recovery in these subjects. However, all people had chronic pain. Furthermore, therapeutic effects were followed up for 15 days after the last treatment. Longer term follow-up would have added weight to the study’s findings. Moreover, the findings of the present study can only be generalized to young participants with MPS. Finally, the present study is not a reflection of the actual clinical practice since additional interventions were not allowed that is usual in physical therapy.
Conclusion
SDN has the same therapeutic effects as DDN in the short term. To make long-term changes, the SDN method is not effective. Therefore, even if the treatment initially begins with SDN, it should be continued with DDN. The DDN method has better effects in the short and long terms than the SDN. However, this does not reduce the importance of the SDN applications.
Acknowledgements
The authors wish to acknowledge the Iran University of Medical Sciences for collaboration in the present study.
Conflict of Interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Registration number: IR.IUMS.REC.1395. 9413340001.
References
- Dommerholt J, Huijbregts P (2011) Myofascial trigger points: Pathophysiology and evidence-informed diagnosis and management. (1st edn) Jones and Bartlett, Toronto, pp: 3-86.
- Alvarez DJ, Rockwell PG (2002) Trigger points: Diagnosis and management. Am Fam Physician 65: 653-660.
- Dommerholt J, Fernandez-de-Las-Penas C, Chaitow L, Gerwin RD (2013) Trigger point dry needling: An evidenced and clinical-based approach. (1st edn) Edinburgh, pp: 35-40.
- Baldry PE (2005) Acupuncture, trigger points and musculoskeletal pain. (3rd edn) Elsevier Ltd, pp: 207-222.
- Behnam A, Mahyar S, Ezzati K, Rad SM (2014) The use of dry needling and myofascial meridians in a case of plantar fasciitis. J Chir Med 13: 43-48.
- Haker E, Lundeberg TH (1990) Acupuncture treatment in epicondyllagia: A comparative study of two acupuncture techniques. Clin J Pain 6: 221-226.
- Ceccherelli F, Rigoni MT, Gagliardi G, Ruzzante L (2002) Comparison of superficial and deep acupuncture in the treatment of lumbar myofascial pain: A double-blind randomized controlled study. Clin J Pain 18: 149-153.
- Itoh K, Katsumi Y, Kitakoji H (2004) Trigger point acupuncture treatment of chronic low back pain in elderly patients: A blinded RCT. Acupunct Med 22: 170-177.
- Baldry P (2002) Superficial versus deep dry needling. Acupunct Med 20: 78-81.
- Pavkovich R (2015) The use of dry needling for a subject with acute onset of neck pain: A case report. Int J Sports Phys Ther 10: 104-113.
- Pecos-Martin D, Aguilera FJ, Izquierdo TG, Urraca-Gesto A, Gomez-Conesa A, et al. (2015) Effectiveness of dry needling on the lower trapezius in patients with mechanical neck pain: A randomized controlled trial. Arch Phys Med Rehabil 96: 775-781.
- Edwards J, Knowles N (2003) Superficial dry needling and active stretching in the treatment of myofascial pain: A randomised controlled trial. Acupunct Med 21: 80-86.
- Rock JM, Rainey Ch (2014) Treatment of nonspecific thoracic spine pain with trigger point dry needling and intramuscular electrical stimulation: A case series. Int J Sports Phys Ther 9: 699-711.
- Koppenhaver SL, Walker MJ, Su J, McGowen JM, Umlauf L, et al. (2015) Changes in lumbar multifidus muscle function and nociceptive sensitivity in low back pain patient responders versus non-responders after dry needling treatment. Man Ther 20: 769-776.
- Salavati M, Akhbari B, Ebrahimi I, Ezzati K, Haghighatkhah H (2017) Reliability of the upper trapezius muscle and fascia thickness and strain ratio measurements by ultrasonography imaging and sonooelastography in subjects with myofascial pain syndrome. J Chir Med 16: 316-323.
- Koppenhaver S, Harris D, Harris A, O’Connor E, Dummar M, et al. (2015) The reliability of rehabilitation ultrasound imaging in the measurement of infraspinatus muscle function in the symptomatic and asymptomatic shoulders of patients with unilateral shoulder impingement syndrome. J Bodyw Mov Ther 10: 128-135.
- Simons DG, Travell JG, Simons LS (1999) Travell & Simons Myofascial Pain and Dysfunction: Upper Half of Body. Baltimore, MD: Lippincott Williams & Wilkins.
- Shin S, Yoon DM, Yoon KB (2011) Identification of the correct cervical level by palpation of spinous processes. Anesth Analg 112: 1232-1235.
- Daniels L, Worthingham C (2014) Muscle testing: Techniques of manual examination. (9th edn) Philadelphia: WB Saunders.
- Ong J, Claydon LS, Teach CT (2014) The effect of dry needling for myofascial trigger points in the neck and shoulders: A systematic review and meta-analysis. J Bodyw Mov Ther 18: 390-398.
- IIbuldu E, Cakmak A, Disci R, Aydin R (2004) Comparison of laser, dry needling, and placebo laser treatments in myofascial pain syndrome. Photomed Las Surg 22: 306-311.
- Kamanli A, Kaya A, Ardicoglu O, Ozgocmen S, Zengin FO, et al. (2005) Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol lnt 25: 604-611.
- Maher RM, Hayes DM, Shinohara M (2013) Quantification of dry needling and posture effects on myofascial trigger points using ultrasound shear-wave elastography. Arch Phys Med Rehabil 94: 2146-2150.
- Gerber LH, Shah J, Rosenberger W, Armstrong K, Turo D, et al. (2015) Dry needling alters trigger points in the upper trapezius muscle and reduces pain in subjects with chronic myofascial pain. PMR 7: 711-718.
- Tsai CT, Hsieh LF, Kuan TS, Kao MJ, Chou LW, et al. (2010) Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am J Phys Med Rehabil 89: 133-140.
- Rickards LD (2009) Therapeutic needling in osteopathic practice: An evidence-informed perspective. Int J Osteopath Med 12: 2-13.
- Koppenhaver S, Embry R, Ciccarello J, Waltrip J, Pike R, et al. (2016) Effects of dry needling to the symptomatic versus control shoulder in patients with unilateral subacromial pain syndrome. Man Ther 26: 62-69.
- Cagnie B, Barbe T, Ridder E, Van Oosterwijck J, Cools A, et al. (2012) The Influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. J Manipulative Physiol Ther 35: 685-691.
- Kamali Hakim I, Ebrahimi I, Sarrafzadeh J, Ezzati K (2017) What is the acute effect of dry needling on the active trigger points of upper trapezius muscle? The effect of eliciting local twitch response on clinical outcomes. PTJ 7: 49-57.
- Sterling M, Bill V, Souvlis T, Connelly L (2015) Dry-needling and exercise for chronic whiplash associated disorders (WAD): A randomised single blind placebo-controlled trial. Int Associat Stud Pain 23: 1-6.
- Cheng JW, Tsai WC, Yu TY, Huang KY (2012) Reproducibility of sonographic measurement of thickness and echogenicity of the plantar fascia. J Clin Ultrasound 40: 14-19.
- Kuniyasu K (2014) Changes in neck muscle thickness due to differences in intermittent cervical traction force measured by ultrasonography. J Phys Ther Sci 26: 785-787.
- Akhbari B, Salavati M, Ebrahimi E, Ezzati K, Haghighatkhah H (2015) Association of ultrasonography findings with pain, range of motion, disability, and pressure pain threshold in subjects with upper trapezius myofascial pain syndrome. PTJ 4: 221-227.
- Critchley DJ, Coutts FJ (2002) Abdominal muscle function in chronic low back pain patients: Measurement with real-time ultrasound scanning. Physiotherapy 88: 322-331.
- O’Sullivan C, Meaney J, Boyle G, Gormley J, Stokes M (2009) The validity of rehabilitative ultrasound imaging for measurement of trapezius muscle thickness. Man Ther 14: 572-578.
- Ota M, Kaneoka K (2011) Differences in abdominal muscle thicknesses between chronic low back pain patients and healthy subjects. J Phys Ther Sci 23: 855-858.
Citation: Sarrafzadeh J, Khani S, Ezzati K, Takamjani IE (2018) Effects of Superficial and Deep Dry Needling on Pain and Muscle Thickness in Subject with Upper Trapezius Muscle Myofascial Pain Syndrome . J Pain Relief 7: 322. DOI: 10.4172/2167-0846.1000322
Copyright: © 2018 Sarrafzadeh J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 10016
- [From(publication date): 0-2018 - Dec 10, 2025]
- Breakdown by view type
- HTML page views: 8925
- PDF downloads: 1091