Review Article Open Access
Endoscopic Therapy for Early Esophageal Neoplasia
Hendrik Manner*Department of Internal Medicine II, HSK Wiesbaden, Germany
- *Corresponding Author:
- Hendrik Manner
Head of Endoscopy
Department of Internal Medicine II
HSK Wiesbaden, Germany
Tel: +49611432420
Fax: +49611432418
E-mail: HSManner@gmx.de
Received date: July 18, 2014; Accepted date: September 12, 2014; Published date: September 19, 2014
Citation: Manner H (2014) Endoscopic Therapy for Early Esophageal Neoplasia. J Gastroint Dig Syst 4:218. doi:10.4172/2161-069X.1000218
Copyright: © Manner H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Endoscopic treatment of early esophageal neoplasia has widely been established in gastroenterology. It has been shown to be effective and safe also in the long-term follow-up, and it is – in contrast to the previous goldstandard, which is esophageal resection – organ preserving. There is no treatment-related mortality and a very low morbidity. In early Barrett’s neoplasia, the two-step concept of endoscopic resection (ER) of all neoplasia and thermal ablation of the non-neoplastic remainder of the Barrett’s segment is the treatment of choice, combining a high rate of curation with a low risk of treatment-related stricture formation. There are two ER techniques for early esophageal neoplasia: The suck-and-cut technique and endoscopic submucosal dissection, the latter one mainly used for squamous cell cancer. For thermal ablation, radiofrequency ablation (RFA) and argon-plasma coagulation (APC) are mainly used.
Abstract
Endoscopic treatment of early esophageal neoplasia has widely been established in gastroenterology. It has been shown to be effective and safe also in the long-term follow-up, and it is – in contrast to the previous gold-standard, which is esophageal resection – organ preserving. There is no treatment-related mortality and a very low morbidity.
In early Barrett’s neoplasia, the two-step concept of endoscopic resection (ER) of all neoplasia and thermal ablation of the non-neoplastic remainder of the Barrett’s segment is the treatment of choice, combining a high rate of curation with a low risk of treatment-related stricture formation.
There are two ER techniques for early esophageal neoplasia: The suck-and-cut technique and endoscopic submucosal dissection, the latter one mainly used for squamous cell cancer. For thermal ablation, radiofrequency ablation (RFA) and argon-plasma coagulation (APC) are mainly used.
Keywords
Endoscopic therapy; Radiofrequency ablation; Argon-plasma coagulation; Esophageal
Principles of Endoscopic Therapy
In early Barrett’s neoplasia, the so-called two-step concept of endoscopic resection (ER) using the suck-and-cut-technique of all neoplastic areas and thermal ablation of the non-neoplastic remainder of the Barrett’s remainder is the treatment of choice at present [1-3]. This treatment approach combines a high rate of curation with a favourably low risk of side effects (stricture formation, perforation, bleeding). For thermal ablation, radiofrequency ablation (RFA) and argon-plasma-coagulation (APC) are mainly used [1,4]. Another possible treatment approach that is mainly used in the U.S. is cryotherapy [5]. In early squamous cell cancer, only resection of the primary neoplasia has to be carried out.
Endoscopic Resection (ER)
ER is not only a therapeutic approach, but it is primarily diagnostic. In comparison with biopsy alone, a true tissue diagnosis can be made. It can be clarified by means of histopathological evaluation which kind of lesion exists (low-grade intraepithelial neoplasia, high-grade intraepithelial neoplasia, or early cancer), and the true invasion depth of the early neoplasia can be evaluated. If a lesion is diagnosed that shows a very low-risk of lymph-node metastasis, ER can be carried out with a curative intent.
A very low risk of lymph-node (LN) metastasis can be expected in early Barrett’s cancer that is limited to the mucosa (in experienced hands also with incipient submucosal invasion, sm1, together with a complete histopathological low-risk pattern G1-2, L0, V0) [6]. In early squamous cell cancer, the risk of LN metastasis starts to be relevant if the tumor invades the muscularis mucosae (m3 lesions). The latter lesions should only be treated endoscopically if the other histological patterns are classified as “low risk” (G1-2, L0, V0), or if the patient has a relevant comorbidity or is unwilling to undergo surgery or radiochemotherapy.
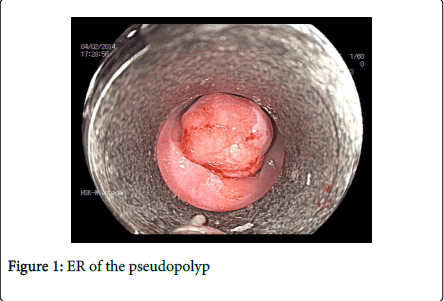
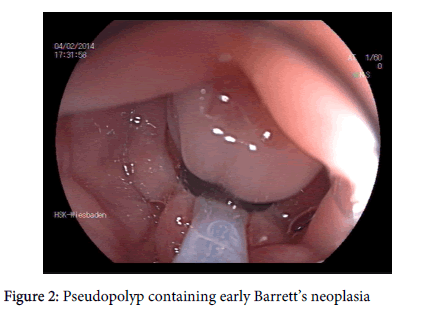
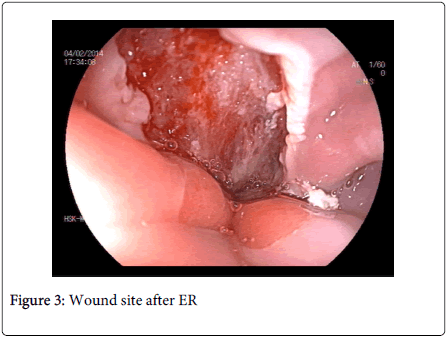
ER using the suck-and-cut technique: This technique has been introduced to endoscopy many years ago, and it has been shown to be effective and safe also in the long-term. Using suck-and-cut ER, the target lesion is sucked into a cylinder (ligation system (Figure 1) or transparent cap), and this newly formed pseudopolyp is then resected using a snare (Figures 2 and 3). Using a ligation device, a rubber-band is released over the pseudopolyp prior to resection. Lesions up to 20 mm in diameter can be resected in one piece (en bloc), and lesions beyond 20 mm can safely be resected using the piecemeal-technique.
Endoscopic submucosal dissection (ESD): This relatively new and attractive technique comes from Japan [7]. Theoretically, it allows en-bloc resection of lesions large in diameter in experienced hands. Therefore, ESD promises a lower risk of local recurrence after resection. On the other hand, the risk of complications (bleeding and perforation) is relatively higher than after suck-and-cut ER, and it is a time-consuming technique.
During ESD, the target lesion is circumferentially cut outside it’s borders, and then resected in one piece moving a dedicated endoscopic knife on the level of the submucosa.
In the treatment of early Barrett’s neoplasia, even experienced endoscopists are not able to achieve high complete resection rates using ESD [8]. This derives from the fact that early Barrett’s neoplasia is often very difficult to delineate. It can therefore be stated that suck-and-cut ER should be chosen for ER in early Barrett’s cancer, not at least because of the high complete remission rates that have been reported after suck-and-cut ER.
In early squamous cell cancer, ESD is gaining importance in addition to suck-and-cut ER [9]. Neoplastic lesions can well be delineated using lugol staining, and complete resection rates may therefore be higher.
Endoscopic Ablation
In early Barrett’s neoplasia, thermal ablation of the non-neoplastic remainder of the Barrett’s segment effectively reduces the risk of metachronous neoplasia [1].
There are two mainly used techniques used for this purpose: Argon-plasma coagulation (APC) [1] has been established many years ago, and it can be effectively used especially in small remainders of Barrett’s mucosa at the cardia or in the area of Barrett’s islands in the former Barrett’s segment. Especially for longer Barrett’s segments, the relatively newer technique of radiofrequency ablation (RFA) is very helpful [4]. Most reports have been on RFA during the last years, and RFA is now chosen over APC in most expert centers. The number of treatment sessions required for complete ablation may be lower in comparison with APC, and the ablation effect may be more homogenous. However, no randomized trial comparing RFA to APC has been published so far.
Cryotherapy [5] can also be used for Barrett’s ablation, but there are only few data that have been reported so far, and this technique is mainly used in the U.S.
The new technique of Hybrid-APC which is a combination of submucosal fluid injection prior to ablation and APC promises a very low risk of side effects [10]. However, no clinical studies have been published on Hybrid-APC so far, and there are ongoing studies to evaluate it’s clinical effects in Europe.
References
- Manner H, Rabenstein T, Pech O, Braun K, May A, et al. (2014) Ablation of residual Barrett's epithelium after endoscopic resection: a randomized long-term follow-up study of argon plasma coagulation vs. surveillance (APE study).Endoscopy 46: 6-12.
- Ell C, May A, Gossner L, Pech O, Günter E, et al. (2000) Endoscopic mucosal resection of early cancer and high-grade dysplasia in Barrett's esophagus.Gastroenterology 118: 670-677.
- Pech O, May A, Manner H, Behrens A, Pohl J, et al. (2014) Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus.Gastroenterology 146: 652-660.
- Orman ES, Li N, Shaheen NJ (2013) Efficacy and durability of radiofrequency ablation for Barrett's Esophagus: systematic review and meta-analysis.ClinGastroenterolHepatol 11: 1245-1255.
- Shaheen NJ, Greenwald BD, Peery AF, Dumot JA, Nishioka NS, et al. (2010) Safety and efficacy of endoscopic spray cryotherapy for Barrett's esophagus with high-grade dysplasia.GastrointestEndosc 71: 680-685.
- Manner H, Pech O, Heldmann Y, May A, Pohl J, et al. (2013) Efficacy, safety, and long-term results of endoscopic treatment for early stage adenocarcinoma of the esophagus with low-risk sm1 invasion.ClinGastroenterolHepatol 11: 630-635.
- Oyama T (2014) Esophageal ESD: technique and prevention of complications.GastrointestEndoscClin N Am 24: 201-212.
- Neuhaus H, Terheggen G, Rutz EM, Vieth M, Schumacher B (2012) Endoscopic submucosal dissection plus radiofrequency ablation of neoplastic Barrett's esophagus.Endoscopy 44: 1105-1113.
- Repici A, Hassan C, Carlino A, Pagano N, Zullo A, et al. (2010). Endoscopic submucosal dissection in patients with early esophageal squamous cell carcinoma: results from a prospective Western series. GastrointestEndosc 71: 715-721.
- Manner H, Neugebauer A, Scharpf M, (2014). The tissue effect of argon-plasma coagulation with prior submucosal injection (Hybrid-APC) versus standard APC: A randomized ex-vivo study. United European Gastroenterol. J.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14232
- [From(publication date):
August-2014 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 9548
- PDF downloads : 4684