End of Life and Palliative Care
Received: 24-Mar-2024 / Manuscript No. jpcm-24-130574 / Editor assigned: 26-Mar-2024 / PreQC No. jpcm-24-130574 / Reviewed: 08-Apr-2024 / QC No. jpcm-24-130574 / Revised: 13-Apr-2024 / Manuscript No. jpcm-24-130574 / Published Date: 19-Apr-2024
Abstract
Introduction: Death is inevitable; death is bound to happen be it through illness or any other mode. As a consequence, many people die in hospitals, alone and in pain. Helping patients and their families understand the nature of illness and prognosis is a crucial aspect of palliative care near the end of life. Additionally, palliative care specialists help patients and their families to determine appropriate medical care and to align the patient’s care goals with those of the healthcare team. Finally, establishing the need for a medical proxy, advance directives, and resuscitation status is an integral part of palliative care at the end of life.
Aims and Objectives: The study aims to determine the effect of palliative care at end-of-life Stage.
Methods: It was Prospective observational hospital-based study conducted in the Palliative Department of Mahatma Gandhi Medical College and Hospital, Jaipur, (Rajasthan) for a period of 01 year in all the patients in the end of Life who gave their consent. We assessed the 04 components of Total pain, Psycho, Social and Spiritual assessment of patients with life threatening illness. Questions in 02 sections were asked that could help the Clinicians to Plan the care.
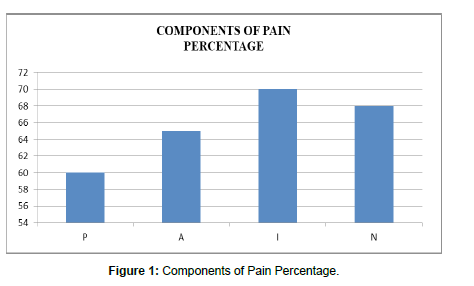
Results: Total Number of 70 Patients was studied of which 05 died during the period of study. The age group of the study was between 45-70 years of which 38 were Males and 27 were Females. Maximum Patients were of Cancer. It was observed that interpersonal problems as loneliness, financial stress and family tensions constituted 70% of 04 constituents of Pain. Among the Psychosocial assessment, Family stress was 75% whereas Psychiatric Vulnerability and Patient Physicians relationship constituted 70%. Most of the patients approximately 76.9% wanted to be remembered by their loved ones some or the other way.
Conclusion: The role of palliative care at the end of life is to relieve the suffering of patients and their families by the comprehensive assessment and treatment of physical, psychosocial, and spiritual symptoms patients experience.
Keywords
End of Life, Palliative Care, Total Pain, Psychosocial and Spiritual Assessment
Introduction
In the final stages of a terminal illness, it can become evident that in spite of the best care, attention, and treatment, your loved one is approaching the end of their life. At this point, the focus usually changes to making them as comfortable as possible in order to make the most of the time they have left. Depending on the nature of the illness and your loved one’s circumstances, this final stage period may last from a matter of weeks or months to several years. During this time, palliative care measures can help to control pain and other symptoms, such as constipation, nausea, or shortness of breath. Hospice care can also offer emotional and spiritual support to both the patient and their family. Even with years of experience, caregivers often find this final stage of the care giving journey uniquely challenging. Simple acts of daily care are often combined with complex end-of-life decisions and painful feelings of grief and loss. You may experience a range of distressing and conflicting emotions, such as sorrow and anxiety, anger and denial, or even relief that your loved one’s struggle is at an end, or guilt that you’ve somehow failed as their caregiver. Whatever you’re experiencing, it’s important to recognize that late-stage care giving requires plenty of support. That can range from practical support for end-of-life care and financial and legal arrangements, to emotional support to help you come to terms with all the difficult feelings you’re experiencing as you face up to the loss of your loved one. Late-stage care is also a time for saying goodbye to your loved one, to resolve any differences, forgive any grudges, and to express your love. While late-stage cares giving can be an extremely painful time, having this opportunity to say goodbye can also be a gift to help you come to terms with your loss and make the transition from nursing and grief towards acceptance and healing.
While dying is inevitable, death is bound to happen be it through illness or any other mode. As a consequence, many people die in hospitals, alone and in pain [1]. Palliative care focuses primarily on anticipating, preventing, diagnosing, and treating symptoms experienced by patients with a serious or life-threatening illness and helping patients and their families make medically important decisions. The ultimate goal of palliative care is to improve quality of life for both the patient and the family, regardless of diagnosis. Although palliative care, unlike hospice care, does not depend on prognosis, as the endof- life approaches, the role of palliative care intensifies and focuses on aggressive symptom management and psychosocial support. Helping patients and their families understand the nature of illness and prognosis is a crucial aspect of palliative care near the end of life. Additionally, palliative care specialists help patients and their families to determine appropriate medical care and to align the patient's care goals with those of the healthcare team. Finally, establishing the need for a medical proxy, advance directives, and resuscitation status is an integral part of palliative care at the end of life.
Palliative medicine establishes goals to relieve suffering in all stages of disease and is not limited to comfort care or end-of-life care [2]. The alleviation of suffering is an essential goal of medical care. To treat it, however, providers must first recognize pain and suffering [3]. Saunders first described the concept of total pain [4] and interaction among the various sources of pain and suffering. [5] Total pains is the sum of the patient's physical, psychological, social, and spiritual pain. This concept is central to the assessment and diagnosis of pain and suffering. Because psychological distress, lack of social support, and physical pain are associated [6]. Treating a patient's total pain is imperative, especially at the end of life. Optimal pain relief will not be possible unless all the elements of total pain are addressed.
Aims and Objectives
Patients near the end of life may experience extreme symptoms that include physical, spiritual, and psychosocial suffering. Preventing and managing these symptoms while optimizing the quality of life throughout the dying process is the goal of palliative medicine [7].
Method
It was Prospective observational hospital-based study conducted in the Palliative Department of Mahatma Gandhi Medical College and Hospital, Jaipur, (Rajasthan) for a period of 01 year in all the patients in the end of Life who gave their consent. We assessed the four components of Total pain, Psychosocial and Spiritual assessment of patients with life threatening illness. Questions in 02 sections were asked that could help the Clinicians to Plan the care. Four Components of Pain were assessed (Table 1). A survey into Eight Components of Psychosocial Assessment was done (Table 2). Patients Coping Strengths and inner resources were analysed and his goals of healing and strengthening relationship were elicited (Table 3).
Statistical analysis
| Four Components of Pain | ||
|---|---|---|
| P | Physical Problems | Often Multiple, must be diagnosed specifically and treated |
| A | Anxiety | Anger and Depression. These are critical components of Pain and must be addressed by Physician in Cooperation with other healthcare Professionals |
| I | Interpersonal Problems | Like Loneliness, financial Stress and Family Tensions |
| N | Not Accepting | Approaching Death, A sense of Hopelessness and Desperate search for meaning of Suffering. These sufferings have to be taken care of because mostly are not relived by Medicines. |
Table 1a: Four Components of Pain were assessed.
| Percentage | ||
|---|---|---|
| P | Physical Problems | 60% |
| A | Anxiety | 65% |
| I | Interpersonal Problems | 70% |
| N | Not Accepting | 68% |
Table 1b: Percentage of each Component of Pain.
| Psychosocial & Spiritual Assessment of Patients with Life Threatening Illness | |||||||
|---|---|---|---|---|---|---|---|
| Yes | Uncertain | No | |||||
| S.No | Domains | N | % | N | % | N | % |
| 1) | Meaning of Illness | 42 | 65% | 7 | 10% | 16 | 25% |
| 2) | Coping with illness | 39 | 60% | 7 | 10% | 19 | 30% |
| 3) | Social Support Network | 26 | 40% | 13 | 20% | 26 | 40% |
| 4) a | Stressors related to patient | 40 | 62% | - | - | 25 | 38% |
| 4) b | Stressors related to Family | 49 | 75% | - | - | 16 | 25% |
| 5) | Spiritual Resources and Faith | 40 | 62% | 9 | 13% | 16 | 25% |
| 6) | Psychiatric Vulnerability | 45 | 70% | 7 | 10% | 13 | 20% |
| 7) | Economic or Financial Issues | 42 | 65% | 10 | 15% | 13 | 20% |
| 8) | Patient – Physicians Relationship. | 45 | 70% | - | - | 20 | 30% |
| NOTE: - N= Number of Patients. | |||||||
Table 2: A survey into Eight Components of Psychosocial Assessment was done.
| Useful Questions for Clinicians to understand Patients Value/Strength/Goals | |||||
|---|---|---|---|---|---|
| S.no | Questions | Yes | No | ||
| N | % | N | % | ||
| A | Mobilising a Patient’s Coping Strength and Inner Resources | ||||
| 1 | Have you lived up to your own ideals in the way you have dealt with your illness? | 40 | 61% | 25 | 38% |
| 2 | Do you feel that this has been a meaningful time for you and the people you care about? | 42 | 64% | 23 | 35.30% |
| 3 | Do you want to be remembered by the people you care about? | 50 | 76.90% | 15 | 23% |
| 4 | Have you found yourself growing or changing or hoped that you could grow or change in this last phase of your life? | 20 | 30.70% | 45 | 69.20% |
| 5 | Are there some of the moments when you have felt most discouraged and downhearted as you have faced your illness? | 41 | 63% | 24 | 36.90% |
| 6 | Are there barriers to feel secure and in reasonable control as you go through this experience with your illness? | 39 | 60% | 26 | 40% |
| 7 | Are there resources and strengths within you that can help you cope? | 41 | 63% | 24 | 36.90% |
| B | Eliciting Patient’s Goals for Healng and Strengthening Relationship | ||||
| 1 | Are there Important relationships in your life including relationship from past, that needs healing or strengthening? | 23 | 35.30% | 42 | 64% |
| 2 | Are there relationships in which you feel something important has been left unsaid? | 25 | 38% | 40 | 61% |
| 3 | Do important people in your life know what they mean to you? | 39 | 60% | 26 | 40% |
| 4 | Are there stories, values or ideas that you want to transmit to people as part of your legacy? | 50 | 76.90% | 15 | 23% |
| 5 | Are there ways that you can help your family now to prepare or deal with your death? | 41 | 63% | 24 | 36.90% |
| 6 | Would you be able to continue to be present in the lives of people you love after you are gone? | 50 | 76.90% | 15 | 23% |
| 7 | Would you like to say good bye to people who have been important to you? | 60 | 92.30% | 5 | 7.60% |
| Note - N= Number of Patients | |||||
Table 3: Patients Coping Strengths and inner resources were analysed and his goals of healing and strengthening relationship were elicited.
Results were expressed in percentage and comparison done.
Result
Total Number of 70 Patients was studied of which 05 died during the period of study. The age group of the study was between 45-70 years of which 38 were Males and 27 were Females. Out Of the 65 remaining Patients, 42 had Cancer, 06 had AIDS and 12 Patients were with COPD and Pleural Effusion and 5 Patients with Cardiac Problems. Four Components of the pain were assessed of which the third Component interpersonal Problems contributed to 70% revealing Loneliness, Financial Stress and Family Tensions which were deeply interwoven into the fabric of Patients Symptoms. Fourth Component contributed about 68% which was in the form of Sense of hopelessness and desperate search for meaning of Suffering. Second Component i;e Anxiety , anger and depression contributed 65% whereas The First Component the Physical Pain contributed to 60% of the results (Figure 1).
Psychosocial and Spiritual assessment of the Patients were done based on eight questions that were
1) Meaning of Illness
2) Coping with illness
3) Social Support Network
4) Stressors related to Patient and Family
5) Spiritual Resources and Faith
6) Psychiatric Vulnerability
7) Economic or Financial Issues
8) Patient/Physician Relationship.
Among the Psychosocial assessment, Family stress was 75% whereas Psychiatric Vulnerability and Patient Physicians relationship constituted 70%. Questions related to Mobilizing Patients Coping Strength and inner resources showed that 76.9% wanted to be remembered by the people they care about some or the other way. 64% of patients felt that there has been a meaningful time with the people they spent time with. 63% agreed with the having enough resources and strength within themselves that can help them cope the disease. At the same time, they also felt discouraged and downhearted while facing the illness. From the question that elicited Patients goals for healing and strengthening relationship showed that 76.9% wanted to continue with their Values and Ideas and pass on to their loved ones as part of their legacy.
Discussion
Factors important to seriously ill patients include adequately controlling pain and other symptoms, avoiding prolongation of the dying process, achieving a sense of self-control, finding meaning in life, and relieving the care burdens of family and loved ones while strengthening and completing those same relationships [8]. This has been proved in our study that patients were more bothered about Financial Stress and family tensions which constituted 70% of the burden also they were not ready to accept the approaching death and had a feeling of hopelessness which constituted about 68% of the total pain. Thus, it is important to consider these factors equally as the clinicians managing Physical pain by Pharmacotherapy. As death becomes nearer, the symptom burden increases while the patient and family tolerance of physical and emotional stress decreases. At this time, primary palliative care interventions should take precedence, and the focus on restorative care should decrease. Pain is one of the most prevalent symptoms near the end of life. Unrelieved pain can be a source of great distress for patients and families and exacerbate other symptoms. Therefore, the adequate management of pain at the end of life is imperative. Although opioid analgesics are the standard of care for treating moderate to severe pain in patients with advanced illness, the false fear that opioids induce respiratory depression and hasten death is a major barrier to their use at the end of life. However, both effects are uncommon when opioids are given at appropriate doses [9]. As death approaches, a clinician may use continuous infusions to manage symptoms and relieve suffering if scheduled or as-needed doses are not adequate. The clinician should continually assess the patient and make adjustments that will control symptoms [10].
Once the physical adverse symptoms and distress have been successfully addressed, it is important to broaden the integrated response of the interdisciplinary treatment team to address the psychosocial and spiritual issues that are an inherent part of the dying process. A comprehensive psychosocial and spiritual assessment allows the team to lay a foundation for healthy patient and family adjustment, coping, and support. Skilled expert therapeutic communication through facilitated discussions is beneficial to maintaining and enhancing relationships, finding meaning in the dying process, and achieving a sense of control while confronting and preparing for death [11]. Compassionate palliative care requires a professional readiness of those specialized in this field to explore the integrity-preserving issues that will foster growth in dignity and transcendence. Reflective open-ended questions are key in optimizing this communication and assessing the willingness of the patient and caregivers to engage. Physicians, psychologists, nurses, social workers, and chaplains can assimilate and negotiate the interpersonal relationship skills and intimacy required to enhance the patient's peace and psychosocial spiritual comfort [11]. Our Study revealed that psychosocial stress particularly related to Family and the loved ones was bothering the patient most which in our study constituted 75%. The Psychiatric Vulnerability in the form of depression, anxiety, difficulty in coping was about 70%. Same way Patient Physician Relationship that is how a physician can help a patient in different situations constituted 70%. Concern about Financial issues was 65% and understanding the meaning of illness was also 65%.
Many patients imagine that death comes suddenly, but for many, the knowledge that one's death is imminent comes first. Those with this awareness often must complete certain tasks to allow a peaceful death such as offering forgiveness, being forgiven, acknowledging regrets, finding closure in professional and community relationships, and saying goodbye to family and friends. Various questions that were asked about mobilizing Patients Strengths and inner resources revealed that 76.9% patients want to be remembered by their loved ones and 64% patients were satisfied with the time spent with their near and dear ones. 63% showed Strengths and resources within to cope with the situations. Questions eliciting Patients goals for healing and strengthening relationship showed that 76.9% want their values and ideas to be transmitted to people as part of their legacy so that they can continue to be present in the lives of people they love after they leave. Most of the patients in our study about 92.3% wanted to say good bye to people who were close to them before leaving this world.
Conclusion
The role of palliative care at the end of life is to relieve the suffering of patients and their families by the comprehensive assessment and treatment of physical, psychosocial, and spiritual symptoms patients’ experience. As your loved one enters late-stage / end-of-life care, their needs can change, impacting the demands one shall face as their caregiver. This can include the following areas as Practical Care and assistance, Comfort and dignity, Respite care, grief support. End of life planning consisting of early preparation, financial and legal advices as living will, Power of Attorney or Advance directives, focus on values, address family Conflicts, communicate with family members and if children are involved make effort to include them. As death approaches, the symptom burden of a patient may worsen and require more aggressive palliation. As comfort measures intensify, so does the support provide to a dying patient's family. Once death has occurred, the role of palliative care focuses primarily on the support of the patient's family and bereavement.
Ethical Consideration
The study was reviewed by the ethical Committee of Mahatma Gandhi Medical College and Hospital Jaipur (Rajasthan) and approved the study vide letter Number – No/MGMC&H/IEC/JPR 2023/1844.
Funding
Nil
Consent
Valid Informed Consent was taken from all the participants.
Acknowledgement
We would like to thank all the participants for their valuable contribution to this study.
References
- Connors AF,Dawson NV,Desbiens NA (1995) A Controlled Trial to Improve Care for Seriously III Hospitalized Patients:The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT).JAMA 274:1591-1598.
- Meier DE, Bishop TF (2011) Palliative care; benefits, services, and models of care. Waltham MA: Up-to-date.
- Cassell EJ (1999) Diagnosing suffering: a perspective.Ann Intern Med 131: 531-534.
- Bial A, Levine S (2007) the assessment and treatment of physical pain associated with life-limiting illness. Hospice/Palliative Care Training for Physicians: UNIPAC 3.
- Saunders C (1996) Apersonal therapeutic journey. BMJ 313: 1599-1601.
- Zaza C, Baine N (2002) Cancer pain and psychosocial factors: a critical review of the literature.J Pain Symptom Manage 24: 526-542.
- Kuebler KK, Heidrich DE, Esper P (2006) Palliative and end-of-life care: Clinical practice guidelines. Elsevier Health Sciences.
- Singer PA, Martin DK, Kelner M (1999) Quality end-of-life care: patients' perspectives.JAMA 281: 163-168
- Von Gunten CF (2005) Interventions to manage symptoms at the end of life. Journal of Palliative Medicine. 8(supplement 1): s-88.
- Qaseem A, Snow V, Shekelle P (2008) Clinical Efficacy Assessment Subcommittee of the American College of Physicians. Evidence-based interventions to improve the palliative care of pain, dyspnea, and depression at the end of life: a clinical practice guideline from the American College of Physicians.Ann Intern Med 148: 141-14
- Block SD (2001) Perspectives on care at the close of life. Psychological considerations, growth, and transcendence at the end of life: the art of the possible.JAMA285: 2898-2905.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Richa R, NipunL, Sudha S, Seema K (2024) End of Life and PalliativeCare. J Palliat Care Med 14: 623.
Copyright: © 2024 Richa R, et al. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1186
- [From(publication date): 0-2024 - Nov 16, 2025]
- Breakdown by view type
- HTML page views: 893
- PDF downloads: 293