Endoscopic Liberation of the Tibial Nerve and FHL Tendon after Posteromedial Fracture of the Talus
DOI: 10.4172/2329-910X.1000323
Abstract
Fractures of the medial tubercle of the posterior process of the Talus is a rare injury that is often misdiagnosed and mistreated. The location of the medial tubercle next to the posteromedial ankle makes the anatomical structures of this region susceptible to injury if the fracture does not heal properly. In cases that a chronic pain is caused by nonunion or malunion of a small fragment, surgical excision may give definitive solution. We describe here endoscopic excision of nonunion posteromedial fracture that irritated the Tibial nerve and FHL tendon.
Keywords: Cedell’s fracture; Posteromedial talus fractures; Endoscopy; Tibial nerve neurolysis
Introduction
Fracture of the medial tubercle of the posterior process of the talus is a rare injury, described by Cedell and named after him as Cedell’s fracture [1].
The posterior process of the Talus is a bony projection that helps to maintain the relationship between the anatomical structures and as an attachment point for ligaments. It is composed of two tubercules, medial and lateral, with a groove between them that allows the passage of Flexor Hallucis Longus (FHL) tendon. The next anatomical structures to the medial side are the neurovascular bundle, Extensor Digitorum longus and Tibialis anterior tendons in this order. This fracture can present only as a local posteromedial ankle pain, but it can also block or irritate the adjacent structures, especially the FHL and neurovascular bundle and by this cause irradiating pain.
Combination of difficulty to observe this fracture on plain x rays due to its anatomical location, and low index of suspicion due to its rare incidence, explains why this injury is often misdiagnosed as ankle sprain and treated accordingly [2]. This may lead to unsatisfactory results with persistent chronic pain and difficulty to return to sport [3].
The treatment of such injury depends on the size of the fragment, the amount of translation, and the time passed since the injury [4]. Usually for acute nondisplaced fractures, conservative treatment with cast immobilization is indicated [5]. For displaced or nonunion cases, a surgical treatment is advised that can be either ORIF for large fragments or excision for small fragments. For ORIF, the open posteromedial approach is usually used while excision can be done in open surgery or in an endoscopic fashion [6,7]. Endoscopic excision for this fracture was previously described and recently a series of 9 Cedell’s fractures that went through endoscopic excision was published with good results [7,8]. We report here an endoscopic treatment of Cedell’s fracture nonunion, the uniqueness of the case described here is that the fragment is in contact with the Tibial nerve as well as the FHL tendon. The patient gave informed consent to publish this case.
Case Report
A 24 year old male was presented in our clinic with complaints of persistent left posteromedial ankle and plantar forefoot pain in the last two years. He said to suffer from repeated ankle sprains, the last and most serious one was two years ago initiating this pain. Before referring to us he was previously treated with intensive physiotherapy and steroids injection with partial alleviation of the pain.
Now he suffers from pain, especially during sport activity when changing gait direction.
In his physical examination he has mild planovalgus foot, pain and fullness when palpating the medial retro malleolar area. No ankle laxity is found. Tinel on the medial retro malleolar region produces pain in the plantar foot at the territory of the tibial nerve. During this 2 years period before referring to us he completed the following imageries:
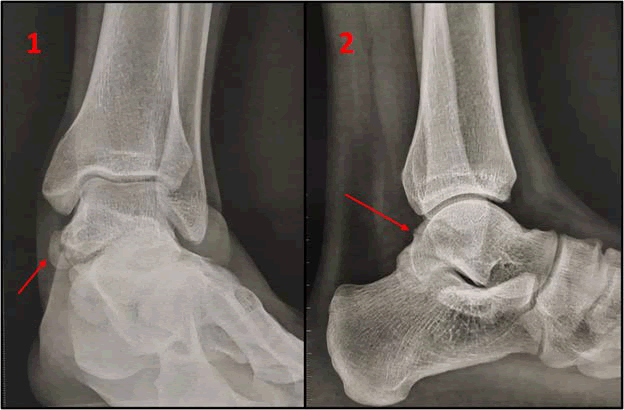
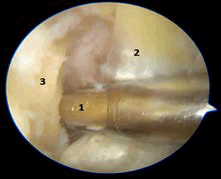
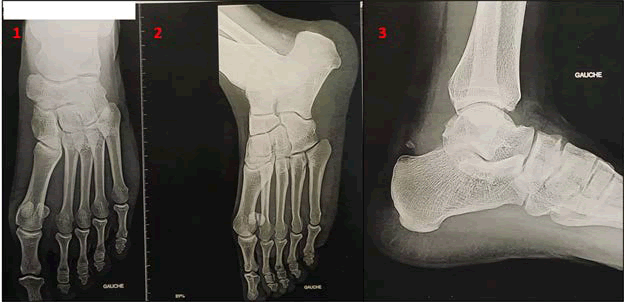
Plain x rays (taken 1.5 years after the injury) In the AP view a nonunion fragment is seen in the medial side above the subtalar joint. In the lateral view subtle radiolucent line that represents the fracture is seen (Figure 1).
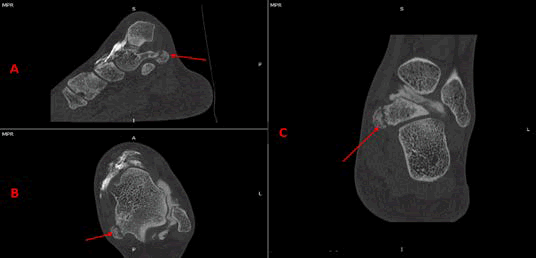
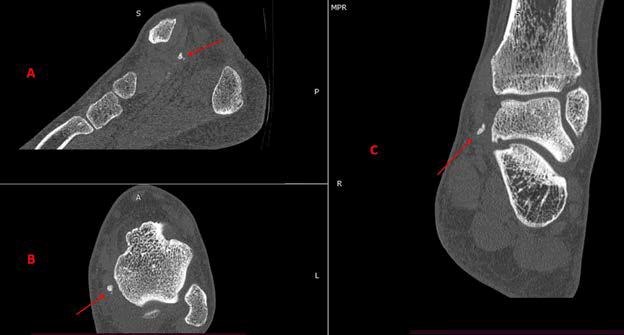
Arthro CT – Fracture of the medial part of the posterior process of the Talus with nonunion in all 3 axes. Note that the subtalar joint is not involved (Figure 2).
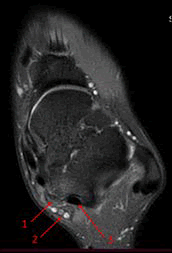
MRI axial view, Fragment that impinges the posterior neurovascular bundle and irritates the FHL tendon (Figure 3), no abnormalities were found in the medial or lateral ligaments of the ankle (not shown).
Due to the time passed since the injury, the persistent symptoms, and the failure of the conservative treatment, we proposed a surgical treatment endoscopic excision of the fragment and liberation of the Tibial nerve.
Surgical technique
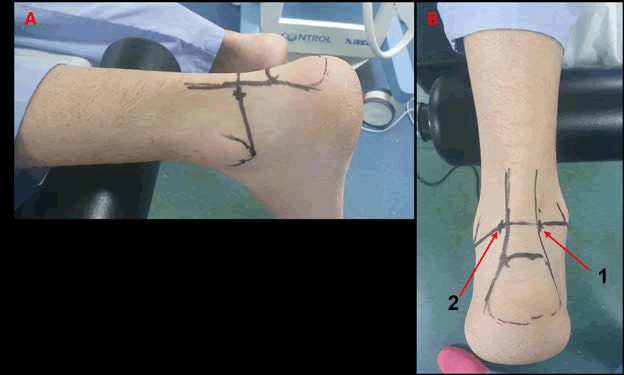
We used the posterior approach as described by Van Dijk [9]. Under spinal anesthesia the patient was placed in a prone position, the legs were left beyond the edge of the table on a padded bar to allow free movement of the ankle (Figure 4A). A tourniquet was placed on the tight and standard sterilization and sterile cover were set in place. Medial and lateral malleolus, Achilles tendon and calcaneus were outlined and a line connecting the tip of the medial and lateral malleolus is drawn. The two portals are on this line, just medial and lateral to the Achilles tendon (Figure 4B). First, the lateral portal is created with only skin incision followed by blunt deep dissection with mosquito forceps to avoid damage to the Sural nerve. With a mosquito clamp we pass just under the Achilles tendon directing to its medial side pressing the skin from the inside as a marker to create the medial portal.
Figure 4: Patient and portals setting: (A) First we outline of the medial and lateral malleolus, Achilles tendon and calcaneus, then a line connecting the tip of the medial and lateral malleolus is drawn. The two portals are on this line, just medial and lateral to the Achilles tendon (A+B). (B) The patient is in a prone position, the legs are beyond the edge of the table on a padded bar.
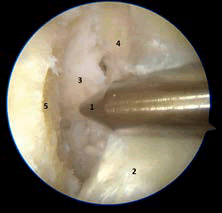
An optic cannula with a trocar is introduced through the lateral portal pointing to the 2nd ray until a bony groove is felt (the subtalar joint) and the trocar is replaced with a camera (30° 4.5 mm). A 3.5 mm straight shaver blade (Dyonics Smith and Nephew) introduced through the medial portal pointing to the lateral side. First, we found a big amount of synovitis and under vision we carefully cleaned it and looked for the subtalar joint. When we see the joint line, the priority is to identify the FHL tendon that serves as a landmark. To do so we carefully glide medially along the subtalar joint with shaver back (safe) side facing medially and the cutter facing laterally, cleaning the surrounding tissue until the FHL tendon is found. We verify that what we see is really the FHL by passively moving the Hallux while simultaneously record the tendon moving.
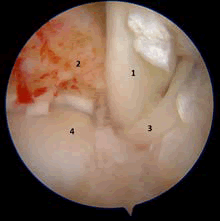
Unlike usual posterior ankle endoscopy, the FHL tendon was found in a much anterior position compared to its normal location and a big amount of fibrosis was found around it that significantly reduced the tendon mobility. Due to the FHL anterior position and to facilitate the access, we excise the lateral tubercle of the posterior process with a curved osteotome. With the shaver back facing medial (leaning against the FHL tendon and pushing it medially) and cutting part facing lateral (leaning on the medial wall of the Talus) (Figure 5) we detached the FHL sheath until we reached a bony prominence that was sticked to the Tibial nerve. With blunt dissection we carefully detached the fragment from the Tibial nerve (Figure 6) and then complete the excision of the bony fragment with shaver and forceps. At the end of the procedure the tibial nerve was free and the FHL tendon could move freely within its tunnel (Figure 7). The portals were sutured with vicryl rapide 3.0 and sterile bandage was used without any cast or immobilizing device.
Postoperative care
The patient was discharged on the same day, he was allowed immediate full weight bearing. For the first week he was asked to keep his leg up while resting and using cold compression a couple of times per day to reduce swelling of the ankle. No special physiotherapy was prescribed. The patient returned to work the day after surgery (Taxi driver).
At 3 weeks post-operative the patient came for his first check-up. At this point he reported improvement of the familiar pain but mild pain when extending the Hallux, he could walk without limitation. No neurological deficit was found. The medial retro malleolar fullness was no longer palpable. In a post op x-ray no abnormalities are noted (Figure 8). The patient was instructed to return to normal activity without limitation.
At 4 months the patient returned for a second checkup, he reported complete disappearance of the medial pain and no irradiating pain. He could return to sport with much improvement compared to his preoperative limitation. He specifies that he does suffer from mild lateral pain only during sportive activity. In his physical examination we find a mild sensitivity over the fibularis tendons and mild snaping of the fibularis. He is instructed to keep his activity without restriction, and to complete dynamic Echo for the fibularis tendons and CT scan.
At 6 months post op checkup he remains pain free in the medial side, he reports improvement in the lateral side pain. The echo test demonstrates switching of the fibularis tendons next to the inferior retinaculum. The CT scan shows disappearance of the fragment beside a small remnant of bone (Figure 9).
Result and Discussion
Fracture of the medial tubercle of the posterior process of the Talus is a rare injury that is often missed in the acute setting. Malunion or nonunion of the fragment may irritate the adjacent anatomical structures and cause chronic pain. If the fragment is small excision is the treatment of choice for pain alleviation with good functional results [8]. Due to the deep location of the posterior process an open approach requires a large incision and careful dissection, for this reason endoscopic approach is preferable. The posterior endoscopic approach is a well-established tool that allows particularly good visualization of the posterior process of the Talus, is relatively safe and prevents the use of large scars and their complications. The use of endoscopic approach for fragment excision was already described [7,8], but here we report a unique situation where the fragment irritates the Tibial nerve. We show that by using careful blunt dissection we can detach the fragment and treat those injuries with good results.
Conclusion
The advantage of performing this endoscopically is the good visualization, the ability to carefully clean the synovitis and the use of small portals that reduces the risk for infection and wound complication and a very quick return to normal activities. On the other hand, working in such vicinity to the neurovascular structures requires extreme caution and accuracy that is usually achieved after long training and is better done after accumulating experience with “standard” cases.
Conflict of Interest
We have no conflict of interests to disclose and the manuscript has been read and approved by all named authors.
Acknowledgement
The Authors are very thankful and honored to publish this article in the respective Journal and are also very great full to the reviewers for their positive response to this article publication.
References
- Cedell CA (1974) Rupture of the posterior talotibial ligament with the avulsion of a bone fragment from the talus. Acta Orthop Scand. 45(3): 454-61.
- Ebraheim NA, Patil V, Frisch NC, Liu X (2007) Diagnosis of medial tubercle fractures of the talar posterior process using oblique views. Injury. 38(11): 1313-7.
- Kim DH, Berkowitz MJ, Pressman DN (2003) Avulsion fractures of the medial tubercle of the posterior process of the talus. Foot Ankle Int. 24(2): 172-5.
- Watanabe H, Majima T, Takahashi K, Kawaji H (2017) Split fracture of the posteromedial tubercle of the talus: Case report and proposed classification system. J Foot Ankle Surg. 56(1): 187-190.
- O'Loughlin P, Sofka CM, Kennedy JG (2009) Fracture of the medial tubercle of the posterior process of the talus: Magnetic resonance imaging appearance with clinical follow-up. HSS J. 5(2): 161-4.
- Shi Z, Zou J, Yi X (2013) Posteromedial approach in treatment of talar posterior process fractures. J Invest Surg. 26(4): 204-9.
- Martinez MJ, Román CV, Giménez EM, Sanz-Reig J (2017) Arthroscopic treatment of a malunion of a posteromedial tubercle fracture of the talus. Arthrosc Tech. 6(6): e2107-e2110.
- Zwiers R, Leeuw PAJD, Wiegerinck EMA, Dijk CNV (2020) Surgical treatment for posteromedial talar process fractures. Foot Ankle Surg. 26(8): 911-917.
- Dijk CNV, Scholten PE, Krips R (2000) A 2 portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 16(8): 871-6.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2303
- [From(publication date): 0-2021 - Dec 22, 2025]
- Breakdown by view type
- HTML page views: 1630
- PDF downloads: 673